-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
p-ISSN: 2332-8355 e-ISSN: 2332-8371
2017; 5(3): 57-61
doi:10.5923/j.ijcp.20170503.02

The Effectiveness of Sodium Divalproate as an Adjuvant Therapy on the Improvement of Paranoid Schizophrenic Patients Receiving Haloperidol
Sukmawaty Machmud, Theodorus Singara, Nur Aeni M. A. Fattah
Department of Psychiatry, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia
Correspondence to: Sukmawaty Machmud, Department of Psychiatry, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Schizophrenia is a severe mental disorder that is a disease in the field of psychiatry. The aim of the research was to determine the effectiveness of sodium divalproate as adjuvant therapy on the improvement of paranoid schizophrenic patients given haloperidol. The research was an experimental study with a total number of 30 paranoid schizophrenic inpatients in RSKD of South Sulawesi Province. They were divided into control group who were only given haloperidol antipsychotics consisting of 15 patients and adjuvant therapy group consisting of 15 patients given haloperidol therapy and sodium valproate. Therapy response was assessed through positive PANSS score at the beginning of therapy, i.e. the first week of therapy and the second week of therapy. The data were analysed using statistical analysis. The results of the research indicate that there is no significant different value of the improvement of recurrent positive symptoms of paranoid schizophrenic between the control group and the adjuvant therapy group. Nevertheless, the adjuvant therapy group of sodium divalproate appears to have a better symptom improvement especially at the beginning of therapy, which means that this group more rapidly experiences clinical response than the control group.
Keywords: Paranoid schizophrenia, Haloperidol antipsychotics, Divalproate, Positive symptoms
Cite this paper: Sukmawaty Machmud, Theodorus Singara, Nur Aeni M. A. Fattah, The Effectiveness of Sodium Divalproate as an Adjuvant Therapy on the Improvement of Paranoid Schizophrenic Patients Receiving Haloperidol, International Journal of Clinical Psychiatry, Vol. 5 No. 3, 2017, pp. 57-61. doi: 10.5923/j.ijcp.20170503.02.
Article Outline
1. Introduction
- Schizophrenia is a severe mental disorder that is a disease in the field of psychiatry. This disease appears 1.4 times more common among men than women and usually occurs earlier among men (Smith et al. 2010). A total of 1.7 million visits to the emergency room per year involve patients with positive symptoms and 20% - 50% of emergency psychiatric visits in the United States involve patients at risk of showing positive symptoms of schizophrenia. Schizophrenia (as many as 27%) and bipolar disorder generally show positive symptoms. Positive symptoms in schizophrenic patients or bipolar disorder can be accelerated or aggravated by factors such as men, younger age, history of substance abuse, non-adherence using antipsychotics (Sadock et al., 2013). Most schizophrenic patients, exhibiting some acute episodes with positive symptoms requiring hospitalization during the course of their illness, and nearly 20% of these patients require treatment for their positive symptoms. Patients with positive symptoms associated with paranoid schizophrenia at risk of harming themselves or others and thus require medication to control the symptoms quickly (Sadock et al., 2013). There are five subtypes of schizophrenia, namely: Paranoid Schizophrenia, disorganized schizophrenia, catatonic schizophrenia, undifferentiated schizophrenia and residual schizophrenia. The main antipsychotic drug most commonly used for the treatment of paranoid schizophrenia is a typical class antipsychotic, ie haloperidol with a maximum dose of 30 mg / day. Haloperidol is the most important drug in the management of all types of schizophrenia (Tjay & Rahardja, 2007). The reason for the use of haloperidol because of the cost efficacy spent in the use of atypical antipsychotic combinations is higher than haloperidol, because the cost of atypical oral units is much more expensive than the typical oral unit price of haloperidol and this is also the result of longer lengths of hospitalization at the use of atypical compared with typical antipsychotic use. The existence of evidence of schizophrenia with antipsychotics using the basic hypothesis of dopamine is less relevant. The evidence shows the core symptoms of paranoid schizophrenia in the form of positive symptoms, did not respond well to antipsychotics that are antagonistic dopamine. This evidence has led to the allegation that the core symptoms are not related to dopamine activity alone. Therefore, the dopamine hypothesis revised to include other neurotransmitters, such as serotonin, glutamate and Gamma Amino butyric Acid (GABA) which interact so that people suffering from schizophrenia (Amir, 2009). Lately, a lot of research on schizophrenia drugs are one class of drugs mood stabilizers. Mood stabilizers is now becoming one of the keys of the therapy of patients with schizophrenia who are not able to overcome only with the administration of antipsychotic alone. Internationally today the addition of many therapies including mood stabilizers in patients with schizophrenia as adjuvant therapy (Kang et al., 2011). Additional drugs may be used to reduce symptoms and complaints such as aggressiveness or positive symptoms in schizophrenia paranoid (Murray et al., 2008). One case report from India. A man, unmarried, age 30 years, weight 62 kg, since 2007, with the main complaint auditory hallucinations and ideas of reference, experience withdrawal and suffered impairment in their daily work. Patients have no history of mood disorders. The patient was diagnosed with paranoid schizophrenia. Given risperidone therapy 8 mg / day in divided doses and 80mg / day of fluoxetine in divided doses. This therapy gives good response in improving patient impairment in working as machinery. But the hallucinations of his auditory hallucinations did not stop, the voices always criticizing him. Then the psychiatrist tried to be given sodium divalproate as adjuvant therapy with antipsychotics and antidepressants with the same dose as before. Patients were given sodium divalproate at a dose of 1700 mg / day in divided doses. Auditory hallucinations result is reduced to 75% of patients with PANSS score 2 and 3 (mild symptoms) the item P3 / hallucinations. Previous work by Ping-Tao et al (2016), which is a meta-analysis study from Taiwan conducted in August 2016 using BPRS and PANSS scale. The study involved as many as 889 showing positive symptoms. A total of 436 schizophrenic patients were given haloperidol or risperidone therapy with valproate addition and 453 were given antipsychotics (given haloperidol or risperidone randomly) alone. The result is a significant psychopathological improvement than only antipsychotics alone. Based on this background, the study aims to know the effectiveness of Sodium Divalproate as adjuvant therapy for the improvement of symptoms of paranoid schizophrenia given haloperidol.
2. Materials and Methods
2.1. Location and Time Research
- The study was conducted at the Emergency Unit (ER) and inpatient (ward) of the Regional Special Hospital (RSKD) of South Sulawesi, during August 2017.
2.2. Design and Research Variables
- This study is a quasi-experimental design with pre-test design approach post-test with Control Time Series Design. The research variables consist of: the independent variable (typical antipsychotic and mood stabilizer), the dependent variable (improvement of positive symptoms of paranoid schizophrenia), intermediate variable (brain neurotransmitter imbalances), and the control variables (education, age and length of therapy).
2.3. Population and Sample
- The study population was all patients diagnosed with paranoid schizophrenia are repeated. The samples in this study were all patients of paranoid schizophrenia who showed positive symptoms and have repeatedly admitted to RSKD South Sulawesi that meet the criteria of inclusion and exclusion.
2.4. Method of Collecting Data
- Every paranoid schizophrenic patients who met the inclusion criteria in the study group, will be recorded identity. Explain to the patient's family the intent and purpose of the study. The subjects were subdivided into two groups, namely the group given adjuvant sodium divalproate and haloperidol therapy with a group given only haloperidol, which was the control group. PANSS measure early before the study in each group in the inpatient ward RSKD. Re-measured PANSS values in each group, after 1 week and 2 weeks of therapy. Perform processing and statistical data analysis with computerized system.
2.5. Data Analysis Technique
- Perform data processing and statistical data analysis, using a paired t test and independent sample t test group receiving adjuvant therapy with sodium divalproate control group.
2.6. Ethics Approval
- The ethics committee of Hasanuddin University, Makassar, Indonesia, for health related studies have approved the protocol of this study (registered number: No. 593/H4.8.4.5.31/PP36-KOMETIK/2017).
3. Results
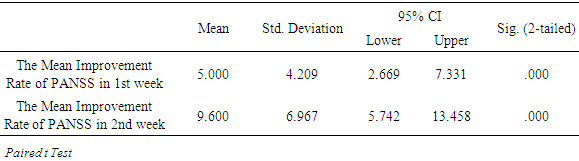
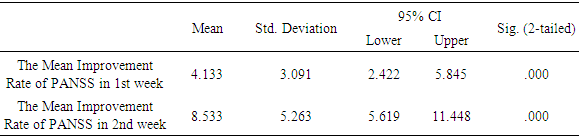
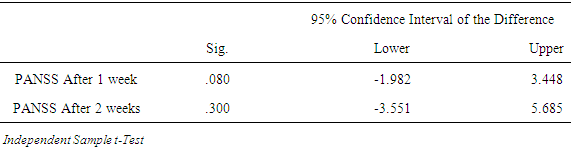
- Studies have been conducted quasi-experimental design with pre-test design approach post-test with Control Time Series Design for examine the effectiveness of Sodium Divalproate as adjunctive therapy to improving the symptoms of paranoid schizophrenia who were given haloperidol. The study was conducted in the hospital ward of Regional Psychiatric Hospital of South Sulawesi Procince from August 7 to August 21, 2017. At the end of the study, the total number of samples were 30 people who fulfilled the inclusion criteria, divided into two groups of samples: control group counted 15 people and 15 persons of adjuvant control group. The sample group was divided into two groups, who received adjuvant sodium divalproate therapy 250 mg / 8 hours / day and haloperidol 5 mg / 8 hours / day and the group received only haloperidol 5 mg / 8 hours / day, which was the control group. Positive and Negative Syndrome Scale (PANSS) used only a positive scale to measure both groups of samples. Data distribution was tested by Saphiro Wilk test because of the number of samples in the small primary data. Total Preliminary PANSS was the total number of PANSS prior to the study in both groups. Total PANSS Week I was the total number of PANSS after one week of therapy in both groups. Total PANSS Week II was the total number of PANSS after two weeks of therapy in both groups. Initial PANSS Difference and Week I is the number of differences between Total PANSS week I against Total Preliminary PANSS in both sample groups. The preliminary PANSS and Week II Difference is the difference between total PANSS week II against Total Beginning PANSS in both sample groups. Each group has a value of P> 0.05, then it says the variable in the data is normally distributed. Therefore test paired t test comparisons for the first week to the second week to find out the average difference in the two groups of samples. P value <0.05 for the first week and second week in the control group then the results were statistically significant (Table 1). P <0.05 for the first and second weeks of the adjuvant therapy group can be said to be statistically significant (Table 2).
|
|
|
4. Discussion
- This study showed that there was no difference in the value of meaningful significance between improved positive symptoms of paranoid schizophrenia who repeatedly between the control group and the group of adjuvant therapy. Nevertheless, the adjuvant sodium divalproate therapy group appears to have improved symptom improvement, especially in therapeutic initiation which means that this group is more rapidly experiencing a clinical response than the control group.This study was conducted to compare the improvement of positive symptoms in schizophrenia paranoid patients given adjuvant therapy with sodium divalproate and haloperidol were given haloperidol, which is a control group based on the PANSS (Positive and Negative Syndrome Scale) Positive consisting of seven items. By paying attention to the variables of sex, age, education level, occupation and marital status, the primary data obtained p value> 0.05, so it concluded that based on these variables is normally distributed to the number of entire sample population. The proportion of sex of the research sample is male more than female that is male counted 24 people (80%) and female counted 6 people (20%). This is in accordance with Kaplan & Sadock (2007), that more than half of all patients with schizophrenia who were hospitalized were male and one-third are women in general, the final results for the treatment of schizophrenia in women is better than the final outcome of schizophrenic patients in male, in this case the schizophrenia in male tended to relapse or recur. One factor that supports fewer women and the end result of schizophrenia is better in women than men because the female hormone estrogen can regulate the dopamine system. Estrogen can prevent the increase in dopamine that occurs in schizophrenic patients or considered estrogen as a protectorate against schizophrenia (Lindamer et al. 2010). Based on the characteristics of the age of the study sample, the age group 31-40 years were 12 people (40.0%), then the age group of 20-30 years were 10 people (33.3%) and the age group 41-50 years were 8 26.6%). The characteristics are in line with the opinion that a picture psychotic schizophrenia typically emerge in late adolescence and the mid age of 30 years. The first episodes of psychotics often appear in men in their early 20s while in late 20s women. Onset of schizophrenia at the age below 10 years and above 60 years of very ja rang occur (Sadock et al., 2013). Schizophrenia is also associated with educational level. A low level of education will further exacerbate the prognosis of schizophrenia. In this study, it was obtained for elementary school education as many as 7 people (23.3%), junior high level as many as 10 people (33.3%), high school level 12 people (40.0%) and S1 as many as 1 person (3.3 %%). The data shows that most of the sample are at elementary and junior high school level. The lower the education level of a person, the less the ability to process stress in his life. Education level is indirectly related to work. With a low level of education it will be difficult for someone to get a job. According to the data of this study, it appears that the sample did not work as many as 17 people (56.7%) and who worked 13 people (43.3%). With no one working then the level of the economy will also be low, earned income will not be able meet the needs of families, especially for those who have been married. So from the sample looks the number of samples who married 17 people (56.7%) and not married 13 people (43.4%). One of the high and stressful stressor factors is the economic problem. Based on the data it can be seen that improvement in PANSS positive score after the first week of therapy p value = 0.08, and after a second week p value = 0.3. This value results obtained from comparative testing with independent testing T test between the two groups of samples. From this comparison test showed no meaningful for each value of p> 0.05. This suggests that in the first week the addition of sodium divalproate therapy is good enough to result in the addition of sodium divalproate therapy after the second week. Thus suggesting that the addition of sodium divalproate may make positive PANSS better in week I than in subsequent therapy. This is in line with research conducted by Ping-Tao et al (201 6), in patients with schizophrenia who received additional therapy besides sodium divalproate antipsychotic as the main drug. This study used a sample of 889 schizophrenic patients who received antipsychotic monotherapy haloperidol or risperidon. A total of 436 patients received adjuvant therapy sodium divalproate and antipsychotic monotherapy and as many as 453 patients who only received monotherapy. The results of the study were significant improvements in the use of valproate at the beginning of therapy, in terms of lowering the symptoms of hostility and aggression. Treatment with adjuvant therapy is more significant at the beginning of therapy compared with treatment for a long time. From the results of these studies reported that among all subtypes of schizophrenia, paranoid schizophrenia that provides significant improvements result in adjuvant therapy sodium divalproate than other subtypes of schizophrenia. The addition of sodium divalproate is beneficial in therapy in week I because divodropproate sodium works increase plasma / serum concentrations of antipsychotics, in it is haloperidol so that the work of haloperidol is stronger than if haloperidol is administered as monotherapy. Sodium divalproate primarily works to reduce glutamate excitation. Glutamate is the major excitatory neurotransmitter that excites neurons in the brain (master swcith). By reducing sodium influx into neuronal cells (Stahl, 2013), cause a reduction in the glutamate excitation of neuronal cells, especially so that the positive symptoms will be reduced. Sodium divalproate work involved inhibits dopamine through the release of GABA, through a mechanism of increasing output and reducing reuptake slow the inactivation of GABA and GABA in GABA ergic cells. GABA is a neurotransmitter that blocks the brain. The work of adjuvant sodium divalproate therapy is only in the first week of therapy or is only beneficial in the beginning of therapy because of the relatively constant internal static state of the body against the various stimuli that cause each specific neuronal cell to always maintain homeostasis. So if the neuronal cells have become homoestatis of sodium ions, then the role of sodium divalproate to reduce the sodium ion influx is no longer needed. Limitations of this study is the lack of the number of samples and a short observation period, so it cannot determine the effect of adjuvant therapy and side effects of sodium divalproate the next therapy phase.
5. Conclusions and Recommendations
- The researchers concluded that there was no significant difference between the recovered positive symptoms of paranoid schizophrenia between the haloperidol-treated groups who were the control group with the group receiving adjuvant sodium divalproate therapy against haloperidol. Patients with recurrent paranoid schizophrenia who receive adjuvant sodium divalproate are seen to have improved symptoms better than recurrent paranoid schizophrenics who did not receive adjuvant sodium divalproate, especially in the first week. Paranoid schizophrenic patients who get adjuvant sodium divalproate more quickly experience a clinical response than patients with paranoid schizophrenia. The adjuvant sodium divalproate therapy is useful for the treatment in the first week. Researchers suggest so that the use of sodium divalproate as adjuvant therapy may be a consideration for the accelerated improvement of symptoms in recurrent paranoid schizophrenic patients. Need to do further research with a larger sample size and more diverse antipsychotic control, using different assessment instruments, with a double-blind randomized design (randomized double blind controlled trials) and studies in other educational centers (multicenter).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML