-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
2013; 1(1): 20-23
doi:10.5923/j.ijcp.20130101.03
A Screening for Presence of Psychological Distress among Undergraduate Medical Students of a Medical College in Rural North-West India
Madhvi Kaistha, Sunil Kumar Raina, AK Bhardwaj, Vishav Chander, Dinesh Kumar, Sushant Sharma
Dr. Rajendra Prasad Government Medical College, Kangra, Himachal Pradesh, India
Correspondence to: Sunil Kumar Raina, Dr. Rajendra Prasad Government Medical College, Kangra, Himachal Pradesh, India.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Medical practitioners seem to suffer unacceptably high levels of psychiatric illness, depression and suicide, dependence on alcohol and drug abuse. The fact that they are aware of the existence of such medical conditions, they do not seek the kind of professional help for themselves as they would provide for their patients. However processes need to be in place to care of them. The aim of the study was to retrieve knowledge on psychological distress using GHQ-12 screening questionnaire. For this a cross sectional study was conducted on undergraduate medical students of a medical college located in the rural area of North West India using a self-administered General Health Questionnaire (GHQ-12) as a tool for assessment of psychological distress.90 students (43%) turned positive on screening. The prevalence of psychological distress was found to be higher among the male students. The study points to a need of providing attention to medical students during their entire tenure with special attention during exam times.
Keywords: Screening, Undergrauate Medical Students, GHQ-12
Cite this paper: Madhvi Kaistha, Sunil Kumar Raina, AK Bhardwaj, Vishav Chander, Dinesh Kumar, Sushant Sharma, A Screening for Presence of Psychological Distress among Undergraduate Medical Students of a Medical College in Rural North-West India, International Journal of Clinical Psychiatry, Vol. 1 No. 1, 2013, pp. 20-23. doi: 10.5923/j.ijcp.20130101.03.
1. Introduction
- Studies all over the world have shown that medical practitioners seem to suffer unacceptably high levels of psychiatric illness, depression and suicide, dependence on alcohol and drug abuse.[1-4] Although these problems may develop over many years, there is evidence that mental distress during medical school predicts later problems in physicians.[5, 6]Repeated evidence that medical students are subjected to considerable stress has been published over the last decades[7-10], which in addition to the personal suffering of the individual doctor might negatively affect patient care[11]. It is known that physicians do not seek the kind of professional help for themselves as they would provide for their patients[12-15]. Medical students seem to adopt a similar behaviour[16, 17]. However, we know little about the prevalence of clinically significant mental distress in our set up. Knowledge about presence of psychiatric conditions is important in itself and if found, needs attention. While burnout or stress-reactions are conceived of as reactions to a pressing environment, psychiatric disorders such as bipolar disorder, depression, anxiety are considered inherently multi-factorial, with e.g. hereditary contributions. The present study was undertaken among undergraduate medical students of a medical college in rural northwest India, with the aim of retrieving knowledge on psychiatric morbidity using GHQ-12 screening questionnaire.
2. Methodology
- A cross sectional study was conducted on undergraduate medical students of a medical college located in the rural area of North West India for a period of one month (through November 2012). The college has a total strength of 350 undergraduate students with 50 students in batches 2008, 2009 and 2010 and 100 students in batch 2011 and 2012 (first year).All undergraduate medical students, with the exception of first year medical students were invited to participate. Thus out of a total of 350 students, 250 were invited to participate in the study. The purpose of the study was explained to each student, and those students who agreed to participate in the study were included. Participation was voluntary and applied only to the students who were present in class on the day of assessment. All students already diagnosed and under treatment for psychiatry disorders were excluded from the study. 212 students were finally included in the study giving us a participation rate of 85%.The study was carried out during the month of September 2012. Data was collected after obtaining the necessary approval from the college authorities. A self-administered General Health Questionnaire (GHQ-12) was used as a tool for assessment of psychological distress. General health questionnaire is short (takes 5-10 minutes) and is straightforward to complete. The questionnaire comprising of 12 questions assesses general and psychological health during past one month. Each question had 4 responses which were scored as 0, 1, 2 and 3. Total scores of more than 12 was accepted as positive for psychological distress.For content validity, the questionnaire was pretested on 10 volunteer medical students, 2 junior residents and 2 faculty members. They commented on the relevance and unambiguity of items.
3. Results
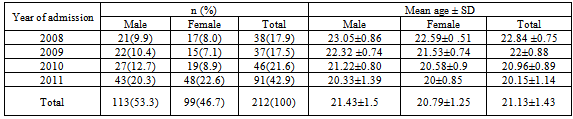
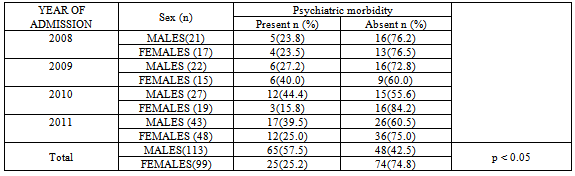
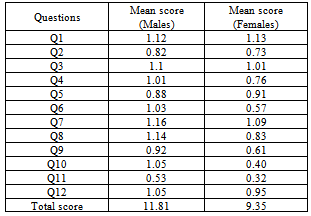
- Out of 212, 113(54.1%) were male students with mean age 21.43±1.5 and 99(45.9%) female students with mean age 20.79±1.25 as shown in table 1. As expected highest number of students (91) belonged to batch 2011.Based on the GHQ-12 scores, as shown in table 2, 90 students (43%) turned positive for. The prevalence of psychological distress was found to be higher among the male students. Out of 113 males, 65(57.5%) were found suspects of a psychiatric morbidity as compared to the females wherein only 25(25.2%) were found positive on GHQ-12. This was found to be statistically significant (p<0.05) The year wise prevalence rate for stress shows that batch 2008 (senior most batch studied) had the lowest prevalence of 23.6%. Prevalence was higher in junior batches, 2009 and 2010 with a rate of 32% and 42% respectively. Interestingly 2011 batch (the junior most batch studied showed a lower prevalence at 32%. A look at the mean scores of students reveals an interesting finding. The mean score for male students was 11.81 (less than the cut off of 12), while for female students, it was at much lower 9.35.
|
|
|
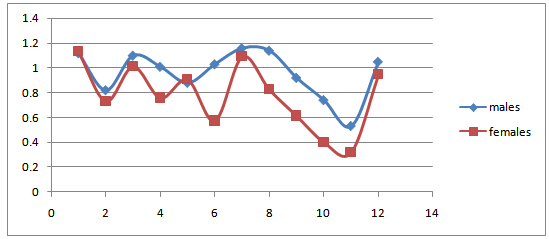 | Figure 1. A line diagram depicting mean scores for different questions |
4. Discussion
- In our study overall response rate was 84.6%. High response rate in our study is similar to the 70%–80% response rate obtained by other studies.[18, 19]Medicine as a profession has always been regarded as a popular choice for professional education.[20] This makes medical profession, may be even more competitive and stressful for students.[21]Studies on stress prevalence suggest that stress among medical students ranges from 30% to 50%.[20,21-25,26,27] and level of stress has been found to be higher in comparison to that of the general population[18] and that of students in other courses of study.[21,22] This becomes important in view of the fact that excessive exposure to stress causes physical and mental problems[28], and therefore it is important to detect stressed students earlier in order to prevent deleterious long-term effects of stress on the students.[18,20,22,24].In our study, we found a lower prevalence of psychological distress among final year students (senior most batch) at 23.6% in comparison to students in other years of study. This may possibly be because senior students have been able to develop skills to manage studies better. Our study also showed that the highest prevalence of psychological distress was found among medical students of batch 2010. This was an interesting finding because this batch was to go into examination within one month of the conduct of the study. Another area that needs to be worked out in reducing psychological distress among medical students is proper career counseling. It may be that students who are not really fit for medical studies because of its complexity may experience stress as a result of their lack of skills.Inspite of the limitations offered in the cross sectional nature of this study, it does point to a need of providing attention to medical students during their entire tenure with special attention during exam times. The college has already been working in this field and counselling sessions are a regular feature during the first year of medical college. This effort needs to be strengthened by providing intervention in the form of a structured orientation programme that addresses issues such as expectations for each year in medical college.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML