-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Brain and Cognitive Sciences
p-ISSN: 2163-1840 e-ISSN: 2163-1867
2022; 10(1): 1-7
doi:10.5923/j.ijbcs.20221001.01
Received: Nov. 17, 2022; Accepted: Dec. 5, 2022; Published: Dec. 14, 2022

Comparative Evaluation of the Results of Conservative and Surgical Treatment of Patients with Hypertensive Intracerebral Hemorrhages (HIH)
Maksudova L. B.1, Gafurov B. G.2
1Republican Research Center of Emergency Medicine, Tashkent, Uzbekistan
2Center for the Development of Professional Qualifications of Medical Workers, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The authors carried out a comparative analysis of the results of conservative and surgical treatment of 140 patients with hypertensive intracerebral hemorrhages (52 female and 88 males). The mean age was 58.8±14.0 years. The results of the study showed that the 30-days survival rates in patients with hypertensive intracerebral hemorrhages depended on many factors and required a multimodal approach in choosing one or another treatment method.
Keywords: Hypertensive intracerebral hemorrhages, Comparative analysis
Cite this paper: Maksudova L. B., Gafurov B. G., Comparative Evaluation of the Results of Conservative and Surgical Treatment of Patients with Hypertensive Intracerebral Hemorrhages (HIH), International Journal of Brain and Cognitive Sciences, Vol. 10 No. 1, 2022, pp. 1-7. doi: 10.5923/j.ijbcs.20221001.01.
1. Introduction
- The incidence of hypertensive intracerebral hemorrhages averages 20 cases per 100,000 population, with a lethal outcome exceeding 40%, and most of the surviving patients have a persistent neurological deficit with an unsatisfactory functional outcome [19]. To this day, the question of choosing the tactics of treating patients with HIH remains debatable, namely, a conservative or surgical approach in a particular case. In the world literature, there are many conflicting data on the viability of the medulla around the hematoma. The advantage of surgical treatment is justified by the fact that after removal of the hematoma, the perfusion of the medulla around the hematoma bed improves due to its evacuation [8,10-12,15,16,20]. However, the results of numerous randomized studies contradict the above theory, since the surgical intervention itself is an additional factor of aggression, which causes aggravation of vascular spasm, an increase in edema around the hematoma bed, which leads to a persistent unsatisfactory functional outcome [5,7,21]. In one of the recent prospective randomized trials, better 30-day survival rates in patients with HIH were observed with conservative treatment compared with surgery.The lack of consensus in the approach and choice of treatment tactics, the lack of knowledge of CT morphometric parameters of HIH, a comparative assessment of 30-day survival after conservative and surgical treatment shows the relevance and debatability of this direction.
2. Material and Methods
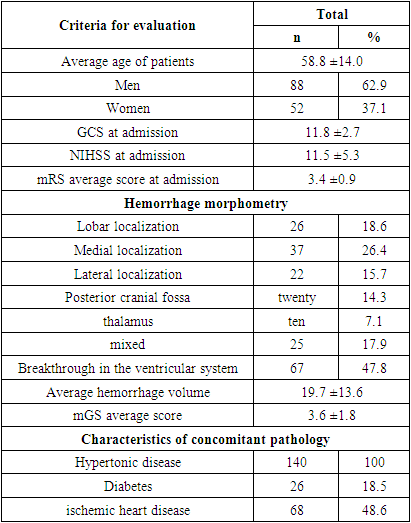
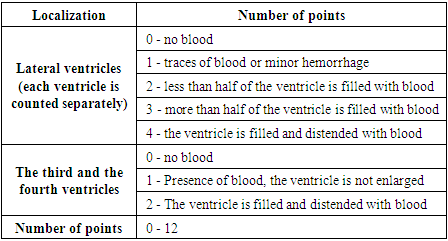
- We carried out a retrospective analysis of 140 patients with HIH of the brain. (Table 1). Of these, 52 (37.1%) patients were female and 88 (62.9%) male, aged 15 to 88 years. The mean age was 58.8±14.0 years. All patients underwent a neurological examination and an assessment of the severity of the condition using the National Institutes of Health Stroke Scale (NIHSS) and the modified Rankin scale (mRs) (Table 1). The level of consciousness was assessed using the Glasgow Coma Scale (GCS) (Table 1). After studying the anamnesis and physical examination, all patients underwent multislice computed tomography (MSCT). MSCT morphometry included an assessment of such indicators as the location and volume of the hematoma, the presence of a breakthrough of blood into the ventricular system, the state of the bypass cistern, deformation or expansion of the ventricular system and its size, displacement of the midline structures of the brain, perifocal edema around the hematoma, if any, and secondary brain changes (Table 1). When assessing the spread of IVH, we used the modified Graeb scale (mGS) (Table 2). The inclusion criteria for this study were as follows:- hematoma volume up to 40 cm3;- the presence of compression of the bypass tank;- the presence of compression of the ventricular system;- the presence of displacement of median structures.The exclusion criteria were the following:- refusal of surgical intervention (refusal of the patient's relatives and patients with impaired level of consciousness according to GCS <7 points).
|
|
3. Results and Discussions
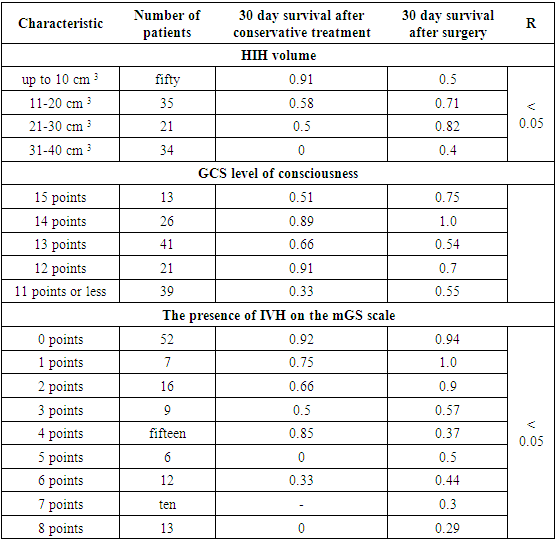
- The large-scale STICH II study did not find strong evidence to support the hypothesis of improved outcomes after early surgery compared with conservative treatment in the category of patients with an impaired GCS level of consciousness <14 points. However, there was a statistically significant positive result in the direction of early surgery compared with conservative therapy in patients with a GCS level of consciousness >13 points without signs of IVH and lobar localization [13]. However, there is a trend of expectant management by some surgeons in patients with less severe neurological deficits and CT morphometry parameters, the absence of high mGS scores, pronounced compression of the bypass cistern and brain mass effect, as well as correctable arterial hypertension [13]. We carried out a comparative analysis of the 30-day survival of patients with IVH depending on the volume of IVH, the level of consciousness and CT morphometry, which were analyzed according to the inclusion criteria in this study after conservative and surgical treatment. Of the 60 patients with conservative treatment of IVH, in 70% (n=42) cases, the volume of IVH was up to 10 cm3, in 18.3% (n=11) cases - 11-20 cm3, in 6.6% (n=4) cases - 21-30 cm3, in 5% (n=3) the volume of HVMK was from 31 to 40 cm3. Evaluation of 30-day survival rates in patients with IVH depending on the volume showed that in patients with IVH volume up to 10 cm3, 30-day survival was 0.91, with a volume of 11-20 cm cm3 - 0.5, with a volume of 31-40 cm3 - 0. An analysis of 30-day survival rates in patients with HIH after surgery showed a trend towards an increase in survival rates as the volume of HIH increased, which indicates the effectiveness of surgical intervention. Thus, in patients with HIH volumes up to 10 cm3, 11–20 cm3, and 21–30 cm3, the 30-day survival rate was 0.5, 0.71, and 0.81, respectively. It should be noted that the 30-day survival rate in the subgroup of patients with HIH volume of 31-40 cm3 after surgery increased to 0.4 compared with conservative therapy. These results indicate a significant correlation between the volume of HIH and 30-day survival. (p<0.05) (Table 3 and Figure 1 A and B).
|
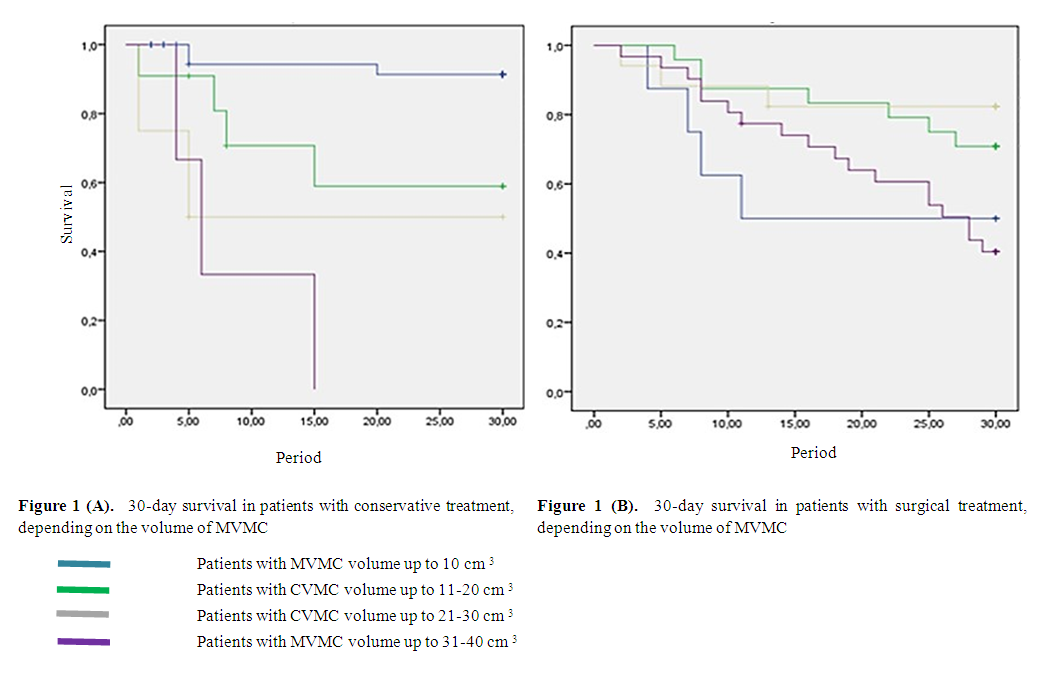 | Figure 1 |
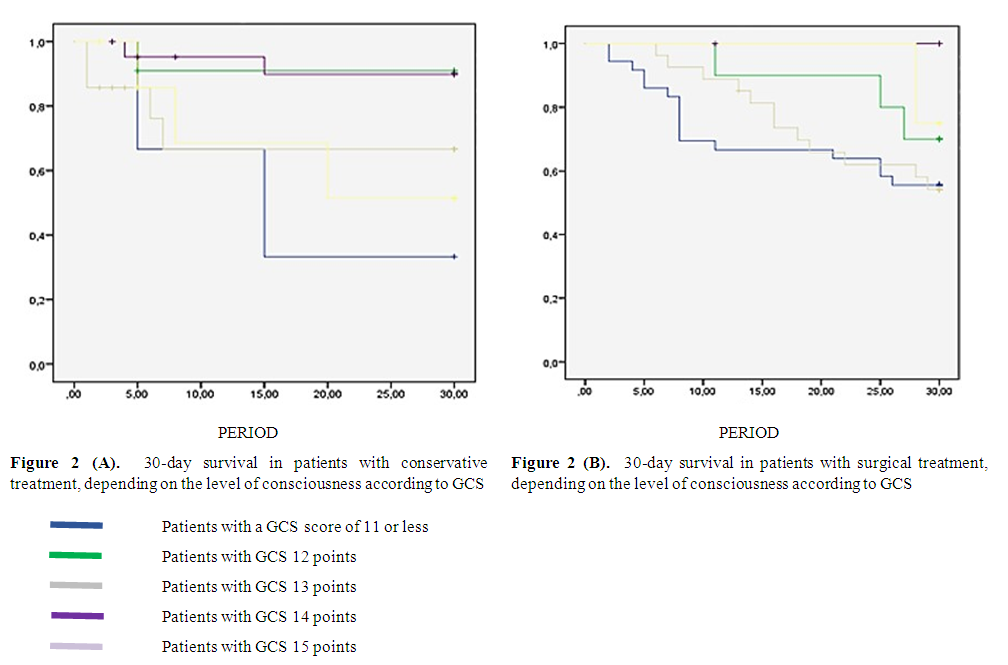 | Figure 2 |
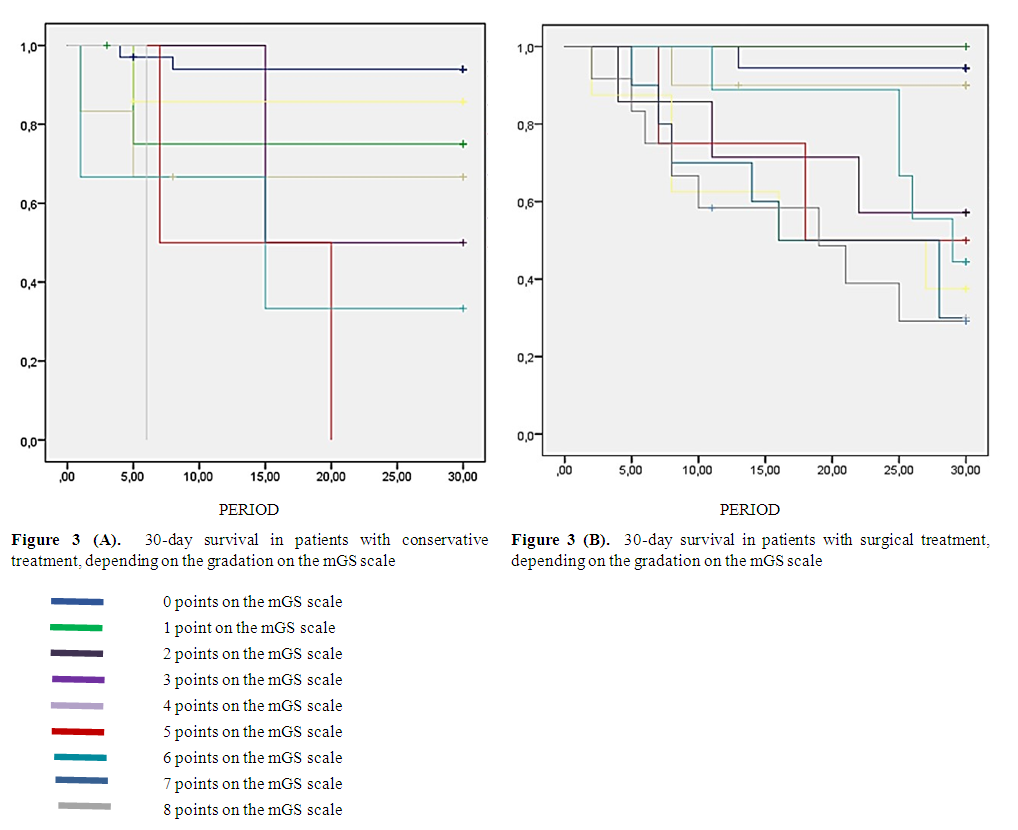 | Figure 3 |
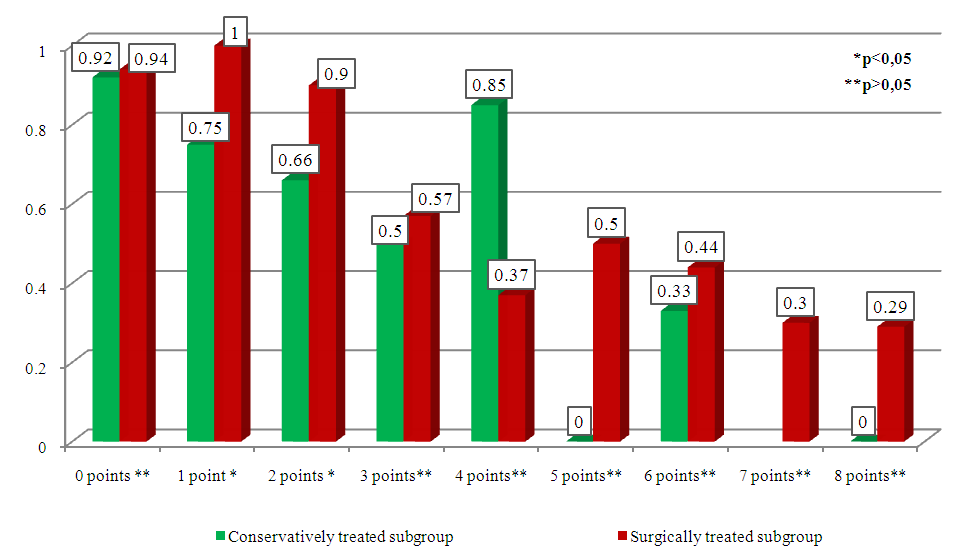 | Figure 4. Comparative assessment of 30-day survival of patients depending on the degree of gradation according to the mGS scale |
4. Conclusions
- Thus, based on the study, we can conclude that the 30-day survival rates in patients with HIH depend on many factors, such as the initial level of consciousness according to GCS, neurological deficit according to the NIHSS scale, as well as CT- morphometric indicators, namely, the localization of the HIH, the volume of hemorrhage and the degree of gradation of intraventricular hemorrhage according to the mGS scale. The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML