-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
2014; 2(1): 11-15
doi:10.5923/j.ijcp.20140201.03
Schizoaffective Disorder: An overview
Yogeswary K.
Student of Faculty of Medicine Udayana University, Department of Psychiatry Faculty of Medicine Udayana University
Correspondence to: Yogeswary K., Student of Faculty of Medicine Udayana University, Department of Psychiatry Faculty of Medicine Udayana University.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
This paper reviews the definition of schizoaffective disorder which is not well understood or defined as other mental health conditions. This is largely because schizoaffective disorder is a mix of multiple mental health conditions that may run a unique course in each affected person. Individuals who have a family history of schizoaffective disorder and women are significantly higher at risk. Diagnostic and Statistical Manual on Mental Disorder-5 is used as a guideline to characterize the disorder as well as to differentiate it from schizophrenia and other mood/affective disorders. The symptom depends on the two subtypes of schizoaffective disorder which includes the manic and depressive type. This paper also discusses the treatment needed to help patients cope with daily basis and improve their social skills. At the current situation there is no cure for schizoaffective patients, however treatments such as pharmacologic and non-pharmacologic which includes group counselling can help reduce worsening of symptoms in patients. Hence, an earlier detection enhances a better outcome.
Keywords: KeywordsSchizoaffective, Schizophrenia, Affective
Cite this paper: Yogeswary K., Schizoaffective Disorder: An overview, International Journal of Clinical Psychiatry, Vol. 2 No. 1, 2014, pp. 11-15. doi: 10.5923/j.ijcp.20140201.03.
Article Outline
1. Introduction
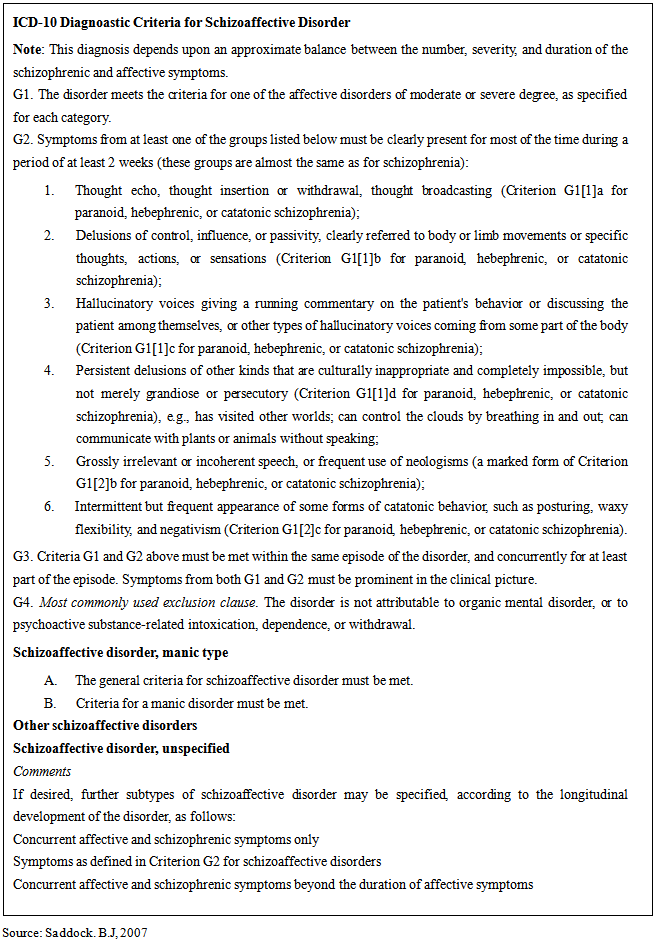
- According to Saddock, schizoaffective disorder has features of both schizophrenia and affective disorder. In current diagnostic systems, patients can receive the diagnosis of schizoaffective disorder if they fit into one of the following six categories. First, patients with schizophrenia who have mood symptoms; second, patients with mood disorder who have symptoms of schizophrenia; third, patients with both mood disorder and schizophrenia; fourth, patients with a third psychosis unrelated to schizophrenia mood disorder; fifth, patients whose disorder is on a continuum between schizophrenia and mood disorder; and finally, patients with combination of the above [1].Generally, schizoaffective disorder has been differentiated in several ways. It can be differentiated as an affective disorder with schizophrenic symptoms, schizophrenia with affective symptoms, a transitional step between schizophrenia and affective disorder in a continuum psychosis, a genetic intermediate form with a combination of schizophrenic and affective symptoms, a possible episode of schizophrenia and affective disorder in a continuum psychosis, a genetic intermediate form with a combination of schizophrenic and affective symptoms, a possible episode of schizophrenia and affective disorder in the same patient at the same time, and as an independent illness with its individual symptoms [2].Research Diagnostic Criteria (RSD) defines schizoaffective disorder as the acute occurrence of a full mood syndrome (depression and/ or mania) and one of a set of “core schizophrenic” symptoms such as bizarre delusions, first-rank symptoms or nearly continuous hallucinations at the same time [3].According to International Statistical Classification of Disease and Related Health Problems (ICD-10), schizoaffective disorder is a separate unit and can be used to patients who have co-occurring mood symptoms and schizophrenic-like mood-incongruent psychosis (Table 1) [1].
|
2. Aetiology
- Till date, the aetiology of schizoaffective disorder is remaining unknown. Thus, researchers believe that there are several factors involved. There are few studies designated to explore the causes that could lead to schizoaffective disorder. Those studies include role of gender, family history and so on [1].
2.1. Role of Gender
- Data from studies shows that females are at significantly higher risk for schizophrenia and other affective disorders compared to males [1]. However, this data is not completely reliable since, compared to males females are more prone to depression and need more familial factor to become ill [6].
2.2. Family History
- A study conducted to observe if there is any specific pattern of family history in persons with schizoaffective disorder compared with persons with bipolar disorder and schizophrenia. It was understood that there is no difference between male and female patients when impact of family history of psychiatric admission was examined. Besides, it was also found that schizoaffective disorder was equally strongly related with bipolar and schizophrenia among first-degree relatives [2, 6].
3. Signs and Symptoms
- A schizoaffective patient has severe mood changes and a number of the psychotic symptoms of schizophrenia, such as, hallucinations, delusions and disorganized thinking. Psychotic symptoms reflect the person’s failure to differentiate reality and imagination. Symptoms of schizoaffective disorder may different in each person and may can range from mild to severe. Symptoms of schizoaffective disorder are a sum of symptoms that appears in depression, mania and schizophrenia. The symptoms of depression are such as poor appetite, weight loss or gain, change in sleeping patterns, agitation, lack of energy, loss of interest in usual activities, feeling of worthlessness or hopelessness, guilt or self-blame, inability to think or concentrate, and thoughts of death or suicide. The symptoms seen in manic patients are inclusive of increased activity, including work, social and sexual activity, increased and/or rapid talking, rapid or racing thoughts, agitation, exaggerated self esteem, distractibility, and self-destructive or dangerous behaviour. Whereas the symptoms in schizophrenia are delusions, hallucinations, disorganized thinking, odd or unusual behaviour, slow movement or total immobility, poor motivation and problem with speech and communication [5].
4. Diagnosis and Differential Diagnosis
- If symptoms of schizoaffective disorder occur, a thorough physical examination and complete medical history will be performed by the doctor. A range of tests such as X-rays or blood tests will be used by the doctors to rule out a physical illness as the reason of the symptoms. If there is no physical reason for the symptoms, the patient may be referred to a psychiatrist or psychologist. Schizoaffective disorder is diagnosed if one has episodes of continuous illness and has, at some point, an episode of mania, major depression or combination of both while also having symptoms of schizophrenia [1, 7].So far, the DSM-V criteria (Table 2) is used as a basic tool in diagnosing patients with mood disorder. To diagnose schizoaffective disorder, DSM-V criteria require a continuous period of illness during which there is a Major Mood Episode concurrent with Criterion A of Schizophrenia: hallucinations, delusions, disorganized verbal communication, grossly disorganized or catatonic behaviour, or negative symptoms such as mild emotional affect. Throughout this period, hallucinations or delusions must be present for a minimum of 2 weeks in absence of Major Mood Episodes. At some time during the illness, there must be any of Major Mood Episode meeting DSM-V criteria as stated. Symptoms should not be due to the effects of drugs or alcohol or a common medical condition [8].Differentiating schizoaffective disorder schizophrenia and mood disorders can be difficult and confusing. The symptoms related to mood in schizoaffective disorder are unclear and persist longer than the symptoms in schizophrenia. Schizoaffective disorder maybe distinguished from a mood disorder by the fact that delusion and hallucination must be present in persons with schizoaffective disorder for at least two weeks in the absence of obvious mood symptoms. The diagnosis of a person with schizophrenia or mood disorder may change later to that of shizoaffective disorder, or vice versa [2].
|
5. Treatment and Prognosis
- It is important for a clinician to distinguish between schizoaffective disorder and schizophrenia or affective disorder to avoid misdiagnosis of patients. It is equally important to differentiate between the two types of schizoaffective disorder as the treatment varies. The issue that matters is not only about treating the patient but treating the patient with the most effective treatment plan. There is no cure for schizoaffective disorder, but treatment has been revealed to be effective in minimizing the symptoms and in helping the person better cope with the disorder and improve social functioning. Drug treatments, along with more psychosocial therapies, are often necessary to successfully treat schizoaffective disorder. Drug therapy usually can stop the patient's psychosis, but often only social and occupational rehabilitation therapies can overcome any associated problems such as unemployment, poverty and homelessness. The prognosis for schizoaffective patients mainly depends on the type of the disorder and the existence of a trigger. Improved treatment responds are seen in the bipolar type of the disorder than in the depressive type. Commonly, earlier detection of the disorder and total compliance of the medication gives more positive outcome. Treatment for schizoaffective patients can be categorized into two: pharmacologic and non-pharmacologic [1].
5.1. Pharmacologic
5.1.1. Antidepressants
- Selective serotonin reuptake inhibitors (SSRIs) are ideal over the other types of antidepressants. The adverse-effect profiles of SSRIs are lesser compared to other drugs’ profiles, therefore it promotes improved compliance [1]. However, it is suggested that antidepressants to be discontinued if psychosis worsens or if no improvements observed. Although there are side effects caused by the antidepressants, the risk seems to be minimal compared with the possible benefits of reducing distressing mood symptoms [3, 4]. It is also important for the clinicians to take into account previous antidepressant success or failure.
5.1.2. Antipsychotics
- A number of studies were performed to examine the effects of atypical antipsychotics on both type of schizoaffective disorder. Antipsychotics are said to be the best available treatment for patients with acute exacerbation schizoaffective disorder or schizophrenia with depressive symptoms. Results from three studies which were done to evaluate the effect of clozapine shows that patients with bipolar type improve better than the depressive type. Another open study proved that patients treated with clozapine also showed reduced suicidal behaviour [1, 3]. On the other hand, schizoaffective patients of depressive type show better progress to risperidone than those of bipolar type [3]. Antipsychotic medications, which has thymoleptic effects are said to be insufficient in overcoming mood disturbance in the disorder.
5.1.3. Mood Stabilizers
- This is also considered as an important treatment for schizoaffective patients. Lithium and carbamazepine are the examples of widely used mood stabilizers. When compared lithium with carbamazepine, it was found that carbamazepine was more effective in treatment of schizoaffective disorder, the depressive type [1].
5.2. Non-Pharmacologic Treatment
5.2.1. Psychotherapy and Counselling
- Building a trusting relationship in therapy can help individuals with schizoaffective disorder better understand their condition and feel hopeful about their future [1]. Effective sessions focus on real-life plans, problems and relationships. New skills and behaviours specific to settings such as home or workplace may also be introduced.
5.2.2. Family or Group Therapy
- Helping patients through education on illness, creating goals and dealing with daily problems associated with the disorder are the main purpose of the therapy. Families could deal better with loved ones through family therapy. Treatment can be more effective when schizoaffective patients are able to discuss their real-life problems with others. Supportive group settings can also help decrease social isolation and provide a reality check during periods of psychosis [4].
6. Suggestion
- Patients who are considered as threat for themselves as well as to the society should be hospitalised immediately. Community services plays vital role in helping patients to overcome the stigma after discharged from hospital. Specialised services might be required which include services such as community psychiatric nursing, occupational therapy, pharmacy delivery services and guidance in managing financial affairs.
7. Conclusions
- After discussing the points of view, it can be concluded that schizoaffective disorder is a combination of two illnesses which are schizophrenia and mood or affective disorder. Besides, schizoaffective disorder is a variation of schizophrenia but the exact cause still remains unknown. The symptoms of schizoaffective disorder are a sum of symptoms that emerges in schizophrenia. This disorder can be categorized into manic and depression type. However, since the symptoms of schizoaffective disorder are similar to schizophrenia and bipolar, this makes it difficult to be diagnosed. The diagnosis may take some time as it is difficult to tell the differences between schizoaffective disorder, schizophrenia and mood disorders. Usually, schizoaffective disorder can be diagnosed when the symptoms of mood disorder and schizophrenia are present simultaneously for a minimum of two weeks. Treatment for schizoaffective patients can be categorized into two: pharmacologic and non-pharmacologic. Antipsychotics, mood stabilizers and antidepressant are used in pharmacologic treatment. The effect of each drug varies according to the type of schizoaffective disorder. Apart from the pharmacologic treatment, non pharmacologic also plays an important role as an effective treatment such as psychotherapy and counselling which includes family or group therapy to help patients feel more confident in performing their daily basis routine. Besides, the goal of counselling is to help support individuals with schizoaffective disorder to understand their condition better and manage everyday problems related to this disorder. Patients who are considered as threat for themselves as well as to the society should be hospitalised immediately. Specialised services such as community psychiatric nursing, occupational therapy, pharmacy delivery services and guidance is required in managing financial affairs. The prognosis of schizoaffective patients is mainly dependent on the type of the disorder and the occurrence of trigger. Therefore, it is important that a schizoaffective patient is treated and diagnosed as early as possible in order to have a better outcome. However, more studies should be performed with big sample sizes to explore the disease efficiently.
ACKNOWLEDGEMENTS
- First of all, I would like to show my gratitude to the lord because with his blessings I have managed to complete this paper on schizoaffective disorder.With pleasure, I, Yogeswary Karpayah, would like to convey my heartiest thank you to Dr. Lely Setyawati, the supervisor for my paper work whose encouragement, guidance, and support from the initial to the final level enabled me to develop an understanding of the topic and successfully complete it.I would like to apologize if there are any weaknesses that could be found in my report and I would be glad to get feedbacks from the readers as it would help me in improvising myself in time to come. Last but not least, I hope that my writing would be beneficial to the readers as how it was to me.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML