-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
p-ISSN: 2332-8355 e-ISSN: 2332-8371
2017; 5(2): 25-31
doi:10.5923/j.ijcp.20170502.01

Insomnia and Dysfunctional Beliefs and Attitudes about Sleep among Elderly Persons in Abeokuta, Nigeria
Adefolakemi Ogundele 1, Maroh Ighoroje 1, Olukayode Abayomi 2
1Neuropsychiatric Hospital, Abeokuta, Nigeria
2Department of Psychiatry, Ladoke Akintola University Teaching Hospital, Ogbomoso, Nigeria
Correspondence to: Maroh Ighoroje , Neuropsychiatric Hospital, Abeokuta, Nigeria.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: Insomnia is a common health complaint among the elderly. Sleep problems in this group are often accompanied by maladaptive sleep-related cognitions. However the relationship between dysfunctional beliefs and attitudes about sleep to insomnia and depression in the elderly has not been explored in this environment. Methods: It was a cross sectional study carried out among 212 elderly persons in the community. Individuals with a past history of mental illness were excluded. Respondents were administered the Dysfunctional Beliefs and Attitudes about Sleep Questionnaire (DBAS-16), Insomnia Severity Index (ISI) questionnaire, the Geriatric Depression Scale (GDS). Results: The mean age of respondents were 70.1±7.1 years, 81.6% were males, 23.6% used medication to aid sleep, while 16.0% slept for < 4 hours per night. Insomnia and depressive symptoms were present in 53.3% and 23.6% of the respondents respectively. Presence of insomnia (t = 5.19, df = 210, p < 0.001), depressive symptomatology (t = 2.52, df =210, p = 0.013) and use of medication to aid sleep (t = 2.436, df = 210, p = 0.016) was significantly associated higher total DBAS scores. The multiple linear regression showed that the presence of insomnia (p < 0.001, ß = 21.93) was the most significant predictor variable of dysfunctional beliefs and attitude about sleep. Conclusions: Faulty sleep beliefs are present among the elderly in Nigeria and may be driven by poor sleep. The clinical implication is that these cognitions should be identified and modified in the management of insomnia in this age group.
Keywords: Dysfunctional beliefs and attitudes about sleep, Insomnia, Depression, Elderly, Nigeria
Cite this paper: Adefolakemi Ogundele , Maroh Ighoroje , Olukayode Abayomi , Insomnia and Dysfunctional Beliefs and Attitudes about Sleep among Elderly Persons in Abeokuta, Nigeria, International Journal of Clinical Psychiatry, Vol. 5 No. 2, 2017, pp. 25-31. doi: 10.5923/j.ijcp.20170502.01.
Article Outline
1. Introduction
1.1. Background
- Insomnia is a common health complaint among elderly people. It has been estimated to affect between 25-30% of the older population [1, 2]. The diagnostic and statistical manual of mental disorders, 5th Edition, defines insomnia as a predominant complaint of dissatisfaction with sleep quantity or quality, along with difficulty initiating or maintaining sleep, which causes clinically significant distress or impairment in important areas of functioning (i.e., social, occupational, behavioral, etc.) [3]. Negative consequences of insomnia in late life include decreased quality of life, high risk for heart diseases, high risk of falls, increased psychological difficulties, increased economic and social costs, increase use and abuse of tranquilizers and mortality [4].Often sleep problems in the older age groups are precipitated and maintained by maladaptive sleep-related cognitions (e.g., faulty beliefs and appraisals, unrealistic expectations and perceptual bias) [5, 6]. Dysfunctional beliefs associated with worry about the negative consequences of insomnia and hopelessness about the fear of losing control over sleep have been identified as the most critical factors in differentiating chronic insomnia from transient insomnia [7]. These dysfunctional sleep-related cognitions may be influenced by the presence of physical and psychological disorders such as chronic pain and mood disorders [8, 9]. The importance of targeting sleep-related beliefs and attitudes in the treatment of insomnia is highlighted by the fact that more adaptive beliefs and attitudes about sleep following treatment are associated with better maintenance of sleep improvements at follow-ups [6, 10].
1.2. Rationale
- Previous studies on sleep disorders have been conducted among the elderly population in Nigeria [2, 11, 12]. But these were largely limited to profile and prevalence studies. Despite increasing recognition of the importance of cognitive factors in the etiology of insomnia, no past work has investigated the dysfunctional sleep related beliefs and attitudes among the elderly population in this country. This study will fill this dearth of information.
1.3. Aims
- The study aims to examine the dysfunctional beliefs and attitudes about sleep and its relationship to insomnia among elderly persons in Abeokuta, Ogun state, Nigeria.
2. Methods
2.1. Study Population and Sample Size
- The study’s design was cross sectional. It was conducted in Abeokuta, the capital of Ogun state, south western Nigeria. The study population consisted of the over 1000 retired civil servants of the Ogun state civil service who belonged to the Abeokuta chapter of the Nigeria Union of Pensioners. Using the Leslie Kish's formula (n = nf/1+nf/N for a study population less than 10000) and estimating for a 20% non-response a sample size of 268 was estimated.
2.2. Procedure
- The respondents were randomly selected from 450 retirees who regularly attended the association’s meetings held every last Wednesday of the month. The participants were recruited over a consecutive 3 month period (July – September 2016). The study’s inclusion criteria were (a) a minimum of 60 years as at last birthday (b) absence of a severe visual or hearing impairment (c) absence of a previous history of mental illness (d) ability to speak, read and understand English. Ethical approval was obtained from the research and ethical committee of the Neuropsychiatry Hospital, Aro, Abeokuta Ogun State, and permission was obtained from the Nigerian Union of Pensioners, Ogun state, Abeokuta chapter. A written Informed consent was obtained from each subject. The participants completed 3 self-report questionnaires.
2.3. Instruments
2.3.1. Dysfunctional Beliefs and Attitudes about Sleep (DBAS-16)
- The DBAS Scale was used to assess maladaptive cognitions about sleep. Its original version contains 30 items [13]. The 16-Item version is more user-friendly, utilizes a Likert-type response (0–10) and has an adequate internal consistency and convergent validity [5]. Questions on the DBAS-16 fall into four subscales: Consequence – 5, Worry/Helplessness – 6, Expectations – 2 and Medication – 3. The consequence subscale, relate to the subject’s perception of how insomnia affects energy, mood, and overall functioning. The worry/helplessness subscale focuses on perceptions about how worried a subject may be about the unpredictable nature of his/her sleep. The expectations subscale focuses on the belief that one cannot function without eight hours of sleep, and that napping in the day is necessary to catch up on sleep if preceded by a night of insomnia. The medication subscale queries the participant regarding beliefs that insomnia is essentially the result of a chemical imbalance and can only be managed by medications. The average of all 16 questions forms the overall DBAS-16 score, with higher scores indicating a greater degree of maladaptive sleep-related cognitions. [14]. The DBAS Scale has been used in the elderly [5, 15]. Permission to use the questionnaire for this study was sought from the authors.
2.3.2. Insomnia Severity Index (ISI)
- The ISI is a 7-item self-report questionnaire assessing the nature, severity, and impact of insomnia [16]. The ISI has displayed good discriminant validity, content validity, internal consistency and test-retest reliability [16, 17]. The dimensions of sleep evaluated are: severity of sleep onset, sleep maintenance, and early morning awakening problems, sleep dissatisfaction, interference of sleep difficulties with daytime functioning, noticeability of sleep problems by others, and distress caused by the sleep difficulties. The usual recall period is the last month and a 5-point Likert scale is used to rate each item yielding a total score ranging from 0 to 28. The score is interpreted as follows: absence of insomnia (0-7); presence of insomnia (8-28) with subthreshold/mild insomnia (8-14), moderate insomnia (15-21), and severe insomnia (22-28). It has been validated for use in primary care and older adults [18].
2.3.3. Geriatric Depression Scale (GDS)
- The GDS was developed for the screening and evaluation of depression in the older population [19]. The short form consist of a 15-item self-report questionnaire in which participants are asked to respond by answering yes or no in reference to how they felt over the past 2 weeks [20]. Scores of 0-4 are considered normal and 5-15 are depressed (5-8 indicate mild depressive symptoms; 9-11 indicate moderate depressive symptoms; and 12-15 indicate severe depressive symptoms). The GDS has been found to have a 92% sensitivity and 89% specificity when evaluated against diagnostic criteria (ICD or DSM) [20].
2.4. Data Analysis
- Data was analyzed using the statistical package for social sciences (SPSS 21) computer software. The socio-demographic and sleep related characteristics were presented using descriptive statistics frequencies and percentages. The average total DBAS scores and subscale scores were calculated and presented using descriptive statistics determining the mean and standard deviation. The associations between the dysfunctional beliefs and attitudes about sleep, socio-demographic and sleep related variables, insomnia and depression were analyzed using the independent t test. The level of statistical significance was set at < 0.05. Multiple linear regression was done to determine the extent of the relationship between multiple variables and the dysfunctional beliefs and attitudes about sleep.
3. Results
- Of the 268 persons invited, 212 gave written consent and fully participated in the study, giving a response rate of 79.1%. The mean±sd age was 70.14±7.10 (range: 60-93). The majority were males (81.6%) and almost two-third reported having a chronic medical illness (mostly hypertension, osteoarthritis and diabetic mellitus). Thirty four (16%) respondents slept for less than 4 hours per night while 23.6% currently used medications to aid sleep. Sixty persons (29.8%) had a geriatric depressive score of ≥ 5. and were categorized as depressed. One hundred and thirteen (53.3%) had insomnia (ISI ≥ 8), of which 80 (37.7%) had mild insomnia (ISI = 8-14) and 33 (15.6%) had moderate to severe insomnia (ISI = 15-28). See Table 1.The mean±sd scores on the dysfunctional belief and attitude about sleep scale was 4.23±2.45. The bivariate analysis showed no significant association between age groups (60-69 and ≥70 years), gender and average DBAS scores. The presence or absence of a chronic medical illness, and the average hours of night sleep had no influence on mean DBAS scores. The individuals who used medications to aid sleep scored significantly higher than those who didn’t use medications to sleep (t = 2.43, p = 0.016). Respondents who had significant depression symptomatology had higher DBAS scores than those who weren’t depressed (t = 2.52, p = 0.013), There was an association between having insomnia and higher DBAS scores (t = 5.19, p = 0.001). See Table 1.The average DBAS subscale scores of the individuals were consequences (4.38±2.89), helplessness (4.09±2.53), expectation (5.15±3.19) and medication (3.65±2.77). Those who use medications to aid sleep had higher scores on the medication subscales (t = 3.69, p < 0.001). Respondents with insomnia (ISI≥8) had significantly higher scores (p < 0.001) on all DBAS subscales while depressed persons had higher scores on the consequences, helplessness, expectation sub scales. See Table 2.To determine the extent of the relationship between the significant variables (medications to aid sleep, GDS scores and ISI scores) and the dependent variable, average total DBAS Scores, a multiple regression analysis was carried out. The result showed that respondents ISI scores was the most significant predictor of dysfunctional belief and attitude about sleep (p < 0.001, ß = 21.93). See Table 3.
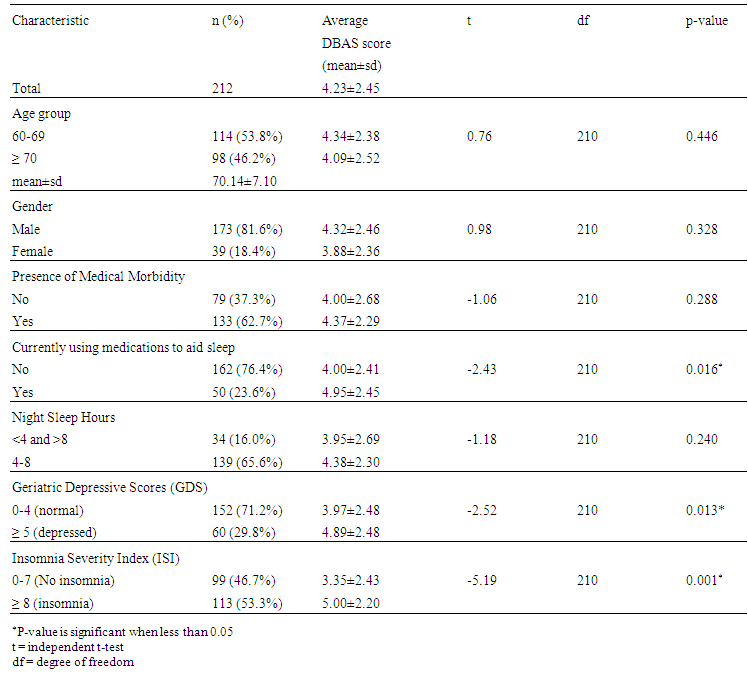 | Table 1. Dysfunctional Beliefs and Attitude about Sleep and Respondent’s Variables |
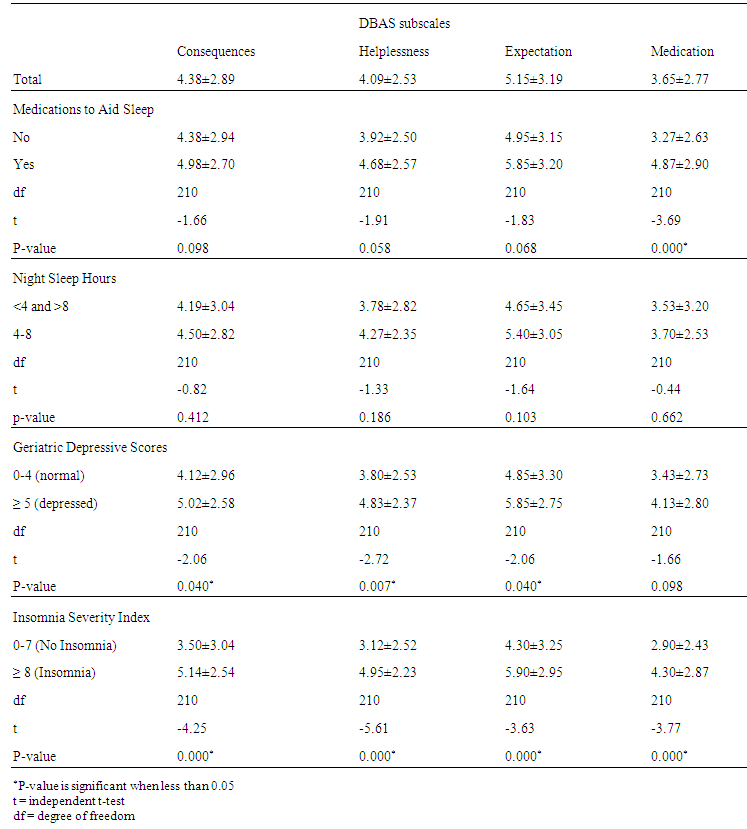 | Table 2. DBAS subscales, depression and sleep variables |
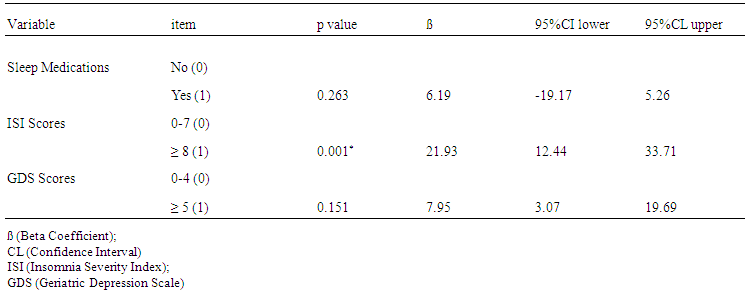 | Table 3. Multiple Linear Regression Predicting Dysfunctional Belief and Attitude about Sleep |
4. Discussion
4.1. Insomnia and DBAS
- More than half of the respondents reported having insomnia, with 15.6% having symptoms of a moderate to severe degree. These rates are high when compared with the 10%-20% prevalence of sleep problems commonly reported in general adult population [21, 22]. Previous studies have also reported a high prevalence and burden of insomnia and other sleep disorders in the elderly population [23, 24]. This study showed that persons with insomnia symptoms have more dysfunctional beliefs and attitudes about sleep than those without sleep problems. These false beliefs includes an exaggeration of the perceived negative consequences of insomnia, excessive worry and helplessness, unrealistic and wrong expectations about sleep and beliefs that medications are necessary to induce and sustain sleep. This supports previous findings that insomnia in this age group is often accompanied and maintained by maladaptive sleep-related cognitions [6, 15]. The association between insomnia and faulty beliefs and attitudes toward sleep remained significant after adjusting for other variables.
4.2. Depression and DBAS
- Respondents with significant depressive symptoms had more faulty beliefs and attitudes about sleep. Dysfunctional sleep related cognitions may be influenced by the presence or absence of psychological disorders as chronic pain, and mood disorders [8-10]. Likewise depressive symptoms may mediate the relationship between insomnia and dysfunctional beliefs an attitudes about sleep [25]. One study noted that dysfunctional beliefs about sleep are positively related to the intensity of suicidal ideations and its effect on insomnia symptoms appears to be mediated through these variables [26].
4.3. Use of Medications and DBAS
- Those who use medications to aid sleep believed that insomnia is essentially the result of a chemical imbalance which can only be managed by medications. Although the use of ‘sleeping pills’ may improve the duration and quality of sleep, they are not sufficient to produce changes in beliefs and attitudes [27]. Instead continuous use may precipitate the wrong beliefs about medications and even account for more frequent insomnia complaints in older people [28].
4.4. Duration of Sleep and DBAS
- Respondents’ average duration of night sleep played no significant role on beliefs and attitudes about sleep. Neither short sleepers (<4 hours) nor adequate (4-8 hours) sleepers differed with regard to DBAS scores. A similar finding had been reported by Pandey et al [29]. This may imply that other measures such as the quality of sleep (ease to falling asleep, sleeping uninterrupted, feeling refreshed upon waking) may be subjectively more important to the elderly than the total sleep time.
4.5. Gender and DBAS
- We found no relationships between faulty sleep beliefs and socio-demographic variables as gender. The literature has consistently demonstrated a higher prevalence rate of insomnia and use of sleep medications in females than males [30, 31]. In our study, an individual’s gender did not significantly lead to more faulty beliefs and attitude about sleep. A similar find was reported by Yang et al in their study of 307 adults in Taipei Taiwan [32]. A meta-analysis of 61 surveys over a 25 year period revealed that gender differences in self-reported sleep maintenance difficulties and early morning awakening were not clear cut [33].
4.6. Clinical Implications
- Our study highlighted that faulty sleep beliefs are present among the elderly in Nigeria and may be driven by poor sleep. They may propagate anxiety, preoccupations and the psychological dependence on sleep medications. These beliefs can act as barriers to the successful utilization of pharmacological and behavioral approaches to managing sleep disorders [34]. The management of insomnia in the community often entails the prescription of hypnotic medications most especially the benzodiazepines and over-the-counter medications [35]. Although they are indicated for short-term symptomatic treatments, their use often becomes chronic and leads to adverse consequences such as chemical dependency, daytime sedation, falls and vehicular accidents [4, 34]. This study showed the importance of identifying and targeting sleep related beliefs and attitudes in the treatment of insomnia. More adaptive beliefs and attitudes about sleep following treatment have been associated with better maintenance of sleep improvements at follow-ups [6]. Behavioral approaches to the management of insomnia includes, sleep hygiene, relaxation, and cognitive behavioral treatments such as sleep restrictions and stimulus control procedures (CBT) [36]. Sleep hygiene refers to a list of behaviors, environmental conditions and other sleep-related factors that can be adjusted as a stand-alone treatment or component of multimodal treatment for patients with insomnia [37]. Edinger et al in a randomized controlled trial showed that CBT (compared with progressive muscle relaxation and a sham behavioural intervention) was most effective for reducing dysfunctional beliefs about sleep and such cognitive changes correlate with sleep improvement [10].
4.7. Strengths
- This is probably the first study in Nigeria to explore the relationship between dysfunctional beliefs and attitudes about sleep and insomnia in a vulnerable population. The study used internationally accepted instruments (DBAS-16, ISI and GDS) which made its findings easily comparable with similar studies in other parts of the world.
4.8. Limitations
- The study’s design was cross-sectional which partially shows a temporal relationship (but not a causal one) between variables. The use of self-report questionnaires may likely have predisposed the respondents to both response and recall bias. Although the study identified negative sleep beliefs among the respondents of this study, it did not identify culture specific myths and traditions regarding sleep, which may also have implications for management. Some important confounders such as use of psychoactive substances as alcohol and tobacco were not corrected for.
5. Conclusions
- Identifying and targeting dysfunctional beliefs and attitudes about sleep in the elderly remains a key to the successful understanding of the aetiology and treatment of insomnia. This study informs consumers, caregivers and health workers in Nigeria of the presence and role of dysfunctional sleep beliefs and attitudes in sleep disorders among the elderly.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML