-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Clinical Psychiatry
2013; 1(1): 17-19
doi:10.5923/j.ijcp.20130101.02
Epilepsy in Pregnancy with Hospital-Acquired Pneumonia
Amer Hayat Khan1, Siti Rahmah Hashim2, Imran Khan3, Ashfaq Ahmad1
1School of Pharmaceutical Sciences, Universiti Sains Malaysia
2Department of Surgery, School of Medical Sciences, Universiti Sains Malaysia, Health Campus, Kelantan, Malaysia
3Psychiatry Unit, Khyber Teaching Hospital, Peshawar, KPK, Pakistan
Correspondence to: Amer Hayat Khan, School of Pharmaceutical Sciences, Universiti Sains Malaysia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Epilepsy and Pneumonia both show rare but high mortality rates in mother as well as in foetuses. Drug therapy is highly challenging. A 29 years old Malay lady was referred to Hospital Universiti Sains Malaysia from a primary care hospital, presenting with epilepsy and 29th weeks of pregnancy. Upon arrival, the patient developed 2 episodes of up rolling eyeball; starring and the events were resolved with IV Diazepam 5mg. During the hospital stay the patient contracted hospital acquired pneumonia and abdominal pain. Anti-epileptic drugs (AED) are positive evidence of human foetal risk. Currently, patients having uncontrolled seizures, tend to deteriorate with enhanced incidence of co-morbidity. Multiple physiological changes occur during pregnancy which influence drug disposition, volume of distribution, renal elimination, altered hepatic enzyme activity, and decline in plasma protein concentrations. Drug interactions are common issues with the present condition. Anti-epileptic drugs can cause congenital malformation; they may be used in a scenario where benefits outweigh the risk of AED use in such patients. Drug-drug interaction is another issue that should be monitored to avoid any complication or adverse drug reactions.
Keywords: Epilepsy, Pregnancy, Hospital-Acquired Pneumonia
Cite this paper: Amer Hayat Khan, Siti Rahmah Hashim, Imran Khan, Ashfaq Ahmad, Epilepsy in Pregnancy with Hospital-Acquired Pneumonia, International Journal of Clinical Psychiatry, Vol. 1 No. 1, 2013, pp. 17-19. doi: 10.5923/j.ijcp.20130101.02.
1. Introduction
- Epilepsy is a disorder that is best viewed as a symptom of disturbed electrical activity in the brain, which may be contributed to by many aetiologies. The literature reports the incidence of epilepsy in males is 49 cases per 100,000 person per years, whereas in females it is 41 cases per 100,000 persons per year.[1] Although, there are some genetic disorders associated with epilepsy, eclamptic seizures in pregnancy can only occur in females. [2]Katz and colleague reported that, approximately 1 million women of childbearing age in the United States have seizure disorders, among these only 20,000 give birth each year. Concerns during these pregnancies include the risk of foetal malformation, perinatal death, miscarriage, and increased seizure frequency.[3] Many factors have been shown to precipitate seizures in susceptible individuals. Excessive sleep, sleep deprivation, sensory stimuli, emotional stress and hormonal changes during the time of menses, puberty or pregnancy have been associated with the onset or an increased frequency of seizures. Certain drugs (theophylline, antidepressants) also have been associated seizureprovokation. Perinatal injuries and low gestational weight at birth are also risk factors for developing partial-onset seizures. However, immunization has not been associated with increased risk of epilepsy.[2,3]Among pregnant women, the volume of distribution and the hepatic metabolism of Antiepileptic drugs (AEDs) are increased; there is reduced bioavailability; significantly reduced compliance to medication; as well as fear of risk to the foetus. All these factors lead to increase in seizure frequency, which is observed in 17-33% of pregnancies.[3]A population-based study conducted in Norway reported that pregnant women with epilepsy had a lower risk of complications but an increased risk of induction, caesarean delivery, and postpartum hemorrhage.[4] The exact incidence of pneumonia during pregnancy is difficult to obtain and there is variation from 6.3 per 1000 deliveries to 8.5 per 1000 deliveries being reported. The mortality rate with Pneumonia has been cited as the third most frequent cause of indirect obstetric death in North America.[5] Mothers with pneumonia are significantly more likely to deliver before 34 weeks gestation, with preterm delivery occurring in up to 43% of cases.[6]
2. Case Presentation
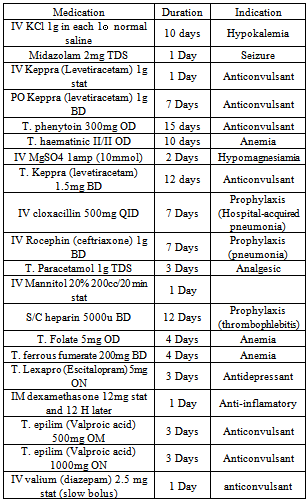
- A 29 years old Malay lady was referred to Hospital Universiti Sains Malaysia (Tertiary level health care unit) from a primary care unit, and presented with epilepsy at the 29th week of pregnancy. The patient reported of feeling lethargic and had a decreased oral intake for the prior 3 days associated with headache, but denied fever. Upon arrival, the patient developed 2 episodes of up rolling eyeball and starring and the events were resolved with IV Diazepam 5mg.The patient had been diagnosed with epilepsy since 6 years of age and was currently on Valproic aid (Tablet Epilim) 600mg TDS. Two weeks previously the patient had been admitted to hospital because of a breakthrough seizure. The patient had a history of double depression secondary to dis-harmony and violence from previous marital life. The current pregnancy was her 3rd, whereas the previous pregnancies were successfully delivered without any complications.During the admission, patient experienced several events of fitting over a period of four weeks. The fits occured at least twice a day, and were noticed through a twitching on her face and the upper limbs. The episodes usually lasted for around 30-60 seconds per event and were self-aborted. The fits were resolved and no events of fits were reported afterwards.
|
3. Discussion
- Anti-epileptic drugs (AED) fall into Category D according to the United States of America, FDA for pregnancy which indicates a positive risk to the human foetus. It is clear that anti-epileptic drugs taken in the first 18weeks of pregnancy can cause a slightly increased risk of serious congenital abnormalities in the baby.[7] Some recent data have indicated higher malformation rates with exposure to valproic acid compared with some other major AEDs. The teratogenic effects of valproic acid appear to be dose dependent, with higher risks at dosage levels >1000 mg/day. Poly-therapy involving treatment with more than one AED also seems to be associated with an increased risk of birth defects compared with monotherapy. [8] Thus, in pregnancy clinical evidence suggests using valproic acid as first-line monotherapy in primary generalised epilepsy, and lamotrigine or topiramate as second line alternatives. Although lamotrigine maybe safer, it may not be as effective as valproate. However seizures in pregnancy may harm both mother and baby. Women who do not take AED’s while pregnant will obviously have less risk of adverse effects from AED’s but they will also have a far greater risk of experiencing seizures during their pregnancy which in turn can cause harm to both the mother and her baby.[9] Pregnancy has a variable effect on the frequency of seizures. Although there are controversies, in the majority of cases pregnancy was found to increase the frequency of seizures.[8]Based on this patient’s medication chart, there are several drug-drug interactions that require monitoring. Phenytoin is reported to have interaction with diazepam. This interaction happens because phenytoin induces the metabolism of drugs that are substrates for CYP2C, CYP2D, and CYP3A. However, phenytoin is eliminated predominantly by CYP2C9-and CYP2C19-dependent hepatic metabolism. Drugs extensively metabolized by CYP2C19 could potentially influence phenytoin elimination by acting as an alternate substrate for this iso-enzyme. Thus, this may increase the serum concentration of phenytoin.[10] The combination of diazepam and levetiracetam has been reported to have anticonvulsant actions even though both drugs are given at doses far lower than their therapeutic levels.[11] Although there is evidence that folic acid can cause a decrease in phenytoin serum concentration to sub-therapeutic levels, it has been suggested that folate supplementation should be initiated whenever phenytoin therapy commences because of the hypothesized cofactor mechanism, and better seizure control with no perturbation of phenytoin pharmacokinetics.[12,13] Total phenytoin concentration is reported to fall during valproateadministration which may be due to redistribution of the drug being displaced by valproate for plasma protein binding, thus enhancing the clearance of phenytoin.[14]Guidelines from the British Thoracic Society for the management of pneumonia in adults especially in pregnancy, recommends that Penicillin, macrolid, and cephalosporin are likely to be the optimal antibacterial agents. These antibiotics have a good safety record in pregnancy.[5]
4. Conclusions
- A patient is diagnosed with double depression secondary to violence from her previous marriage. The medication given to her is necessary to control her recurring break through seizures which may endanger her and the baby’s health. Anti-epileptic drugs may cause congenital malformation. Drug-drug interaction is another issue that should be monitored to avoid any complication or adverse drug reactions. Pneumonia during pregnancy needs more research to clarify the risk factors and outcomes on patient and foetus.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML