-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
p-ISSN: 2332-8355 e-ISSN: 2332-8371
2017; 5(1): 10-15
doi:10.5923/j.ijcp.20170501.02

Psychopathology among Offenders in a Nigeria Prison
Afis Agboola1, Emmanuel Babalola1, Owoidoho Udofia2
1Neuropsychiatric Hospital, Aro, Abeokuta, Nigeria
2University of Calabar, Calabar, Nigeria
Correspondence to: Emmanuel Babalola, Neuropsychiatric Hospital, Aro, Abeokuta, Nigeria.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of this study was to determine the prevalence of psychopathology among inmates in a Nigeria prison. It also explored the relationship between psychiatric morbidity and physical comorbidity. Ninety four prisoners were administered sociodemographic questionnaire, General Health Questionnaire (GHQ 28) and Present State Examination was done. PULSE Profile was used to evaluate physical and functional disability. Majority of the inmates were young offenders (62.8%), 57.4% scored 5 and above on GHQ 28. One third of the inmates (32.8%) had depression. There is high prevalence of psychopathology among prison inmates. Continuous efforts should be made to provide adequate mental health services in prisons.
Keywords: Psychopathology, Offenders, Prisons, Nigeria
Cite this paper: Afis Agboola, Emmanuel Babalola, Owoidoho Udofia, Psychopathology among Offenders in a Nigeria Prison, International Journal of Clinical Psychiatry, Vol. 5 No. 1, 2017, pp. 10-15. doi: 10.5923/j.ijcp.20170501.02.
Article Outline
1. Introduction
- Societies worldwide have designed methods and means of protecting their citizens from individuals who pose a threat or have the potentials of causing harm to others. Imprisonment is meant to reform, rehabilitate and re-integrate offenders back to the society. It is not an ideal place to manage mentally disordered inmates because of the stressful nature of the prison environment [1, 2]. Although prisoners represent a very small proportion of the total global population, they are likely to be extensive consumers of a wide range of health services [3, 4]. This is because the condition of incarceration can cause both physically and emotionally distress on the inmates, predisposing them to mental illness. In fact mental health problems are by far the most significant cause of morbidity in prison [5, 6].Singleton and colleagues in 1998 [7] reported that a third of male prisoners and two fifth of female prisoners with mental illness, also have longstanding physical complaints. Among men, musculoskeletal complaints were most common followed by respiratory complaints. The Country Reports on Human Rights Practices for 2015 on Nigeria reported the deplorable conditions in Nigerian prisons. Inmates and detainees most of whom are awaiting trials are “subjected to torture, extrajudicial execution, food and water shortages, gross overcrowding, inadequate medical treatment, deliberate and incidental exposure to heat and sun and infrastructure deficiencies that led to wholly inadequate sanitary conditions that could lead to death” [8].The mental health of individuals in incarceration are often neglected as routine health screening is not usually done, resulting in a severely overcrowded situation containing mentally disordered offenders who in the opinion of prison medical officers need treatment in a psychiatric hospital [9]. Few studies of psychiatric morbidity among offenders have been carried out in Nigeria [10, 11]. Some of the studies were focused on specific mental disorders among the prisoners [12-14]. None of the local studies have focused on both awaiting trial and convicted prisoners; neither has any show the relationship between psychiatric disorder and co-existing physical illness. The assessment of mental health requirement of the prisoners is necessary for holistic health services planning in our penal institution. Adequate health services, if need be a complete overhauling of the existing health services may be necessary so as to reduce the burden of care on the staff, with fewer disturbances and possibly reduction in the rate of suicide among the prisoners. This study aimed at determining the prevalence of psychiatric disorders among prisoners in Southern part of Nigeria. It also set out to explore the types of physical co morbidity among inmates with psychiatric illness and assess the relationship between psychiatric morbidity and physical co-morbidity.
2. Methodology
- This is a descriptive cross sectional study carried out at the Calabar prison, located in the South-South geopolitical zone of Nigeria. The prison has a population of 278 inmates (male awaiting trial were 162 while 106 were convicted). Female inmates were ten in numbers (8 awaiting trial and 2 convicted inmates). However, only the male population was involved in the study because there were just 10 female inmates in the prison at the time of the study which made it difficult for comparison. Out of the 268 inmates, 228 inmates met the inclusion criteria which were (1) wiliness to participate in the study. (2) Not too physically ill to participate in the study. (3) Ability to communicate in English language. Permission was granted by the prison authority with ethical approval obtained from ethical committee of Federal Psychiatric Hospital Calabar. All the participants were duly informed about the study and they gave verbal informed consent. Strict confidentiality was emphasized to the inmate as much as possible.Socio-demographic questionnaire designed by the researchers was used to elicit information from the participating inmates on variables such as age, marital status, highest completed level of education etc.The General Health Questionnaire 28 (GHQ 28) covers four identifiable areas of distress depression, anxiety, social impairment and hypochondriasis. It is used as a screening instrument for mental disorders with diagnosis confirmed with a more specific instrument. GHQ can be used in a large survey like the institutionalized population, primary health care center or community.The Present State Examination (PSE) is a semi-structured instrument which systematically covers all the phenomena that is likely to be considered during a mental state examination. The interviewer usually a psychiatrist is trained on how to identify abnormal phenomena than could have been present for a specific period of time usually within last four weeks, and also to rate their severity. It contains 140 items, each item is rated on a 3 or 4 point scale. Most symptoms are scored 0, 1, 2, 8, or 9. 0 mean the symptoms was absent during the last four weeks. Scores like 1 or 2 or 3 depends on the severity of the symptom present. Eight mean that is the examiner is not sure whether the symptom(s) is present or not after proper enquiry from the patient and 9 means that either the question was not asked from the patient or the answer given should be disregarded for the purpose of rating the present state but they are noted in the schedule for easy reference when the history is taken. The Pulse Profile is an instrument was designed to evaluate any physical or functional disability in the activities of daily living of a chronically ill patient or elderly patient or institutionalized population. It indicates impairment in term of physical abnormalities. The components of the acronym PULSES are as follows P= physical condition, U= upper limb function, L= lower limb function, S= sensory components (speech, vision, hearing), E= Excretory function, S=mental and emotional status. Summation of the six components resulted in a range of scores from 6, indicating no functional disability as a result of the physical illness considering the age of the patient, to 24 indicating severe physical or functional disability. Reference standard scores above 6 but below 12 indicate mild disability, scores above 12 but below 16 reflect moderate disability and the scores above 16 represent severe disability.
3. Procedure
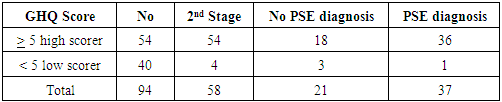
- The study was conducted in 2 stages. The first stage was the administration of the GHQ 28 to the 94 inmates selected from a simple random sampling of all the 228 male inmates. Prisoners were asked to complete the self-administered questionnaires alone during their work time rather than when they are in groups in order to discourage other people influence when answering the questions. Completion of the questionnaire was voluntary. Completed questionnaire were returned directly to the first author by the inmates in order to maintain strict confidentiality. Out of the 94 inmates that were given GHQ 28 questionnaire, 40 of the inmates scored less than 5 while 54 of the inmates scored 5 and above on the GHQ 28 questionnaire. Ten percent of the 40 inmates (4) that screened normal on the GHQ 28 questionnaire and the 54 inmates who scored high on the GHQ 28 questionnaire, all together making 58 inmates proceeded to the second stage of the study. The second stage was in form of clinical interview using Present State Examination (PSE 9) and detailed physical examination was carried out on them using the PULSES Profile as a guide to elicit any history of past or present physical illness. However those inmates with evidence of physical co-morbid illness were classified under the broad categories of ICD 10.Data was analyzed using Statistical packages for social sciences (SPSS) version 21.0 [15]. Frequency counts and chi square test was used for categorical variable. Continuous variable were analyzed by means, and one-way analysis of variances (ANOVA) at 5% level of statistical significant.
4. Result
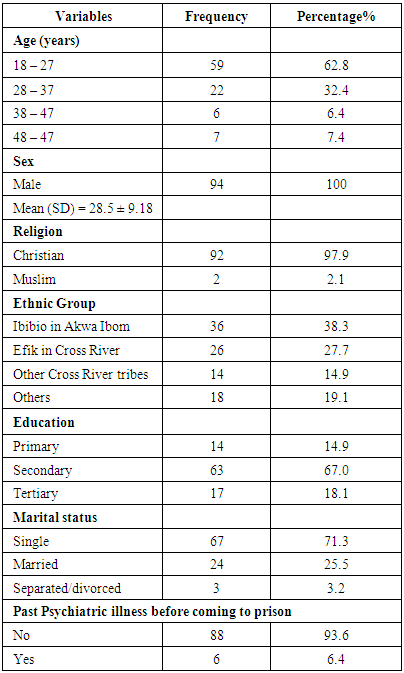
- There were 94 (100%) males in the study with ages ranging from 18 to 64 years and mean age of 28.5 years, SD = 9.18. Majority of the subjects were young offenders aged between 18 to 27 years 59 (62.8%). Seven (7.4%) of the inmates were 48 years and above. Sixty seven (71.3%) of the subjects were single, while 24 (25.5%) are married. Educational profile of the respondents revealed that majority of them were secondary school dropped out 38 (40.4%) and only just 6 (6.4%) of the inmates had a full tertiary education. The subjects were Nigerians of different ethnics background, however Ibibio ethnic group were in the majority. Almost all the inmates were Christians 92 (97.9%) among the studied population. Table 1
|
|
|
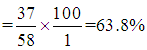 Un-weighted specificity = low scorer that turn out to be no PSE diagnosis divided by total number of no PSE diagnosis, multiply by 100
Un-weighted specificity = low scorer that turn out to be no PSE diagnosis divided by total number of no PSE diagnosis, multiply by 100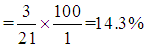 Un-weighted sensitivity= high scorer that turn out to be PSE diagnosis divided by total number of PSE diagnosis multiply by 100
Un-weighted sensitivity= high scorer that turn out to be PSE diagnosis divided by total number of PSE diagnosis multiply by 100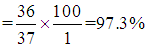 However since there were no equal number of high and low scorers in this study, the sample have to be weighted back to represent the original score distribution.High scorers = since all the 54 high scorers proceeded to second stage therefore
However since there were no equal number of high and low scorers in this study, the sample have to be weighted back to represent the original score distribution.High scorers = since all the 54 high scorers proceeded to second stage therefore  Then multiply all the high scorers PSE diagnosis and no PSE diagnosis by 1.Low scorers = since there were 40 low scorers and only 4 proceeded to second stage therefore
Then multiply all the high scorers PSE diagnosis and no PSE diagnosis by 1.Low scorers = since there were 40 low scorers and only 4 proceeded to second stage therefore  Then multiply all the low scorers PSE diagnosis and no PSE diagnosis by 10.
Then multiply all the low scorers PSE diagnosis and no PSE diagnosis by 10.
|
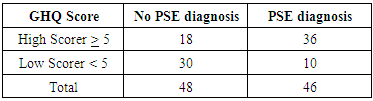
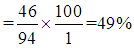 True Specificity
True Specificity 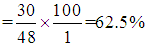 True Sensitivity
True Sensitivity 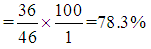 This method of calculating weighting of the sample subjects was obtained from Goldberg (1988) handout on two stage screening survey.
This method of calculating weighting of the sample subjects was obtained from Goldberg (1988) handout on two stage screening survey.5. Discussion
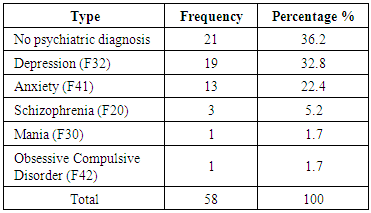
- The main findings in this study were as follows: high prevalence rate of mental disorders in Calabar prison, depression was the commonest psychiatric illness among the inmates however, only a few were brought to the attention of the prison medical officials, approximately half of the subjects with mental disorder also have co-morbid physical illness, there was significant association between psychiatric disorder and co-morbid physical illness. Majority of the inmates were young, single offenders of low educational background. Young people between the ages of 18 to 27 years as observed in this study were prone to commit crime because; during the early period of their life especially at the adolescent period, their personality is just taking shape, they can easily succumb to peer pressure. In the Nigerian society, success is measured by material possessions; there is tendency for young people to want to acquire these physical materials by all means possible. Good education or vocational training can provide a legal source of income or even influence sense of reason to be a good citizen in a society. However, crime is not synonymous with poor educational status or low socioeconomic class. Findings in this study are similar to reports of previous works carried out elsewhere. A study found preponderance of young male adult below the age of 40 years [7]. Adesanya and colleagues reported predominantly young male adult with poor educational background and social status [11].It is a source of concern to note that the majority of the inmates were on the awaiting trial lists. Prison is normally a place where reformation and rehabilitation of offenders that have been found guilty take place. A situation where a first time offender of minor crime like stealing and whose trial is not concluded even after 6 months in prison is a source of worry to even the prison officials themselves. However the recent reform in the judiciary system culminating in prison decongestion of late is a good omen. It is uncommon in high income countries to have first time offenders subjected to the same stressful, restricted condition together with the harden criminals. The high prevalence of psychiatric disorders in this study could be due to psychoactive substance abuse before and during imprisonment. Most of the violent crimes like murder occurred under the influence of drug intoxication, in fact majority of the subjects gave past history of drugs intake before imprisonment and even some of the inmates admitted to occasional intake of cannabis that was smuggled into the prison. Poor access to full medical services in the prison may also be contributory. Lack of adequate medical facilities in prison is a major problem, even those inmates who are known psychiatric patients do have frequent relapse because of irregular supply of medications from the prison headquarter in the nation’s capital city. The only prison medical officer in the state have to oversee provision of services at two prisons with large inmates population, and he is also responsible for provision of services to the entire prison staffs at the zonal headquarter in Calabar. The daily rigid and strenuous routine activities and confinement to a place for an unusual long period of time is a major psycho stressor to the prisoners.Depression was the commonest mental disorder however, only few of them were brought to the attention of the visiting psychiatrists. Most of the affected inmates were suffering silently, receiving medical treatment for body weakness, recurrent headache and internal heat instead of psychiatric evaluation and treatment. Lack of adequate manpower for the delivery of psychiatric services is responsible for this situation. Although the prison authority have an agreement with the Federal Psychiatric Hospital Calabar for provision of psychiatric services however, the psychiatric hospital are not encouraged enough to continued rending the services to the inmates because of lack of basic antipsychotic medication. Reason for high rate of depression could also be due to the fact that majority of the inmates with depression belonged to the awaiting trial prison category, their cases were yet to be concluded even after spending 3 to 4 years in the prison. This situation can lead to feeling of helplessness and hopelessness especially if they were innocents.Only few authors assessed co-morbid physical illness among the inmates in their study. Singleton et al in 1998 [7] reported that musculoskeletal problem was the most common co-morbid physical illness among male prisoners in England and Wales followed by respiratory problem. Agbahowe [16] reported disease of the gastro-intestinal system (peptic ulcer and inguinal hernia) as the commonest physical illness followed by disease of eye (visual difficulties). For an ideal screening instrument like the GHQ 28, it should be highly sensitive and specific. This has been confirmed with the GHQ 28 questionnaire by various researchers all over the world however, in this particular study, GHQ 28 was not highly sensitive and specific for these set of prison population. Before weighting the sensitivity was high and specificity was low but after weighting, taken into consideration that some of the inmates who scored high on the GHQ questionnaire but do not have ICD 10 diagnosis after the PSE was administered, the sensitivity dropped but the specificity increased. This observation may be due to the cutoff point of 5 which may be too high for this study. Cut off point of 4 may be ideal for a study of this nature. Some of the inmates may have deliberately scored themselves high with the hope that they may be released from the prison on the ground of psychiatric illness this was obvious to this author during the second stage of the study. Also the level of motivation during the period of answering the GHQ questions may be responsible. Some of the inmates may have exhibited what is known as Hawthorne effect (answering the questionnaire in a manner that will please the researcher requesting them to fill the questionnaire or according to the dictate of the people around). However from the review of the available prison studies carried out in Nigeria no report was given of validity of the screening instrument with that of the instrument used in making the psychiatric diagnosis among the inmates.
6. Limitations of the Study
- This is only a descriptive study. The study do not include control group of people who consult their doctors for various psychiatric reason in the community. Information given by the participants may not be highly reliable as evidenced by larger percentage of those with no PSE diagnosis during the second stage of the study despite scoring high in the self- administered GHQ 28 questionnaire. Present State Examination (PSE 9) only assessed one month prevalence of mental disorder. It does not have provision for making lifetime diagnosis. Some of the inmates gave past history suggestive of psychological symptoms while in prison but the symptoms “subsided or disappeared” according to them after seeing the prison medical staff that provided counseling on how to adjust to their new environment. Also the PSE 9 does not have the provision for making diagnosis of personality disorder, mental retardation and alcoholism. Future study should involve the use of Structural Clinical Assessment in Neuropsychiatry (SCAN) and International Personality Disorder Examination (IPDE) where there were provisions for making these diagnoses.
7. Conclusions
- There is a high rates of psychiatric disorders found among prison inmates in Nigeria when compared to prisoners in more affluent countries. This should stimulate further research in this area with the aim of reducing the suffering of the affected prisoners. Delays in sending prisoners to the psychiatrists for psychiatric assessment as recommended by the courts are adding to the problem of the mentally disordered prisoners in the country thus, denying them treatment of their condition. With the present situation within the prison environment, treatment of mentally ill offenders is a mirage because of the absence of adequate psychiatric services and the inability of the prison clinical staff to detect the signs and symptoms of abnormal behaviors among the inmates.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML