-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
p-ISSN: 2332-8355 e-ISSN: 2332-8371
2017; 5(2): 32-38
doi:10.5923/j.ijcp.20170502.02

Obesity and Pattern of Use of Antipsychotic Agents among Outpatients with Schizophrenia in Nigeria
Maroh Ighoroje1, Adefolakemi Ogundele1, Olukayode Abayomi2
1Neuropsychiatric Hospital, Aro, Abeokuta, Nigeria
2Department of Psychiatry, Ladoke Akintola University Teaching Hospital, Ogbomoso, Nigeria
Correspondence to: Maroh Ighoroje, Neuropsychiatric Hospital, Aro, Abeokuta, Nigeria.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: This study aims to estimate the rate of obesity in outpatients with schizophrenia and to determine the association between Body Mass Index (BMI) and the pattern of use of antipsychotic agents (type or class of drug, dosage, duration of use, and use of depot antipsychotics). Methods: The design was cross-sectional. One hundred and fifty subjects diagnosed with schizophrenia and attending the outpatient clinic of the Neuropsychiatric Hospital, Abeokuta, Nigeria participated. Their current anthropometric values (weight, height and waist circumference) were measured. BMI prior to commencement of medications and pattern of use of antipsychotic agents were obtained from their records. The associations between current BMI, patient’s characteristics and pattern of use of antipsychotics were analyzed using Chi Square test (P < 0.05). Results: The rate of obesity, overweight and elevated blood pressure were 7.3%, 33.3% and 14.0% respectively. More females, younger respondents and hypertensive persons were obese. These associations were statistically significant. There was no association between BMI and pattern of antipsychotic use.Conclusions: There is a need to raise the awareness of the mental health worker, to the extent of obesity and the need to routinely screen patients on antipsychotic medications for this and other metabolic risk factors.
Keywords: Obesity, Antipsychotics, Schizophrenia, Nigeria
Cite this paper: Maroh Ighoroje, Adefolakemi Ogundele, Olukayode Abayomi, Obesity and Pattern of Use of Antipsychotic Agents among Outpatients with Schizophrenia in Nigeria, International Journal of Clinical Psychiatry, Vol. 5 No. 2, 2017, pp. 32-38. doi: 10.5923/j.ijcp.20170502.02.
Article Outline
1. Introduction
1.1. Background
- Excess body weight is one of the most common physical health problems in patients with schizophrenia [1]. The rate of obesity in patients with schizophrenia on antipsychotic agents has ranged from 5% in studies done in low and medium income countries to over 50% in the developed world [2-5]. Obesity in patients with severe mental illness has been attributed to an unhealthy lifestyle, poverty, a familiar and personal genetic profile, limited access to medical care, and the use of antipsychotic agents [6]. Obesity as measured by an elevated body mass index (BMI ≥ 30Kg/M2) and waist circumference (WC > 102cm for men; > 88cm for women) has been identified as the most prevalent factor in metabolic syndrome [7]. In addition to an elevated risk of cardiovascular disease, type 2 diabetes mellitus, osteoarthritis and gallbladder disease, excessive weight gain contributes to a decreased quality of life, non-compliance with antipsychotic medications, a lowered self-esteem, social withdrawal and increased stigmatization [8-10]. With regards to antipsychotic medications, pharmaco-genomic approaches have detected more than 300 possible candidate genes for antipsychotics-induced body weight gain [1]. In addition, antipsychotic treatment may contribute to obesity by increasing appetite [11]. In relation to its extrapyramidal side-effects profile, the ‘newer’ generation atypical antipsychotics represent a substantial improvement on ‘older’ typical drugs. However, clinical experience and epidemiological studies have shown that some of the atypical antipsychotics (e.g. clozapine and olanzapine) can induce substantial weight gain and cause metabolic disturbances [1, 12]. This important effect may be related to the histamine and serotonin (5HT2C) receptor blocking effects of antipsychotics and a genetic variation at the 5HT2C [13]. Although, the literature has shown that overweight and obesity is common in patients with schizophrenia, the rate of these conditions in Nigeria is yet to be thoroughly studied. To the best of our knowledge, the rate of obesity in persons with schizophrenia is unknown in our environment. This study aims to bridge this gap and add to the existing body of knowledge concerning obesity among patients with schizophrenia on antipsychotic treatment, especially as it relates to the Nigerian environment.
1.2. Aims of the Study
- To estimate the rate of obesity and overweight in outpatients with schizophrenia in Abeokuta, Nigeria, and to determine the association between obesity and the pattern of use of antipsychotic agents (type or class of drug, dosage, duration of use, and use of depot antipsychotics).
2. Material and Methods
- The study’s design was cross-sectional. It was carried out at the outpatient clinic of the Neuropsychiatric Hospital, Aro, Abeokuta, South-west Nigeria. The hospital was established in 1954 and has a total bed capacity of 546 for inpatient care. It has an assessment/emergency unit that provides 24 hours first contact and emergency services, all days of the week. The outpatient clinics are run for follow-up consultations on Mondays, Tuesdays, Thursdays and Fridays after the first contact at the assessment unit or following discharge from in-patient care. About 2000 patients are seen at the outpatient clinic every month. There are about 16 clinic days (4 days per week) in a month and about 60-70% of the patients regularly seen at the adult clinic are been managed for schizophrenia [14]. A sample size of 161 was calculated using the Leslie Kish’s formula [15]. Based on case note records, respondents between 18 and 64 years of age, who met the International Classification of Disease (ICD-10) criteria for Schizophrenia (F20), had been complaint on antipsychotic medications for the past 12 months without default and had no history of hypertension, diabetes or any other chronic medical condition prior to commencement of antipsychotics were screened and randomly selected to participate in the study.A questionnaire drawn up by the researchers was used to elicit basic socio-demographic characteristics, current anthropometric values (weight, height and waist circumference), current systolic and diastolic blood pressure, and clinical characteristics such as illness and medication history. The patient’s blood pressure and weight prior to commencement of antipsychotics were obtained from the case notes. Obesity was defined as a body mass index (BMI) of 30 and above. The BMI, a key index for relating body weight to height, is a person's weight in kilograms (kg) divided by their height in meters (m) squared [16]. Elevated blood pressure was defined as a systolic blood pressure (SBP) of 140 mm Hg or more, or a diastolic blood pressure (DBP) of 90 mm Hg or more, or the taking of antihypertensive medications [16]. The psychotic module of the Mini International Neuropsychiatric Interview (M.I.N.I) was used to confirm the diagnosis of schizophrenia in the respondents. The M.I.N.I is a structured diagnostic interview, developed in 1990 by psychiatrists and clinicians in the United States and Europe, for DSM-III-R/IV and ICD-10 psychiatric disorders [17]. It requires only ‘yes’ and ‘no’ answers. It is divided into modules identified by letters corresponding to 17 diagnostic categories. For each disorder, one or two screening questions rule out the diagnosis when answered negatively. Ethical approval was obtained from the Research and Ethics Committee of the Neuropsychiatry Hospital, Aro, Abeokuta, Ogun State. The purpose of the study was explained to the respondents. They were assured of confidentiality and signed an informed consent form. The interview was conducted, at the reception room of the adult outpatient clinic of the hospital. The study’s participants were recruited over a 3 month period (July – September 2016).The statistical package for social sciences (SPSS) version 21 for windows was used for analysis of data. The socio-demographic and clinical variables of the respondents were presented using descriptive statistics frequencies and percentages. The means and standard deviations were calculated as applicable. The rate of obesity was presented categorically, using frequency distribution tables and percentages. The associations between BMI, patient’s characteristics and pattern of use of antipsychotics were analyzed using Chi Square test. The level of significance was set at < 0.05.
3. Results
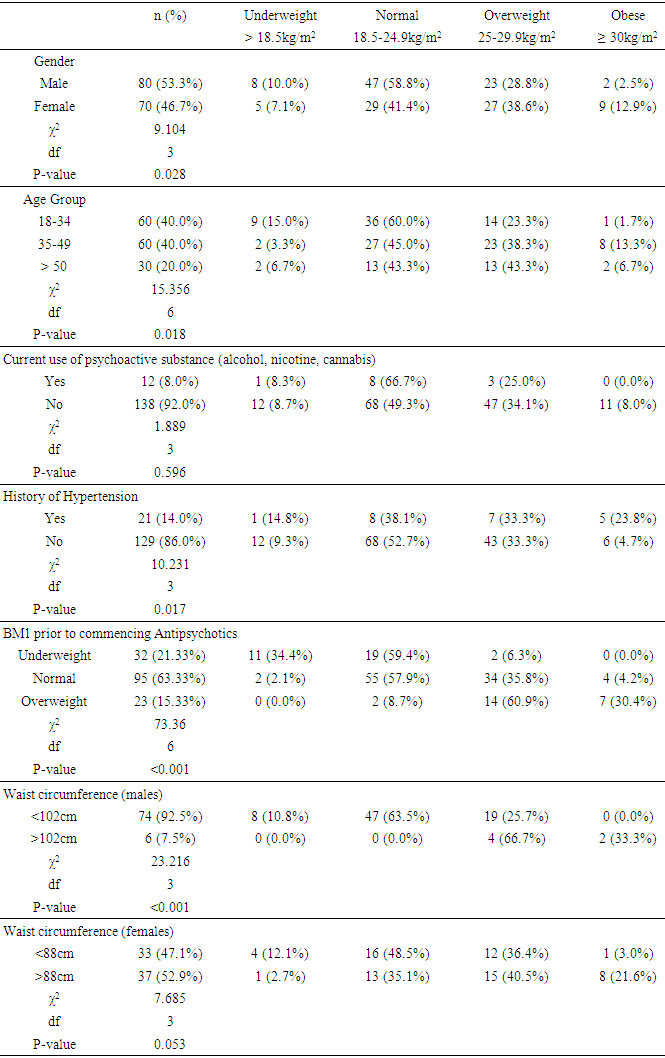
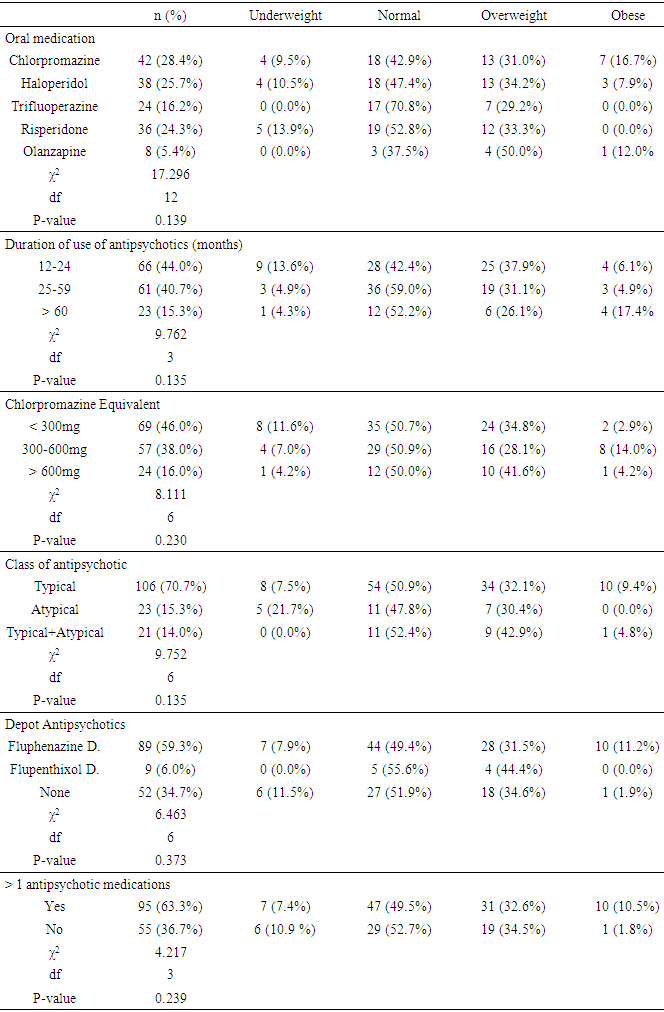
- A total of 150 outpatients participated in the study. They all met the diagnostic criteria for schizophrenia, and had been duly compliant with antipsychotic medications and clinical visits for the past 1 year. The majority of the respondents were males (53.3%), and most (80%) where less than 50 years of age. The mean age of the participants was 39.10 ± 11.18 SD years. Eleven subjects (7.3%) were obese (BMI > 30kg/m2). The case note records showed that 23 subjects (15.3%) had an overweight BMI prior to the commencement of treatment. However 33.3% were currently overweight. Six (7.5%) of the males and 37 (52.9%) of the females had an increased waist circumference. Over 90% of the obese individuals had an at-risk waist circumference. Twenty one (14%) respondents had an elevated blood pressure or were on anti-hypertensive drugs. Only 12 (8%) persons had a lifetime history of use of psychoactive substances (alcohol, nicotine and cannabis). Most of the patients had used medications continuously for 12-24 months, and were on a typical, 1st generation antipsychotics – Chlorpromazine, Haloperidol and Trifluoperazine (70.7%). Two-third of the respondents were currently using more than one medication, while 65.3% were on a depot (fluphenazine decanaote or flupenthixol decanaote). Tables 1 and 2.
|
|
4. Discussion
- The rate of obesity of 7.3% reported among patients with schizophrenia on antipsychotics is quite similar to results from developing countries as Ghana (5.91%) and Indonesia (5.0%) [5, 18]. But compared with findings from high income countries such as the United-Kingdom (47%), Australia (59%), Sweden (37%) and Japan (31%), the rate of obesity in this study is rather low [19-22]. The value is also lower than the rate of obesity in the general Nigerian adult population (8.1-22.2%) [23]. Brown et al. and Roick et al. noted that psychiatric patients in western societies smoke cigarettes more frequently, exercise less often, snack regularly and eat more meals high in fat and low in calories than non-psychiatric patients [24, 25]. Besides, the high rate of use of weight inducing atypical antipsychotic drugs such as olanzapine, clozapine and risperidone contributes to the problem in advanced countries [12]. These factors may not readily apply in poorer countries like Nigeria. Unlike developed countries, there are no national social welfare and rehabilitation programmes for the mentally ill. Patients and families bear the major burden of care and struggle financially to eat regular meals and buy their medications [26]. In this study, over 70% of the patients were on the cheaper 1st generation antipsychotics (chlorpromazine, haloperidol and trifluoperazine), which compared to the more expensive newer antipsychotics (olanzapine and risperidone), had a lower risk of inducing obesity and metabolic syndrome. In addition, only 8% of the respondents in this study reported a current use of psychoactive substances (cannabis, cigarettes and alcohol). We reported more females being overweight and obese than males. More females (57.9%) also reported having an at-risk waist circumference. Similar findings have been reported in other studies [27, 28]. Mc Eloy et al. suggested that the gender difference and the higher rate of overweight and obesity in women may be due to important interactions of gender with many factors that influence body fat and fat distribution [29]. In addition to antipsychotic medications, weight gain in females may be precipitated by events such as pregnancy, oral contraceptives therapy and menopause [30-32]. In this study, 82% of all cases of overweight, obesity and hypertension occurred in patients between 18 and 50 years of age. Gorczynski noted that patients with schizophrenia appear to develop physical illnesses and cardiovascular diseases at a younger age than the general population [33]. Many investigators have reported that excess morbidity and mortality in schizophrenia is highest in the young and generally decreases with age [29, 34]. Additionally, patients with schizophrenia are rarely treated for physical illnesses in the early, less severe phases and appear for medical attention only when cardiovascular and pulmonary diseases are severe and potentially life-threatening [29, 35].Over 90% of the obese individuals in this study also had an at-risk waist circumference. A recent meta-analysis of 77 studies reported that at-risk waist size is most useful in predicting high rates of metabolic syndrome with a sensitivity of 79.4% and a specificity of 78.8% [7]. Bell et al. identified obesity and at-risk waist circumference as the most prevalent factors in metabolic syndrome [36]. Although the Body Mass Index increased significantly with antipsychotic use, there was no significant association between BMI and the pattern of use of antipsychotics (type or class of drug, dosage, duration of use, and use of depot antipsychotics). Similar to these findings, Jerrell et al in their study reported that the odds of developing obesity/excessive weight gain, was not significantly related to any specific atypical agent compared to haloperidol [37]. Prior to the discovery of the atypical drugs, low potency first generation antipsychotics such as chlorpromazine and thioridazine have long been known for their weight gain potential [38]. However, findings from clinical experience and epidemiological studies shows that atypical antipsychotics (especially, clozapine, olanzapine, risperidone and quetiapine) can induce substantial weight gain and cause metabolic disturbances [39, 40].
4.1. Strengths and Limitations
- To the best of our knowledge this is the 1st study examining overweight, obesity and use of antipsychotic medications among patients with schizophrenia in Nigeria. This would provide guidance for discussions and future research on the subject. The limitations of the study include its cross-sectional design and the retrospective analysis of patient’s records. This may have introduced some bias. A longitudinal approach in which respondents are systematically followed up from first appointment would be most ideal. Secondly, other metabolic risk factors such as diabetes mellitus and dyslipidemia were not measured. In addition, likely confounders (such as nutritional status, sedentariness and use of other medications such as anticholinergic agents, antihypertensives and oral contraceptive therapy) were not accounted for.
5. Conclusions
- There is a need to raise the awareness of the mental health worker, to the extent of obesity and the need to routinely screen patients on antipsychotic medications for this and other metabolic risk factors. In addition, there is the need of developing a policy framework for the active management of these diseases in patients with schizophrenia in Nigeria.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML