-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
2016; 4(1): 8-16
doi:10.5923/j.ijcp.20160401.02

Coping Strategies and Family Functioning as Predictors of Stress among Caregivers of Mentally Ill Patients
Lubna Ghazanfar , Sameera Shafiq
Department of Psychology, University of Gujrat, Hafiz Hayat Campus, Gujrat, Pakistan
Correspondence to: Sameera Shafiq , Department of Psychology, University of Gujrat, Hafiz Hayat Campus, Gujrat, Pakistan.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The present study was conducted to examine primarily objective that the family functioning and Coping strategies act as the predictors of stress in caregivers. The sample of the study comprised of 150 respondents (25% males and 75% females) purposively selected from five different hospital settings located in Gujrat and its nearby cities. Demographic questionnaire along with Urdu versions of Self-Report Family Inventory (Beavers, Hampson & Hulgus, 1990) [1], Coping Strategies Questionnaire (Kausar & Munir, 2004) [10], and Perceived stress scale (Mariam et al., 2011) [14] were used to collect the data. Results revealed that among demographic variables gender showed statistically significant difference with respect to family functioning, coping strategies, and stress, whereas other demographic variables, including age, family system and relation to patient showed statistically significant differences with respect to coping strategies only. Further, the findings indicated a significant correlation between family functioning and stress. Furthermore, the family functioning accounted for 54 % of the variance for stress and was significant predictor, while coping strategies did not predict stress among caregivers. Limitations and Recommendations of the research are discussed.
Keywords: Family functioning, Stress, Coping Strategies, Caregivers
Cite this paper: Lubna Ghazanfar , Sameera Shafiq , Coping Strategies and Family Functioning as Predictors of Stress among Caregivers of Mentally Ill Patients, International Journal of Clinical Psychiatry, Vol. 4 No. 1, 2016, pp. 8-16. doi: 10.5923/j.ijcp.20160401.02.
Article Outline
1. Introduction
- Family is defined as a dynamic, collaborative system in which what affects one member of the family automatically reverberates throughout the system, resulting in affecting all members of the family. Family functioning refers to how a particular family operates and interacts within and outside the family with other social systems [34]. It comprises of the ways in which family members communicate, interact with, and relate to each other in a variety of activities such as setting of goals, pursuing of goals, family activities that provided an opportunity to the family members to involve in together, and accept all the family rules, routines and employ efforts to solve problems [20, 33]. The Beavers Systems Model conceptualizes family functioning as comprising of family competence encompasses all the structural available information, and resiliency level of the family members, requiring the capability of the family member to adjust to changes that occur throughout their life cycle. It implied that every family member can understand, appreciate different viewpoints of all family members and recognize that behaviors of all family members are interconnected and entrenched in interpersonal patterns, and as a result, there are least possibilities of blame game within the family [2].Families living with the mentally ill family members often face more stress than the ones who are living apart. Primary caregivers normally become isolated from friends and family devoted little time for sustaining social networks and friendships, thereby resulting in an increase in social isolation. Caregivers with no adequate social support feel isolated and alone in the process of caregiving with higher level of stress and family conflicts, further aggravating this condition. Schock and Gavazzi (2005) [28] explained subjective burden as an evaluation made by a family member regarding illness caregiving experience that comprised the stigma or shame attached to mental illness.Tull (2008) [32] explained the experience of a burden as a high level of stress that caregivers encounter because of caregiving for an ill family member. Stress is a response of the individuals to various stressors that occur in their daily life, particularly threaten their coping abilities, and ultimately individual perceives himself/herself to be not capable enough to manage these situations [27]. The stress comprised of all nonspecific changes within an organism caused by the stressors damage and the rate of wear and tear in the body that resulted in a general but a consistent set of reactions within the body [26]. The caregivers have to encounter sudden family circumstances, financial difficulties, and fatal events related to their loved one’s care. The more challenging the needs of mentally ill, the more difficult and hectic the caregiver's role might be. Often the caregivers have to work hard [24]. They did not have enough free time to spend in leisure activities, with friends, handling personal matters, eventually resulting in stress. Coping involves handling challenging situations, employing efforts to solve problems in one’s life, and making oneself capable enough to manage and reduce stress. A successful coping undergoes several characteristics, including one’s sense of personal control, positive emotions, and personal resources and further it depends on the context in which particular coping strategies used because, often people employ various coping behaviors, out of which some are more successful than others are [5]. Coping strategies as problem-focused coping and emotion-focused coping. In problem-focused coping, a person directly faces whatever the troubles are and employs efforts to solve them. Whereas, in emotion-focused coping a person respond to stress specifically by using defense mechanisms, such as by avoiding the particular problem, justifying what has occurred, refuting it is happening, giggling it off and use religious beliefs as a way of support to deal with stress [5].The positive coping strategies prove to be effective and satisfactorily while dealing with stress and, ends in a peaceful resolution of the problem. Whereas, negative coping strategies, on the other hand, provide not enlightened resolution, instead, they perpetuate perception of stress and further ineffective responses in a vicious circle that may never be broken or intercepted e.g., to avoid the problem, emotional rigidity, hostility, aggression, and self- damaging behaviors [29].Having social support could help people feel worthy, and can bulwark the stress by either providing sufficient resources for coping with stress or making the individuals to perceive stress as less threatening. The greater social support from family perceived as healthy family functioning was related with lower levels of caregiver stress [14]. Caregivers who reported poor family functioning showed higher scores of stress and burden [9, 6]. While the stress and coping model along with social support theory guides the framework of current study, the research has examined family functioning and coping strategies as a predictor of stress among caregivers of mentally ill patients.In the present research, the family functioning was operationally defined as the overall wellbeing of a family unit in such domains as family health/competence, conflict, cohesion, leadership, and emotional expressiveness. Family competence refers to as how well the family, as an interactional unit, performs the necessary and nurturing tasks of organizing and managing itself. It was measured in terms of the family affect, parental coalitions, optimistic versus pessimistic views and family problems. Family Conflict was measured in terms of overt and covert conflict, including arguing, blaming, fighting openly, acceptance of personal responsibility, unresolved conflict, and negative feeling tone in the family. Cohesion was measured in terms of family togetherness, satisfaction received from inside the family versus outside, and how much time the family members spend together. Leadership refers to parental leadership, directiveness and degree of rigidity of control. Emotional Expressiveness refers to the open expressions of warmth by family members, caring and closeness by verbal and nonverbal means [1]. Stress, was operationally defined as subjective evaluation made by the individuals perceived as family functioning of caregivers keeping in focus the overall wellbeing of the family. It was measured as the degree to which the person perceives their lives as unpredictable, intense and challenging [4]. Coping strategies has been measured in terms of following domains such as active-practical coping, active-distractive coping; avoidance-coping and religious focused coping strategies. Active practical coping refers to practical efforts to deal with stressful event. Active distractive strategies involve active but not problem focused efforts such as going out with friends, involving in leisure activities; Avoidance coping included strategies such as isolation withdrawal; Religious focused coping strategies included strategies such as praying more than usual, recitation of the Quran more than usual [10].
1.1. Theoretical Framework
- The theoretical framework of the present study was directed by Stress and Coping Model of Lazarus and Folkman (1984) [13] and Social Support theory by Lakey and Cohen (2000) [12].Coping strategies has been explained as the behaviors, thoughts, and emotions that caregivers employed to regulate the changes that take place in their life. It depends on the strength of available resources whereas stress is the consequence of imbalance created between demands and resources. Every stressor endures primary appraisal to determine the level of harm, which is then, suppressed in a secondary appraisal. This is the point, where a person lined up a range of coping responses with that particular stressor to determine the best course of action. Thus, individual become stressed when demands surpasses his/her resources such as his/her ability to cope and intervene stress. Therefore, it is more important how a person perceives and interprets the particular stressful event rather than the event itself [13]. Coping strategies have significantly contributed as a predictor of burden which is an indicator of stress [11, 8]. The second theory is Social Support Theory, which gives clear direction for conceptualizing family functioning in a supportive role to reduce the impact of stress. Social relations affect our behaviors, biology, cognitions, and emotions and normally persons perceive that close relationships comprising of family members are available as support if they needed [12]. Social support perspective predicts that supportive actions of family members protect people from stress by improving their coping performances. In Pakistan due to the limited psychiatric settings and high expenses of inpatient’s services, there is a high burden on family members while caring for the patients with psychiatric disorders. In an effort to provide the best possible care for a family member, caregivers often sacrifice their own physical and emotional needs and the emotional and physical experiences involved with providing care can strain even the most capable person. Family functioning is an important aspect of the family environment that influences the physical, social and emotional wellbeing of individuals, what actually happens within the family and how it functions can be a key protective factor in determining the healthy personality of caregivers and reducing their current and future risks associated with any problem. Lack of psychosocial support from the community to families of mentally ill patients resulted in high burden of stress [2]. Belief that support is available reduces the effect of stress by contributing to less negative appraisals, if one feels supported from the family it may be helpful in successful coping with stress [3]. The greater social support from family perceived as healthy family functioning was related with lower levels of caregiver stress [13]. Caregivers who reported poor family functioning showed higher scores of stress and burden [16, 9, 6]. While the stress and coping model along with social support theory guides the framework of current study, the research has examined family functioning and coping strategies as a predictor of stress among caregivers of mentally ill patients.The physical and psychological effect of somebody providing caregiving services at home can bring stress as it creates social, emotional, behavioral, and financial problems for the family members, affects the family functioning of caregivers, and, as a result, confines their personal life. Being exhausted from caregiving responsibilities may limit how well the person performs, which may cause problems for them. These problems eventually cause stress for the caregivers and can affect their all domains of life, including work, socializing and relationships, unless or until they used effective ways to cope with that stress. The following study aimed to explore the relationship among variables and, to find out whether family functioning and coping strategies predict stress in caregivers. Further, to find out the differences among caregivers on family functioning, stress and coping strategies with respect to demographic variables such as age, gender, family system, diagnosis of the patient, relation to patient and education level. Therefore, the hypotheses of the present study stated as follows.
1.2. Hypotheses
- Hypotheses of the present study postulated as follows.H1-Family functioning and coping strategies will predict stress among caregivers of mentally ill patients.H2-Female caregivers of mentally ill patients will have statistically significant higher scores on family functioning, stress, and coping as compared to male caregivers.H3-Parents of mentally ill patients will have statistically significant higher scores on family functioning, stress and coping as compared to siblings, spouses and children.
1.3. Rationale of the Study
- In previous studies, there has been less attention on the family functioning of the caregivers who take care of the patient and clinicians hardly give any attention to their needs. Therefore, this study was conducted to find out the family functioning of the caregivers of mentally ill patients, along with perceived stress. The implications of this study would be helpful for the clinicians in developing constructive working relationships with caregivers, and considering their needs, as an essential part of service provision for people with mental disorders who require and receive care from their relatives. Moreover, it would instigate them to introduce interventions programs which would reduce the burden on caregivers, lessening their stress; improve the caregiver–patient relationship and overall family functioning. They could provide caregivers with much of the information they need to better cope with their stressors as well as their relatives’ mental illnesses. It is crucial for mental health professionals to be sensitive to the stress and burden experienced by families, in order to plan and implement a comprehensive treatment programs. This would also facilitate enhancing the quality of life of both- the mentally ill, and their families.
2. Method
2.1. Research Design
- The present study has used a survey research design in which the correlation between family functioning and coping strategies was assessed to predict stress among caregivers of mentally ill patients by selecting them while their visit in the psychiatric wards of the hospitals. This research design was applied to find out the predictive value of the variables such as family functioning and coping strategies acting on the level of stress experienced by the care providers of the patients having any type of the psychiatric disorders.
2.2. Sample
- The sample of the present study was the primary caregivers of mentally ill patients. Purposive sampling technique was used for the selection of sample of 150 caregivers from five different hospital settings located in Jhelum, Kharian, and Gujrat, enlisted as Jhelum Poly Clinic Hospital Jhelum, Combined Military Hospital Kharian Cantt, Subhan Hospital Kharian, Aziz Bhatti Shaheed Hospital Gujrat, and Umar Arshad Hospital Gujrat. There were 25 % male caregivers and 75% male caregivers. Majority of the caregivers were parents (41%), children (21%), siblings (21%) and spouse (17%). Family caregivers who were healthy (not having diagnosed mental or physical disability) primary relatives (parents, siblings, spouses, and children) of patients with mental illness and showed willingness to participate in the research, were included in the sample. Verbal and written informed consent was taken from uneducated and educated caregivers respectively.
2.3. Instruments
- The following scales are used in the present study1) Self-Report Family Inventory is a 36 item self-report instrument originally developed by (Beavers, Hampson & Hulgus, 1990) [1]. In the present study, Urdu version of this scale was used to assess family functioning of respondents on the five dimensions of health/competence, conflict, cohesion, leadership, and emotional expressiveness. It is a five- point scale for each item ranging from 1 to 5. The scale has high internal consistency reliability with Cronbach’s alpha between .84 and .93 and test-retest reliability of .85.2) Perceived Stress Scale originally developed by Cohen, Kamarck, and Mermelstein, 1983) [4]. In the current study Urdu version of this scale translated by Mariam et al. (2011) [14] was used. The Perceived stress scale measures the individual’s subjective evaluation of the stressful situations in the past month of their lives. The scale has good reliability Cronbach alpha 0 .78. The respondent has to indicate on a 4-point scale.3) Coping Strategies Questionnaire (Kausar & Munir, 2004) [10] was used to measure coping strategies employed by caregivers of mentally ill patients. It comprised of 62items and was specifically developed for Pakistani population in the Urdu language. It is a 4-point scale with four subscales, namely as active-practical coping, active-distractive coping, avoidance-focused coping and religious-focused coping with 0.72, 0.58, 0.55 and 0.73 alpha reliabilities respectively. The total alpha reliability for CSQ is 0.89.
2.4. Procedure
- Permission was taken not only for the usage of the scales but also to collect data from the five hospital settings: Jhelum Polyclinic Hospital Jhelum, Combined Military Hospital Kharian Cantt, Subhan Hospital Kharian, Umer Arshad Hospital Gujrat, and Aziz Bhatti Shaheed Hospital Gujrat. Caregivers who were primary relative of the patients, have been approached purposively. They were briefed about the purpose of data collection and were, instructed to read each statement carefully and choose the option, which was most suitable according to their own opinion. For the majority of caregivers, interview technique was used as a method of data collection. Data were collected after obtaining a verbal and written consent from the caregivers. It took about 40-45 minutes for each participant and almost three months to complete data collection process via instruments mentioned earlier.
3. Results
- The data collected from 150 purposively selected caregivers with the help of the standardized questionnaires, were analyzed using SPSS statistical package version 22.0 and is given below:
|
|
|
|
|
|
4. Discussion
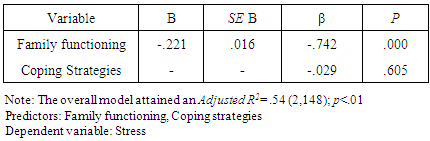
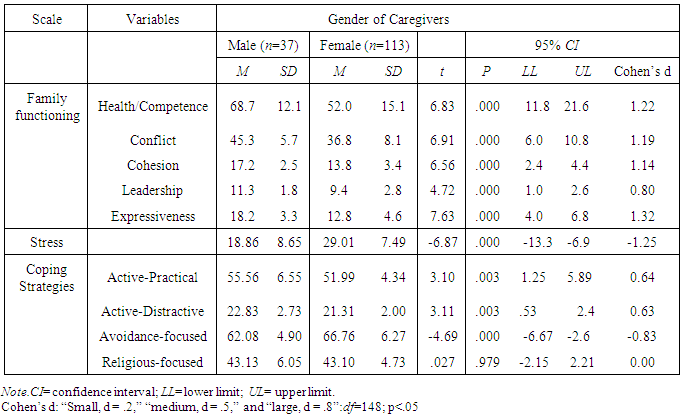
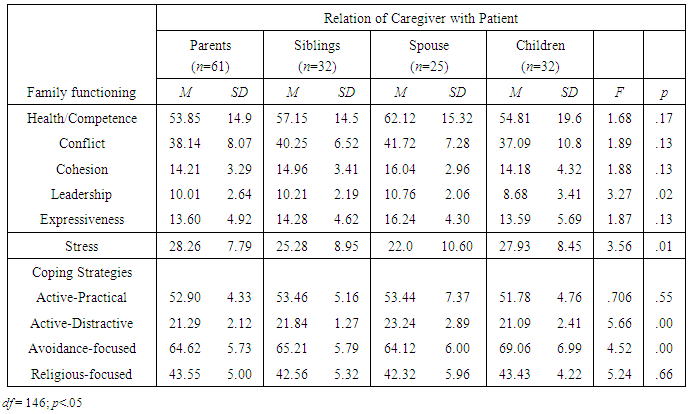
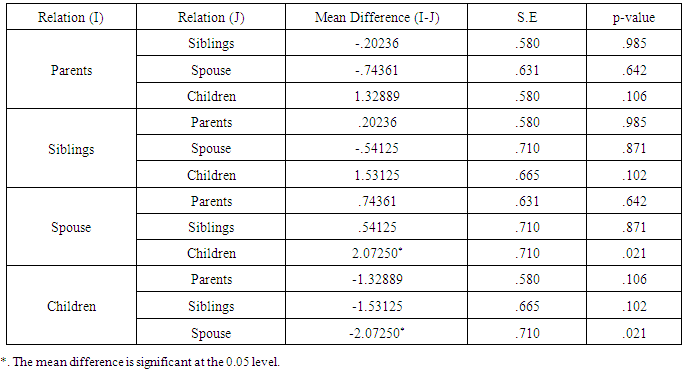
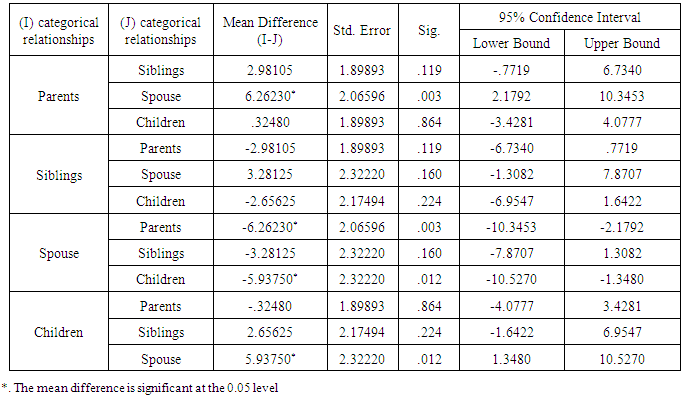
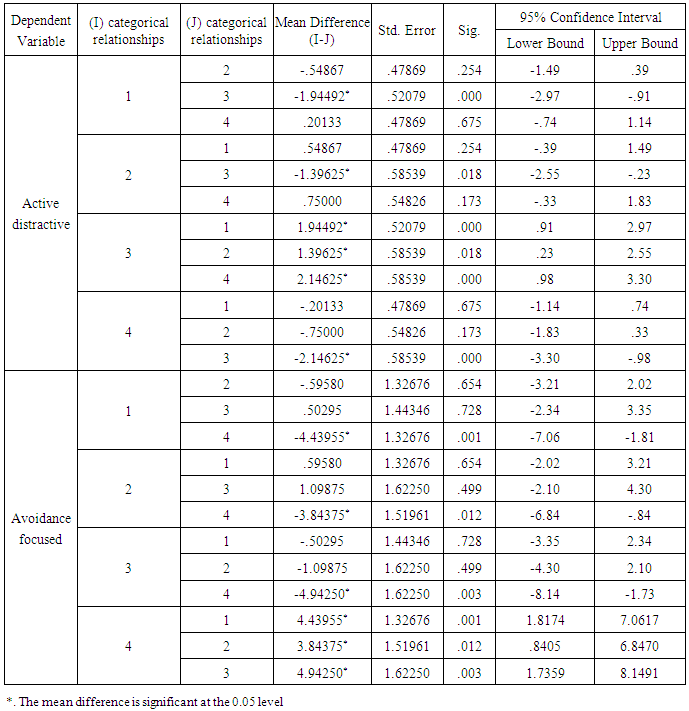
- The 1st hypothesis of the study stated that family functioning and coping strategies predict stress among caregivers of mentally ill patients. Findings of the present study depicted in the table 1 revealed that family functioning accounted for 54 % of the variance for stress, and were significant predictor, whereas, coping strategies did not predict stress among caregivers. These findings are, supported by the findings of the study conducted by Mitrani et al. (2006) [17], which revealed that family functioning showed significant contribution to stress among caregivers. Further, it is supported by the study of Clark et al., (as cited in Radomski & Latham, 2008) [22] reported that premorbid family functioning is an important predictor of stress in caregivers. However, these findings are not, supported by the study conducted by Kim, Chang, Rose & Kim (2011) [11] reported that coping strategies significantly contributed as a predictor of burden, which is an indicator of stress. The possible reason for this finding is that specifically in Gujrat region, no psychiatric institution has been found to be devoted in providing knowledge and information regarding mental illness, treatment and coping skills to the family members of mentally ill patients. Family members endure various stressors comprises of stigma, shame, financial burden, often they feel dismayed which resulted in mishandling of the patient. They don’t know how to cope with these stressful conditions. The 2nd hypothesis of the study stated that female caregivers of mentally ill patients will have higher scores on family functioning as compared to male caregivers. Findings from the table 2 indicated significant gender differences in all dimensions of family functioning among caregivers of mentally ill patients as the mean score of male caregivers are higher as compared to female caregivers. The possible reason for this finding might be the majority of the caregivers as females. In Pakistani culture, women face many social and cultural pressures, mostly stayed at home, and are responsible for all household activities. Family nurturance along with providing primary care to their mentally ill member for the whole day is part of their core duties. They are less likely to obtain any formal help from other family members.Moreover, the female caregivers of mentally ill patients will have higher scores on stress as compared to male caregivers. Findings from the table 2 indicated significant difference in stress among caregivers of mentally ill patients with respect to their gender, as females experience more stress as compared to males which is consistent with the findings of Mitsonis et al. (2010) [18] who has reported significant higher level of stress experienced by female’s caregivers than males. The possible reason for this finding is that male members are more resilient and committed in providing caregiving as compared to females. It is consistent with the views of Greene (2012) [7] that caregiver stress seems to affect women more than men caregivers. The findings of the study have further showed significant gender differences among caregivers of mentally ill patients on active-practical, active distractive and avoidance focused coping strategies. Whereas, it indicated no significant difference on religious coping strategies with respect to gender of caregivers as depicted in the table 2. According to the findings, male caregivers used active practical and active distractive coping strategies more as compared to female. The possible reason might be that in Pakistani culture mostly the male members of the family have more commitments and socialization as compared to females. These findings of the study are also consistent with the findings of the study conducted by Mays and Lund (1999) [15] indicated that male caregivers are more committed and resilient in providing care for mentally ill persons and used more action oriented, persistent and firm approaches.Findings of the study depicted in table 2 also showed that female caregivers of mentally ill patients used avoidance coping strategies more as compared to male caregivers. These findings are consistent with the study conducted by Stephens, Norris, Kinney, and Grotz (1988) [31] who examined the ways in which caregivers cope with stressful situations. Findings indicated that the caregivers who used more escape-avoidance coping strategies experience more stress, depression, and conflict in personal relationships as compared to the caregivers who used positive coping strategies more, and majority of the caregivers were women who used avoidance strategies. Further, the findings of the present study depicted in table 2 did not showed significant difference in religious coping which is consistent with the findings of the previous study conducted by Pun, He and Wang (2014) [21] who examined the extent of burden and identify coping strategies embraced by family caregivers living with psychiatric patients.The 3rd hypothesis of the study stated Parents of mentally ill patients will have higher scores on family functioning. Findings of one-way analysis of variance of the study from the table 3 indicated significant difference on leadership dimension of family functioning among caregivers of mentally ill patients with respect to the relation of caregiver with patient, as spouses, siblings and parents scored high on leadership as compared to children. The possible reason for this finding is the role of caregivers, as a spouse, siblings, and parents of mentally ill patients caregivers have to lead the families, handle with day-to-day life circumstances, unexpected crises, and playing part in family’s decisions making. It has been supported by the views of Peterson (2009) [19] that individual’s roles played an important part in healthy family functioning. Parents are expectedly responsible for guidance, discipline, and providing nourishment for their children, whereas children are expectedly liable to show cooperation and respect to their parents. Parents of mentally ill patients will have higher scores on stress. Findings of one-way analysis of variance of the study from the table 3 revealed significant differences in stress as parents indicated more stress as compared to siblings, children, and spouses of mentally ill patients. Richard et al., (2012) supported that parents and families having adult child or relative suffering from mental illness experience significant losses, to which they react with despair. Parents were specifically apprehensive regarding their child’s social difficulties. They generally detected their child’s functional debility. They experience more stress from an increasing awareness that something wrong was happened with their child, however they did not know exactly what it was, why it was happening and how to fix it [25]. Parents of mentally ill patients will have higher scores on coping strategies. Findings of one-way analysis of variance from the table 3 (a) indicated significant differences in active-distractive and avoidance-focused coping strategies among caregivers with respect to their relation with patient. Spouses used active distractive while, children used avoidance coping more than compared group.These findings are consistent with the findings of Rammohan, Rao & Subbakrishna (2002) [23] who have examined stress perceived as burden and coping in caregivers of mentally ill patients. Findings indicated a significant difference between two groups of caregivers such as spouses of mentally ill patients employed negative distraction more as a way of coping. While findings revealed that children used more avoidance coping strategies. This is supported by the study of Snyder et al. (2014) [30] indicated that caregivers often recognized providing care as a problem and that the use of most coping strategies were stable except the fact that adult child caregivers used more avoidance coping strategy. It might be because in Pakistani society children are not much independent and parents or senior family members are held responsible for decision-makings, and handling major issues.Within or outside the family. Therefore, in case of any stressor in the family children most likely used avoidance coping strategies rather than active-practical coping strategies.
5. Conclusions
- The study concluded that family functioning is a significant predictor of stress among caregivers of mentally ill patients. Female caregivers experienced more stress as compared to male caregivers, among caregivers parents of mentally ill patients were more stressed as compared to siblings, spouses and children. Male caregivers mostly used active-practical and active distractive coping strategies whereas female caregivers used more avoidance coping strategies. Among caregivers spouses used more active-distractive coping strategies whereas children used more avoidance coping strategies.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML