-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
2015; 3(1): 6-8
doi:10.5923/j.ijcp.20150301.02
Three Clinical Cases of Halidol_ Induced Hypochromia
1Drug Information Center, El Minia Psychiatric Hospital
2Manager of El Minia Psychiatric Hospital
Correspondence to: Nagy MA , Drug Information Center, El Minia Psychiatric Hospital.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Several psychotropic drugs, including halidol, may its chronic administration causes hypochromia. Halidol is an antipsychotic drug that the Food and Drug Administration (FDA) has approved for psychosis, schizophrenia and epileptic psychosis treatment. A few cases of halidol-induced hypochromia have been previously reported on, but the pathophysiology and clinical manifestations are not yet known. This case series reports on 3 patients with different medical conditions who experienced hypochromia during treatment with halidol. In these cases, the induced hypochromia occurred upon chronic administration of halidol. We also discuss several characteristics of halidol-induced hypochromia.
Keywords: Halidol, Hypochromia, Psychosis, Schizophrenia, Epilepsy
Cite this paper: Nagy MA , Mahmoud MM , Three Clinical Cases of Halidol_ Induced Hypochromia, International Journal of Clinical Psychiatry, Vol. 3 No. 1, 2015, pp. 6-8. doi: 10.5923/j.ijcp.20150301.02.
Article Outline
1. Introduction
- Halidol is indicated for long term maintenance treatment where a neuroleptic is required. Food and Drug Administration (FDA) has approved for Psychosis, schizophrenia, epileptic psychosis. Blood dyscrasias such as neutropenia, throm bocytopenia and pancytopenia have not also been reported (Sagara., 1998). Furthermore, a few cases of halidol -induced agranulocytosis have been reported, but its exact pathophys iology is as yet unknown. It has been reported that half of the patients with bipolar disorder may take at least 3 psychotropic drugs, and that the usage of multiple drugs increases the risk of hypochromia (Gustafson et al., 2002). Therefore, it is necessary to be aware of the possibility of hypochromia during the treatment of psychosis, schizophrenia, epilepsy with halidol. We report here on 3 cases of hypohromia with their different characteristics during treatment with halidol.
2. Cases
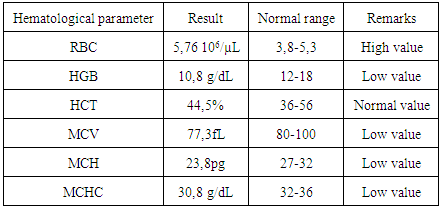
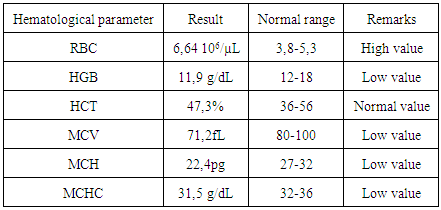
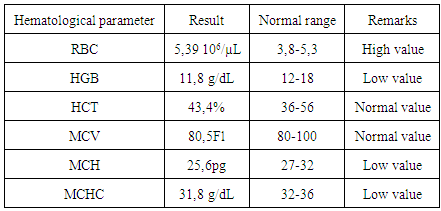
- Case 1A 25-year-old man was admitted to a psychiatric ward due to Schizophrenia. He was treated with halidol amp for 2 continuous years in addition to achtenone 2 mg, respiridone 4 mg and serteraline 100. His measured cystolic blood pressure was 118 mmHg and diastolic blood pressure was 75 mmHg. Normal pulse rate was recorded 86 per min. The investigated random blood sugar was (156 mg/dl). Disturbance in its complete blood count was noticed as following in Table 1:
|
|
|
3. Discussion
- Red blood cells (RBCs) are continuously produced in the bone marrow; when a state of iron deficiency proceeds and the iron stores progressively decrease; mean cell volume (MCV), mean cell hemoglobin (MCH), and red blood cell count (RBC) tend to decline. In iron deficient erythropoiesis, synthesis of Hb molecules is severely impaired leading to the production of erythrocytes with low Hb concentration (hypochromic cells). Because of their long-life span of approximately 3 months, several cohorts of normochromic and increasingly hypochromic red cells coexist in the peripheral blood leading to anisocytosis (Nemeth and Ganz 2006).Hypochromic anemia is a generic term for any type of anemia in which the red blood cells (erythrocytes) are paler than normal. This decrease in redness is due to a disproportionate reduction of red cell in proportion to the volume of the cell. In many cases, the red blood cells will also be small (microcytic), leading to substantial overlap with the category of microcytic anemia (Strippoli et al., 2002). However, the most common causes of Hypochromic anemia were iron deficiency and thalassemia, chronic administration of halidol reviles hypocromic anemia in the presented cases.In case 1 & 2, although the other concurrently administered drugs could not be definitely excluded from the possibility of inducing hypochromia, it is relatively easy to consider halidol amp as the cause of hypochromia because the patients had been taking other drugs for over 6 years without any hematologic abnormalities.In these 3 cases, hypochromia occurred after 2 Years of halidol amp initiation, respectively, and in the 3 previously reported cases, the hypochromia also occurred within 8 weeks. It is likely that halidol amp induced hypochromia has a tendency to occur at the early phase of treatment, which is unlike clozapine that rarely induces neutropenia within the first 6 weeks.The suggested mechanisms that illustrate the obvious relation between halidol administration and induced hypochromic anaemia, may include firstly enhancement of erythrovute destruction due to situmulation of macroghagedto engulg RBCs or lastly depression of bone marrow to synthesize RBSs (Lagman., 2005).The proposed approaches for these mechanisms may need other biomarkers as serum ferritin and Tumor necrosis factors TNF-α to have more clear view. To conclude, at the early phase of halidol treatment or after an increased titration of halidol, it is beneficial for the clinician to aware the possibility of an occurrence of hypochromia (Burkhart., 2010).Regarding Cases 1 & 2 There have been several reports indicating that schizophrenia is related to the activation of the inflammatory response system (IRS), characterized by increased serum concentrations of interleukin 6 (IL-6) and tumor necrosis factor α (TNF-α), which are mainly the products of activated monocytes/macrophages responsible for destruction of RBCs( Pawar et al., 2010) An epileptic seizure occur when large groups of neurons in the brain begin firing uncontrollably, disrupting the balance of electrical activity and causing changes in mental function, motor function and behavior. It’s not known what sets off a seizure, but lately scientists like (O'Connor and Corcoran., 2012) have been gathering evidence that inflammation, the immune system’s response to injuries or foreign organisms, plays a pivotal role.Regarding Cases 3 clinical evidence indicates that inflammatory processes contribute to the pathogenesis of several forms of epilepsy (Fabene et al., 2010). Thus, interactions between leukocytes and vascular endothelial cells modulate spontaneous recurrent seizures (SRSs) in a rodent model of temporal lobe epilepsy (TLE) (Fabene et al., 2008).Anemia of chronic inflammation is a form of anemia seen in chronic immune activation. Inflammatory cytokines promote the production of white blood cells. The up regulation of white blood cells causes fewer stem cells to differentiate into red blood cells. This effect may be an important additional cause for the decreased erythropoiesis and red blood cell production seen in anemia of inflammation (Nemeth et al., 2004). In conclusion, either psychotropic diseases or psychotropic drugs may be responsible for induced anaenia through inflammatory intermediates.
4. Recommendations
- It is recommended for patients chronically administrating halidol to have regular monitoring for ion status parameters as plasma iron in addition to follow up transferrin level in blood for consecutive periods.
ACKNOWLEDGMENTS
- We thank Prof. Dr. HishamRamy, Secretary General of the General Secretarial of Mental Health for his kind support and encouragement. Also, Dr Amr Saad, Head of the Egyptian Pharmaceutical vigilance Center and the Head of the Arabic higher technical committee for medicines for his kind advice and support. Authors also thanks members of lab data unit in El Minia Psychiatric Hospital for their kind support.
List of Abbreviations
- (FDA: Food drug administration; RBC: Red blood cell; MCV: Mean cell volume; MCH: Mean cell hemoglobin; Hb: Hemoglobin; TNF: tumor necrosis factor)
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML