-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Applied Psychology
p-ISSN: 2168-5010 e-ISSN: 2168-5029
2021; 11(3): 72-87
doi:10.5923/j.ijap.20211103.02
Received: Oct. 13, 2021; Accepted: Nov. 1, 2021; Published: Nov. 15, 2021

Feeling of Collective Historical Victimization and Attitude towards Clinical Trials of Covid-19 Vaccines in the African Context: The Moderating Role of Anti-Western Emotions and Cognitions
Gustave Adolphe Messanga1, Achille Vicky Dzuetso Mouafo2, Sonia Npiane Ngongueu1, Laurine Elvira Memou1
1Department of Philosophy-Psychology-Sociology, University of Dschang, Cameroon
2Department of Philosophy and Psychology, University of Maroua, Cameroon
Correspondence to: Gustave Adolphe Messanga, Department of Philosophy-Psychology-Sociology, University of Dschang, Cameroon.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The objective of this research is to analyze the link between the past of victimization and subsequent intergroup attitudes and behaviors in the specific field of health. It tests the hypothesis that anti-Western emotions and cognitions (hatred, anger, fear, mistrust, disgust, suspicion, discrimination, stereotypes and prejudices) have a moderating effect on the link between the feeling of collective historical victimization and the attitude towards clinical trials of vaccines relating to Covid-19 in the African context. To do this, the scales of feeling of collective victimization (α= .76), mistrust (α= .76), anger (α= .85), fear (α= .74), intergroup disgust (α= .50), attitudes towards clinical trials of vaccines (α= .72), hatred (α = .79), suspicion (α= .78), discrimination (α= .65), prejudices (α= .36), and stereotypes (α= .31) were administered to 369 participants including 167 women and 205 men. Their age was between 17 and 45 years (M= 22.05; SD= 3.32). The observations made provide empirical support for this prediction. They contribute to the literature on explanatory factors of attitudes towards clinical trials of drugs and vaccines.
Keywords: Feeling of historical victimization, Clinical trials of vaccines, Covid-19, Anti-Western emotions, Anti-Western cognitions
Cite this paper: Gustave Adolphe Messanga, Achille Vicky Dzuetso Mouafo, Sonia Npiane Ngongueu, Laurine Elvira Memou, Feeling of Collective Historical Victimization and Attitude towards Clinical Trials of Covid-19 Vaccines in the African Context: The Moderating Role of Anti-Western Emotions and Cognitions, International Journal of Applied Psychology, Vol. 11 No. 3, 2021, pp. 72-87. doi: 10.5923/j.ijap.20211103.02.
Article Outline
1. Introduction
- Many diseases have wiped out entire populations around the world (Cartwright, 1977). Researches are usually conducted to find treatments and/or vaccines to reduce their spread. In this vein, the literature reveals that to recruit experimental subjects for clinical trials, Africa is constantly solicited by Westerners (Noko, 2020). That is why it has long been considered the guinea pig of Big Pharma who are attracted by low costs and controls. Their products can be tested there with disregard for patients’ safety (Chipaux, 2005). It is therefore not surprising that these trials have caused the deaths of thousands of Africans or left many of them severely affected. This is particularly the case with clinical trials of Trovan, Tenofovir, Nevirapine or Combifivir (Weipzig & Schipper, 2008).It can be suggested that the memory of deaths engendered by clinical trials could generate a feeling of collective historical victimization among Africans. This feeling refers to a state of mind shared by members of a group, which results from intentional, unjust and immoral harm with serious and lasting consequences inflicted by one or more outgroups (Bar-Tal et al., 2009). It is caused by the sufferings experienced by ingroup in the distant past (Schori-Eyal et al., 2014). These sufferings are embedded in collective memory and guide groups’ cognitions, emotions, attitudes and actions (Connerton, 1989). In the field of health, this feeling is fueled by conspiracy theories that generally arise with new pandemics and their vaccines (Van Prooijen & Douglas, 2017).Conspiracy theories are defined as an attempt to explain the ultimate causes of a significant social and/or political event based on certain circumstances which highlight the existence of a plot hatched by two or more powerful actors (Douglas et al., 2019). In Africa, these theories are partly based on the foundation of real experiences that collective memory has not obscured (Cessou, 2020). They flourish in times of social crises such as the onset of illness, since they correspond to high periods of uncertainty and collective fear (Van Prooijen & Douglas, 2017). Indeed, conspiracy theories were quickly developed around HIV/AIDS (Minard, 2007). They argued that this disease was created by the West to exterminate the black population of the United States and Africa (Pipes, 1997). Likewise, during the polio vaccination campaign in northern Nigeria in 2003, strong opposition was noted among parents of children of age to be vaccinated, due to their adherence to conspiracy theories that propagated the idea according to which the said campaign was in fact a program designed to inject sterilants and HIV/AIDS virus into the Muslim community, with the aim of killing its members (Yahya, 2007). Likewise, during the Ebola epidemic in Liberia in 2014, very powerful and widely held conspiracy theories argued that the virus that caused it was a biological weapon invented in a laboratory by the Westerners to infect and kill Africans; hence the fear and mistrust of the population towards the government and international partners (Abramowitz et al., 2017). The consequence of adhering to these theories is that they generate hostile emotions in Africans towards rulers and Westerners (Yahya, 2007).Research on collective victimization reports that when members of a group feel victimized or their group has been victimized in the past, they experience emotions, develop cognitions, and display negative actions towards the oppressive group (Kauff et al., 2017; Pennekamp et al., 2007). Indeed, collective victimization has a powerful impact on individuals’ emotions and beliefs, even when events took place in the distant past (Volkan, 2001). In this vein, the literature reveals that collective victimization leads to stereotypes and discrimination against the group considered to be the perpetrator of the pain inflicted (Fouka & Voth, 2019 ; Rozenas et al., 2017). This effect may extend to members of the group who have not suffered directly from this victimization (Lickel et al., 2006) through media (Paluck, 2009), school (Angvik & von Borries, 1997) or family (Lupu & Peisakhin, 2017) who transmit the memory of collective trauma from one generation to another. By way of illustration, observations made in Rwanda, Burundi and the Democratic Republic of Congo reveal that collective victimization transmits trauma from previous to subsequent generations, thus perpetuating negative intergroup attitudes (Vollhardt & Bilali 2015). It also induces prejudice and intergroup hostility. This is the case of Holocaust-induced victimization which created an antagonistic view of Jews and which, in turn, fueled anti-Semitic prejudices (Antoniou et al., 2020; Dinas et al., 2021).Prejudices against outgroups can induce different emotions (anger, fear, disgust, pity, and guilt) that direct and regulate intergroup behaviors (Mackie & Smith, 2018). In this vein, Barlow et al. (2012) suggest that the frequency of negative experiences predicts stigma and outgroup avoidance. These experiences can be damaging not only because they increase prejudice, but also because they reduce the tendency to interact with outgroup members in the future (Barlow et al., 2012; Hayward et al., 2017). In this vein, in relation to the clinical trials mentioned above, one can suggest that Africans might experience an anti-Western feeling, that is to say a broad opposition, prejudice or hostility towards the people, culture or policies of the Western world, especially in the field of health (Merriam-Webster, 2021).Anti-Western sentiment is fueled by anti-imperialism and is set against countries found guilty of colonial crimes in the past and/or present (Gettleman, 2006). For Africans specifically, this feeling results from the slave trade, colonization, racial discrimination, exploitation of resources that their communities suffered, as well as the many unethical clinical trials carried out by Westerners in the past that have caused mental and physical harm, and the death of thousands of Africans. In this vein, Lado (2005) underlines that white and black remain racial categories whose symbolic and emotional charge, nor the impact of the white man on the consciousness and attitudes of Africans, cannot be neglected. The latter reminds many Africans of the painful history of slavery, colonization, defeat, humiliation, domination and exploitation. This memory is associated with enslavement, subjugation, exploitation, humiliation, and even mass killings. This humiliating and disastrous memory caused an emotional shock among Africans which is reflected in the negative representations they now have of Westerners. These representations fuel the development of hostile cognitions and emotions towards them (anger, hatred or disgust) (Choma et al., 2013; Jasini et al., 2017).The literature reports that hostile emotions greatly influence Africans’ health behaviors as well as their attitudes towards clinical trials of new vaccines (Larson, 2019; Yahya, 2007). Indeed, the clinical trials of drugs that have taken place on the African continent have generated a fear of medicine even in countries where they did not take place. This fear resurfaces every time a medical project is initiated. This explains the low rate of medical research in sub-Saharan Africa (1.3% of the world total) when this region of the world contains almost 25% of diseases (Washington, 2007). Thus, Africans express mistrust of Western medicine. This has enormous consequences on their health behaviors. For example, the polio infection rate has increased in Nigeria, Chad and Burkina Faso. Negative emotions (anger, surprise) are at the origin of these attitudes (Noko, 2020). Attitudes towards clinical trials of Covid-19 vaccines are in this perspective. Their source is, in particular, the fact that the continent records fewer cases infected with Covid-19 compared to the European and American continents; indicating that Africa (8,465,147 cases of infection including 214,574 deaths as of October 11, 2021) is in a less worrying health situation than other continents such as Asia (77,234,756 cases of infection including 1,140,251 deaths on October 11, 2021), North America (54,402,296 cases of infection including 1,105,531 deaths on October 11, 2021) or Europe (60,524,778 cases including 1,246,446 deaths on October 11, 2021) (www.worldmeters.info/coronavirus/); hence the lack of understanding of populations as to the insistence on the need to resort to vaccination against this disease on the continent. This incomprehension was concretely manifested at the announcement of the clinical trials of the BCG vaccine against Covid-19. Indeed, after a video relayed on social networks where researchers from the french National Institute of Health and Medical Research (INSERM) explained the project to reinject the BCG vaccine to Africans in order to see its effectiveness against Covid-19, strong opposition was noted within the African community residing in Africa and outside the continent (Le Monde, 08 May 2020, 9:38).Covid-19 was discovered in December 2019 in Wuhan province in China (Roser et al., 2020). It is one of the components of a large family of viruses that cause illnesses ranging from a simple cold to more severe pathologies such as MERS (Middle East Respiratory syndrome) or SARS (Severe Acute Respiratory Syndrome). It is transmitted by the "Severe Acute Respiratory Syndrome Coronavirus 2" [SARS-CoV 2] (Murphy et al., 2021), which is transmitted mainly by postilions from sneezing and coughing. These symptoms (fever or feeling of fever, cough, and difficulty in breathing) can appear up to 14 days after contact. According to WHO (2020), most infected individuals recover without treatment. People who are elderly or have other conditions such as cardiovascular disease, diabetes and cancer are most likely to develop a severe form of this disease for which there is no cure yet (WHO, 2020). Faced with the growing number of people infected and the mortality rate, WHO has declared a public health emergency of international concern, thus raising Covid-19 to the rank of a pandemic (Cucinotta & Vanelli, 2020). The world currently totals more than two hundred and thirty-eight (238) million officially diagnosed cases of infection and nearly five (5) million deaths (data as of Monday, October 11, 2021; www.worldmeters.info/coronavirus/).Several vaccines are currently being administered to populations to protect them against Covid-19. These include vaccines from Pfizer-BioNtech, Moderna, Janssen (Johnson & Johnson), and AstraZeneca (Centers for Disease Control and Prevention [CDC], 2021). Due to the fact that these vaccines are still in development, they are not yet in their universal and final versions. Indeed, WHO considers them to be "emergency vaccines" because with the growing number of cases, the spread of the virus responsible for the disease had to be limited. That is why it recommends that people who have been vaccinated continue to wear the mask and respect physical distancing. The reason for this is that ignorance of the scope of protection that vaccines provide against disease, infection and transmission does not guarantee that vaccination exempts individuals from complying with barrier measures enacted at the onset of the pandemic to limit its spread. Likewise, it should be noted that more than two hundred (200) vaccines are still under development, of which more than sixty are in the clinical trial phase (WHO, 2020). In this vein, after the announcement of the first clinical trial of the vaccine against Covid-19 in Africa (the clinical trial of the BCG vaccine), the populations expressed strong opposition to its unfolding on the continent (Noko, 2020), undoubtedly because of the memory of the past experiences reported above and which fueled all kinds of conspiracy theories (Kouzy et al., 2020; Ngutjinazo, 2021).There are several determinants of attitudes of reluctance of individuals towards vaccination and clinical trials (Centre Européen pour la prévention et le contrôle, 2015). We can cite social media, lack of awareness, disinformation, lack of confidence in the institutions involved in vaccination; historical, socio-cultural, environmental, economic, political, psychological or health system/institutional factors; personal perception of the vaccine, specific aspects directly linked to vaccines or vaccination, people’s mistrust of the state and conspiracy theories (Damnjanovic et al., 2018; Hornsey et al., 2018 ; Johnson, 2000; Ketterer et al., 2013; Olpiński, 2012; Patty et al., 2017; Rieger & He-Ulbricht, 2020; Yaqub et al., 2014).For the specific case of Covid-19, the literature offers several explanatory factors for the attitudes of reluctance towards vaccination against this disease (Daisy & Steptoe, 2020). These include mistrust of vaccines, concerns about their unintended effects, preference for natural immunity, the media and communication environment, the perception of the pharmaceutical industries, the source of the vaccine, socio-demographic factors, lack of trust in governments, disinformation, psychological factors, past experiences, conspiracy theories, or the higher mortality rate in the West than in Africa (Islam, 2021; Kearney et al., 2021; Kouzy et al., 2020; Murphy et al., 2021; Ngutjinazo, 2021; Noko, 2020; Nyhalah et al., 2021; Roozenbeek et al., 2020; Van der Linden et al., 2020). However, no study, to our knowledge, evaluates the role that anti-Western cognitions and emotions play in the link between the feeling of collective historical victimization and the attitudes of individuals towards clinical trials of Covid-19 vaccines in the African context. In support of this research perspective, the literature on the feeling of collective victimization states that it generates negative intergroup emotions and cognitions which are the sources of hostile intergroup attitudes (Barlow et al., 2012; Hayward et al., 2017; Vollhardt, 2012). In this vein, the scientific project of the present research is to show that in the specific field of health, the feeling of historical collective victimization felt by Africans due to past experiences could lead them to develop anti-Western emotions and cognitions; which could affect their attitudes towards clinical trials of Covid-19 vaccines. It is this idea that is subjected to empirical verification.
2. Hypotheses
- The present study proposes that: Anti-Western emotions and cognitions have a moderating effect on the link between the feeling of collective historical victimization and the attitudes towards clinical trials of Covid-19 vaccines in the African context. Concretely, it is expected that: hatred, anger, fear, mistrust, disgust, suspicion, stereotypes, prejudices and discrimination generated by the feeling of collective historical victimization felt by Africans against Westerners because of the experiences of clinical trials of drugs and vaccines that have killed and severely disabled thousands of people on the continent since the colonial period, lead them to adopt a negative attitude towards clinical trials relating to vaccines against Covid-19.
3. Method
3.1. Participants
- To conduct this study, 369 students of both sexes were selected by the simple random sampling technique in different faculties of the University Dschang. Their age is between 17 and 45 years old. The choice of students is due to the fact that they have a high level of education which allows them to analyze social reality critically. They all agreed to participate in the research on a voluntary basis.
3.2. Material and Measurement
- Several psychometric instruments are used to assess the moderating effect of Intergroup Emotions (IE) and Cognitions (IC) on the link between the feeling of collective historical victimization (HFCV) and the attitude towards clinical trials of vaccines relating to Covid-19 in Africa (ATCTRCov-19V). The first is the HFCV scale (Schori Eyal et al., 2014). It has good reliability and a good factor structure (α= .767; KMO= .773; λα= 55.334; h2= .733). The second, for its part, evaluates the ATCov-19VT (Leslie & Keith, 2017). It has satisfactory metric characteristics (α= .722; KMO= .911; λα= 59.793; h2= .789). The first moderating variable, intergroup emotions, is evaluated by a scale comprising six (6) dimensions. These are: 1) Mistrust (Rusk, 2018; α= .767; KMO= .812; λα= 57.538; h2= .822); 2) Fear (Giner-Sorolla & Russell, 2019; Sternberg & Sternberg, 2008; α= .740; KMO= .714; λα= 57.541; h2= .877); 3) Anger (Giner-Sorolla & Russell, 2019; Sternberg & Sternberg, 2008; α= .853; KMO= .815; λα= 69.472; h2= .862); 4) Disgust (Hodson et al., 2013; α= .500; KMO= .643; λα= 67.362; h2= .850); 5) Suspicion (León et al., 2002; α= .789; KMO= .764; λα= 61.49; h2= .810); and 6) Hatred (Sternberg & Sternberg, 2008; α= .793; KMO= .769; λα= 55.21; h2= .828). The second moderating variable, intergroup cognitions, is evaluated on three (3) dimensions. The first addresses stereotypes (Tiwari et al., 2014; α= .310; KMO= .551; λα= 54.971; h2= .788). The second concerns prejudices (Tiwari et al., 2014; α= .363; KMO= .572; λα= 49.417; h2= .804). The third measures discrimination (Tiwari et al., 2017; α= .658; KMO= .638; λα= 65.777; h2= .696). Overall, the Intergroup Cognitions scale is reliable (α= .693; KMO= .727; λα= 58.66; h2= .677). The same is true for the Intergroup Emotions scale (α= .910; KMO= .716; λα= 82.651; h2= .890). All of these self-administered measures have acceptable sampling adequacy indices (KMO), good factor contributions (λα), and the items have good saturations. They are rated on a Likert scale ranging from 1 (Strongly disagree) to 7 (Strongly agree).
4. Results
- The results of this research are presented in three phases. The first puts into perspective the preliminary tests of the effects of interactions and covariations between the variables of the study and leads to the model of individual prediction (without moderation) of ATCTRCov-19V by IC, IE and HFCV and covariances (Figures 1, 2 and 3). The second is the first level of verification of the moderation of the interaction effect between HFCV and ATCTRCov-19V by IC and IE in the Multiple Linear Regression Model resulting in a model (Figure 4). The third phase is the second level of verification or confirmatory analysis of the hypothesis (Figure 5). It confirms the moderation of the postulated interaction effect by applying the Structural Equation Modeling, with the Robust Maximum Likelihood method under AMOS 23.0.
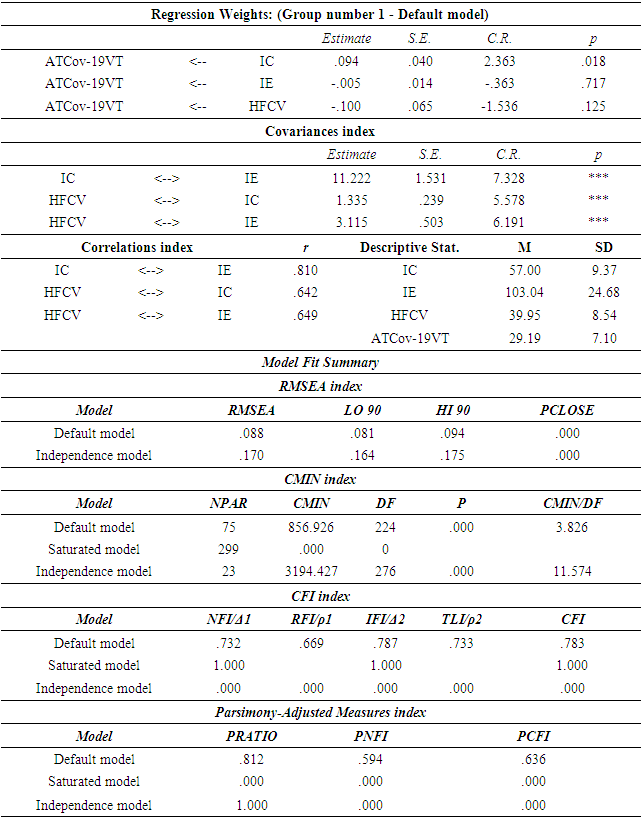
4.1. Covariations between Latent Variables Underlying Intergroup Cognitions and Their Interaction Effects with Attitudes towards Clinical Trials of Covid-19 Vaccines (ATCTRCov-19V)
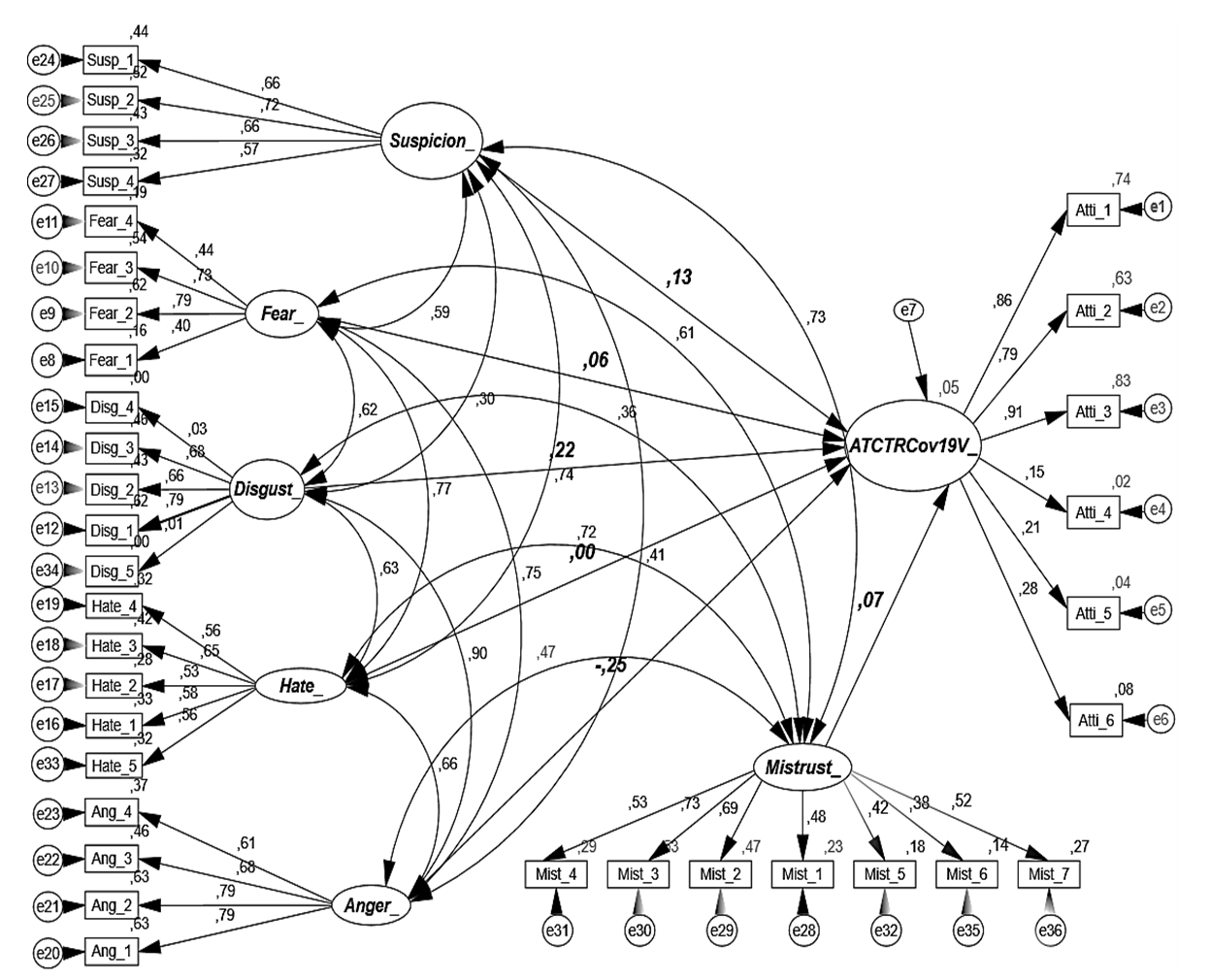
- IC and IE are latent factors underlying the interaction effect between feeling of collective victimization and attitude towards clinical trials of Covid-19 vaccines. Structural equation models are analyzed in order to estimate the interaction effects between these variables and the levels of covariation and to attest to their validity. To do this, the Robust Maximum Likelihood (RML) method in AMOS, an extension of SPSS 23.0 is used. A number of parameters meet the quality criteria of the model, as they make it possible to judge the quality of the statistically valid model from the point of view of the interaction effects between the latent and principal variables of the model. For a good model, the CMIN/DF index must be either below 5% (Byrne, 1989; Civelek, 2018) or below 3% (Civelek, 2018; Meydan & Şen, 2011). The index X 2 must be insignificant with the ratio X 2/df and must be close to 5 (Wheaton et al., 1977); the Root-Mean-Square Error of Approximation (RMSEA) must be less than or equal to .1 (10%) (Browne & Cudeck, 1993) and the PCLOSE strictly less than .5 (5%) (Lomax, 2010).The model in Figure 1 first indicates that the latent variables constituting IC (Stereotypes: M= 23.66, SD= 4.335; Prejudices: M= 23.47, SD= 4.565; Discrimination, M= 23.63, SD= 5.280) covariate positively, with indices ranging from .08 to .84. They correlate positively with each other (Stereotypes<>Prejudice: r= .435 **, p= .000; Stereotypes<>Discrimination: r= .245 **, p= .000; Prejudice<>Discrimination: r= .481 * *, p= .000) and with ATCTRCov-19V (Stereotypes<>ATCTRCov-19V: r= .392 **, p= .000; Prejudices<>ATCTRCov-19V: r= .318 **, p=. 000; Discrimination<>ATCTRCov-19V: r= .200 *, p= .000). Then, it reveals negative and very weak interaction effects between stereotypes and ATCTRCov-19V (β= -.01) and positive effects between prejudices and ATCTRCov-19V (β= .62) and between discrimination and these attitudes (β= .14). Finally, the analysis of the Model Fit Index reveals some acceptable model fit parameters (with RMSEA= .10<.10 (or 10%); PCLOSE= .000<.5 and PRATIO= .871 close to 1). However, other parameters are not (with X 2= 965.50, Df= 183, p= .000>.5, X 2/Df= 5.275> 5; CMIN= 965.505; CMIN/DF= 5.276>5; the NFI= .548; RFI= .481; IFI= .599; TLI= .534; CFI= .594 and PCFI= .517 moving away from 1). These data partially support this model by underpinning the ability of variables underlying IC to predict ATCTRCov-19V. There are other unobservable latent variables underlying stereotypes, prejudices and discrimination that would justify the full validity of the model.
 | Figure 1. Analysis of the effects of latent variables constituting IC on ATCTRCov-19V |
4.2. Covariations between Latent Variables Underlying Intergroup Emotions and Their Interaction Effects with Attitudes towards Clinical Trials of Covid-19 Vaccines (ATCTRCov-19V)
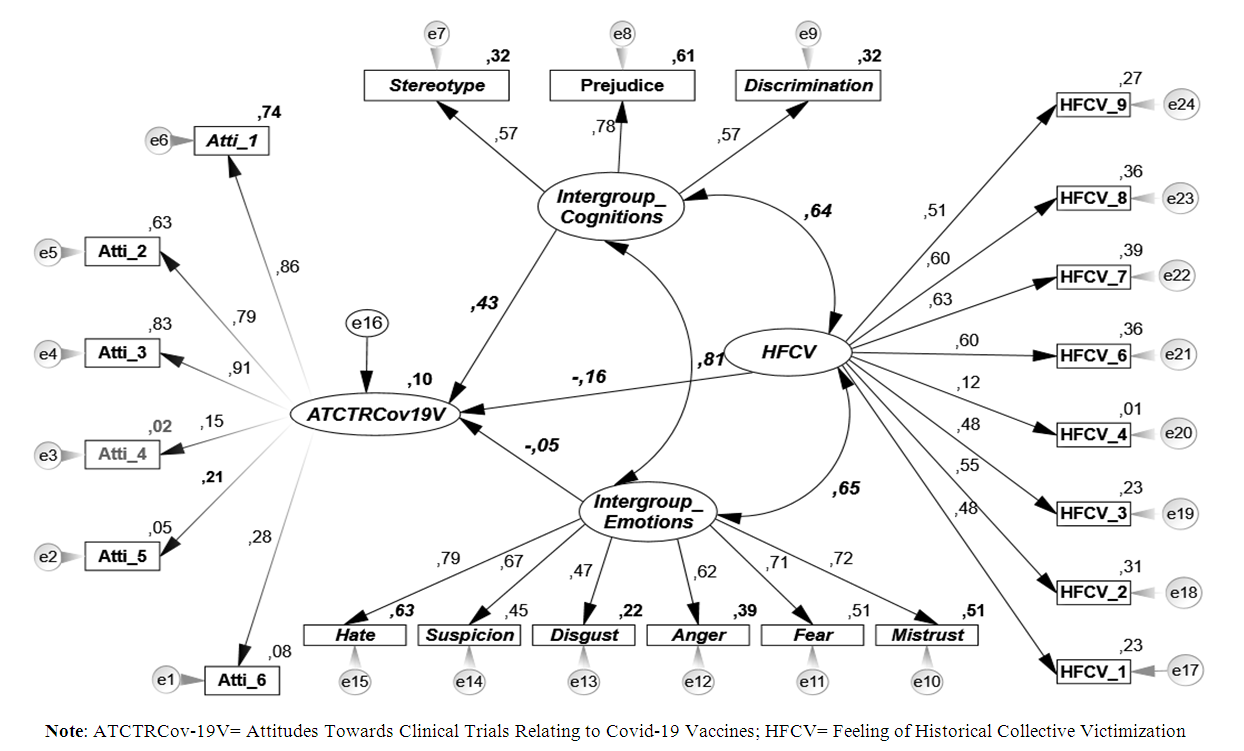
- Figure 2 first reveals that the latent variables constituting IE (Hate: M= 22.82, SD= 6.29; Suspicion: M= 20.45, SD= 5.13; Disgust: M= 16.96, SD= 5.55; Anger: M= 13.78, SD= 5.92; Fear: M= 16.43, SD= 5.25; and Mistrust: M= 34.45, SD= 7.90). These variables covariate positively and the indices range from .33 to .91. The correlation model presents positive and significant indices (Hate<>Suspicion: r= .550 **, p= .000; Hate<>Disgust: r= .410 **, p= .000; Hate<>Anger: r= .505 **, p= .000; Hate<>Fear: r= .569 **, p= .000; Hate<>Mistrust: r= .532 **, p= .000; Suspicion<>Disgust: r= 190 **, p= .000; Suspicion<> Anger: r= .316 **, p= .000; Suspicion<>Fear: r= .435 **, p= .000; Suspicion<>Mistrust , r= .505 **, p= .000; Disgust<>Anger: r= .612 **, p= .000; Disgust<>Fear: r= .420 **, p= .000; Disgust<>Mistrust: r= .225 **, p= .000; Anger<>Fear: r= .576 **, p= .000; Anger<>Mistrust: r = .369 **, p= .000; Fear<>Mistrust: r= .492 **, p= .000). These factors latent in IE are positively and significantly related to ATCTRCov19V (Hate<>ATCTRCov19V: r= .280 **, p= .000; Suspicion<>ATCTRCov19V: r= .315 **, p= .000; Disgust<>ATCTRCov19V: r= .101, p= .051> .01; Anger<>ATCTRCov19V: r= .172 **, p= .000; Fear<>ATCTRCov19V: r= .219 **, p= .000; Mistrust<>ATCTRCov19V: r= .311 **, p= .000).The model reports very weak interaction effects both positive (ATCTRCov-19VßHate, β= .00; ATCTRCov-19VßSuspicion, β= .13; ATCTRCov-19VßDisgust, β= .22; ATCTRCov-19VßFear, β= .06; ATCTRCov-19VßMistrust, β= .07) and negative between these factors and ATCTRCov-19V (ATCTRCov-19VßAnger, β= -. 25). Finally, the Model Fit Index reveals valid model fit indices (with RMSEA= .073<.10 (i.e. 7.3%<10%; PCLOSE= .000<.5) with indices such as: PRATIO= .906, IFI= .778, TLI= .752, CFI= .776, NFI= .699, RFI= .668 and PCFI= .703 close to 1, that is, they are acceptable. The indices like the CMIN= 1592.106, the ratio CMIN/DF= 2.954, the X 2= 1592.106 (Df= 539, p= .000<.05) and the ratio X 2/Df= 2.953 tending towards 5 are acceptable. These data validate the Model Fit Index and the ability of IE latent factors to predict ATCTRCov-19V.
 | Figure 2. Analysis of the effects of the latent variables constituting IE on ATCTRCov-19V |
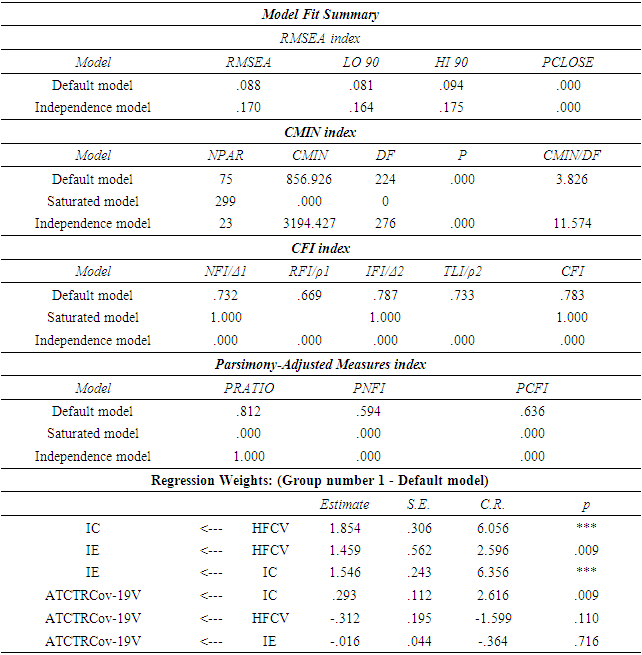
4.3. Analysis of Covariations between Predictors of ATCTRCov-19V (HFCV, IE and IC) and Their Individual Interaction Effects on ATCTRCov-19V
- In fact, the Model Fit reveals a CMIN/DF index= 3.82<5; p= .000. In view of the data collected, we note that the fit index of the hypothetical model is partially acceptable because only the p-value criterion is not respected (X 2 (1, N= 369)= 856.92; df= 224 ; ratio X 2/df= 3.825 close to 5; p= .000<.05) while the other parameters are reasonably acceptable (RMSEA= .08<.1; PCLOSE= .000<5%) (see Table 1 in appendices). This means that the hypothetical model can be accepted. Other goodness-of-fit indices obtained are acceptable. Indeed, the normalized adjustment index or delta 1 is valid and tends towards 1 (NFI or Δ1= .732). It is the same for delta 2 (IFI or Δ2= .787).The TLI or Rhô 1 coefficient (Tucker-Lewis coefficient) and the Relative Goodness Index (RFI) are valid and close to 1 (RFI or ρ1= .669; TLI or ρ2= .733; See Table 1). The comparative adjustment index is determined and also approaches 1 (CFI= .783) and the Parsimony-Adjusted Measures are approximately acceptable (PRATIO= .812; PNFI= .594; PCFI= .636; See Table 1). All of these values attest to a substantially good fit of the statistical model for predicting attitudes towards clinical trials for Covid-19 vaccines by latent variables, including HFCV, IC and IE. However, the predictive indices of the model reveal negative standardized coefficients between HFCV and attitudes (β= -.16), IE and ATCTRCov-19V (β= -.05) on the one hand; a positive standardized index between IC and attitudes (β= .43), as indicated by the above model on the other hand (See Table 1).
 | Figure 3. Individual prediction model (without moderation) of ATCTRCov-19V by HFCV, IE and IC and covariances (preliminary test) |
4.4. First level of Verification: Moderation Test of the Interaction Effect between HFCV and ATCov-19VT by IC and IE in the Multiple Linear Regression Model under SPSS 23.0
- The model in Figure 2 is based on the analysis of the single and multiple linear regression model testing the interaction effects between the variables of the study. It defines the coefficients of determination (R2) and the standardized linear regression indices (β) on the basis of which the validity of the hypothesis is based. It reveals positive coefficients underlying symmetrical interactions between the latent and explained variables. In fact, participants manifest a strong HFCV (8 items; M= 39.95> 28; SD= 8,547) and strongly negative attitudes towards clinical trials of vaccines against Covid-19 (6 items; M= 29.19> 21; SD= 7.10). The simple linear regression coefficients attest that HFCV very weakly and significantly determines ATCTRCov-19V (r= .251 **, p= .000; R2= .063; β1= .251; t= 4.96; SE= .04; CIϵ [.12 .29]; p= 000). This effect of a rate of 6.3% is all the more positive and weak as it legitimizes the use of modulating variables of this interaction by IC and IE and the statistical technique using SEM.Analysis of the effect of IE on the link between HFCV and ATCTRCov-19V first reveals that HFCV induces 20.9% of IE (29 items; M= 103.04>101.5; SD= 24.68; r= .457 **; p= .000; R2= .209; β2= .457; t= 9.86; SE= .13; CIϵ [1.05 1.58]; p= .000) which, in turn, rather generate 10.8% (>6.3%) of ATCTRCov-19V (r= .329 **; p= .000; R2= .108; β3= .329; t= 6.68; SE= .01; CIϵ [.06 .12]; p= .000). The moderation assumption tends to be reliable, as IE increases the level of the positive effect by 4.50%. Then, HFCV acts positively up to 18.1% on IC (16 items; M= 57.00>56; SD= 9.37; r= .426 **; p= .000; R2= .181; β4= .426; t= 9.02; SE= .05; CIϵ [.36 .56]; p= .000) which, in turn, induce ATCTRCov-19V at a rate of 17.2%, slightly less than 18.1% with a deviation of .9 % (r= .415 **; p= .000; R2= .172; β5= .415; t= 8.75; SE= .03; CIϵ [.24 .38]; p= .000). These simple linear regression model results show that IE and IC significantly moderate the interaction between HFCV and ATCTRCov-19V, hence the effect rates of varying interactions.Multiple regression analysis reveals insignificant effects between these latent factors (IE and IC), HFCV and ATCTRCov-19V. Indeed, the analysis of the canonical correlation between IE, IC and ATCTRCov-19V reveals a positive index (r= .433; Eigenvalue= .230; Wilks Stat.= .813). The joint effect of said latent factors reveals a positive coefficient of determination of 18.7%, predicting the explained variable (ATCTRCov-19VßIC<>IE; R2= .187; β5= .336; t= 5.96; SE= .04; CIϵ [.17 .33]; p= .000). The multiple regression proposes, for its part, indices of determinations which together indicate that HFCV, IE and IC simultaneously predict ATCTRCov-19V to the tune of approximately 18.9%. It means that when these variables are put together, their interaction effects with ATCTRCov-19V stabilize at this rate, revealing a non-significant effect of HFCV (ATCTRCov-19VßIE, R2= .18; β7=. 127; t= 2.15; CIϵ [.00 .07]; SE= .01; p= .032; ATCTRCov-19VßIC, R2= .18; β8= .322; t= 5.55; CIϵ [.15 .330 ]; SE= .04; p= .000; ATCTRCov-19VßHFCV, R2= .18; β6= .056; t= 1.02; CIϵ [-.04 .13]; SE= .04; p= .307). All these simple and multiple linear regression indices reveal the existence of the moderating effects postulated in the hypothesis of the study. However, an in-depth analysis of this moderation from a confirmatory perspective of the interaction effects between the variables as postulated in the hypothesis seems to be enriching. This justifies a second validation of the hypothesis, using statistical data from the analysis of moderations via structural equations model.
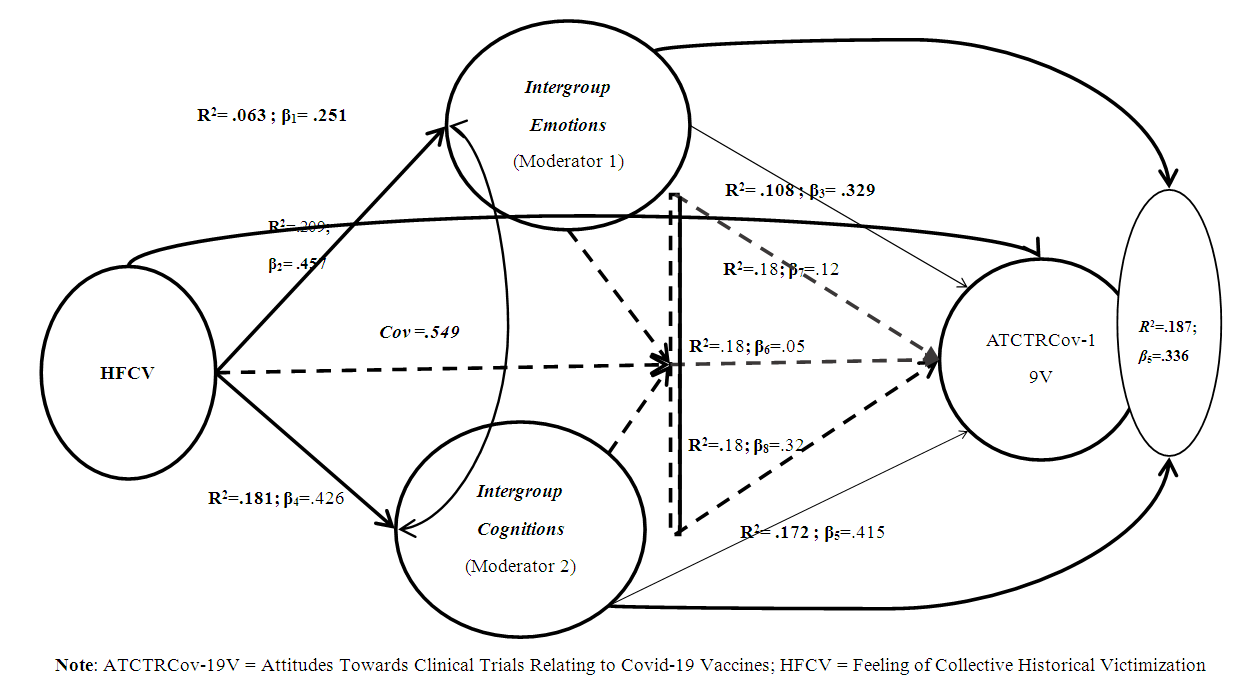 | Figure 4. Moderation of the interaction effect between HFCV and ATCTRCov-19V by IC and IE |
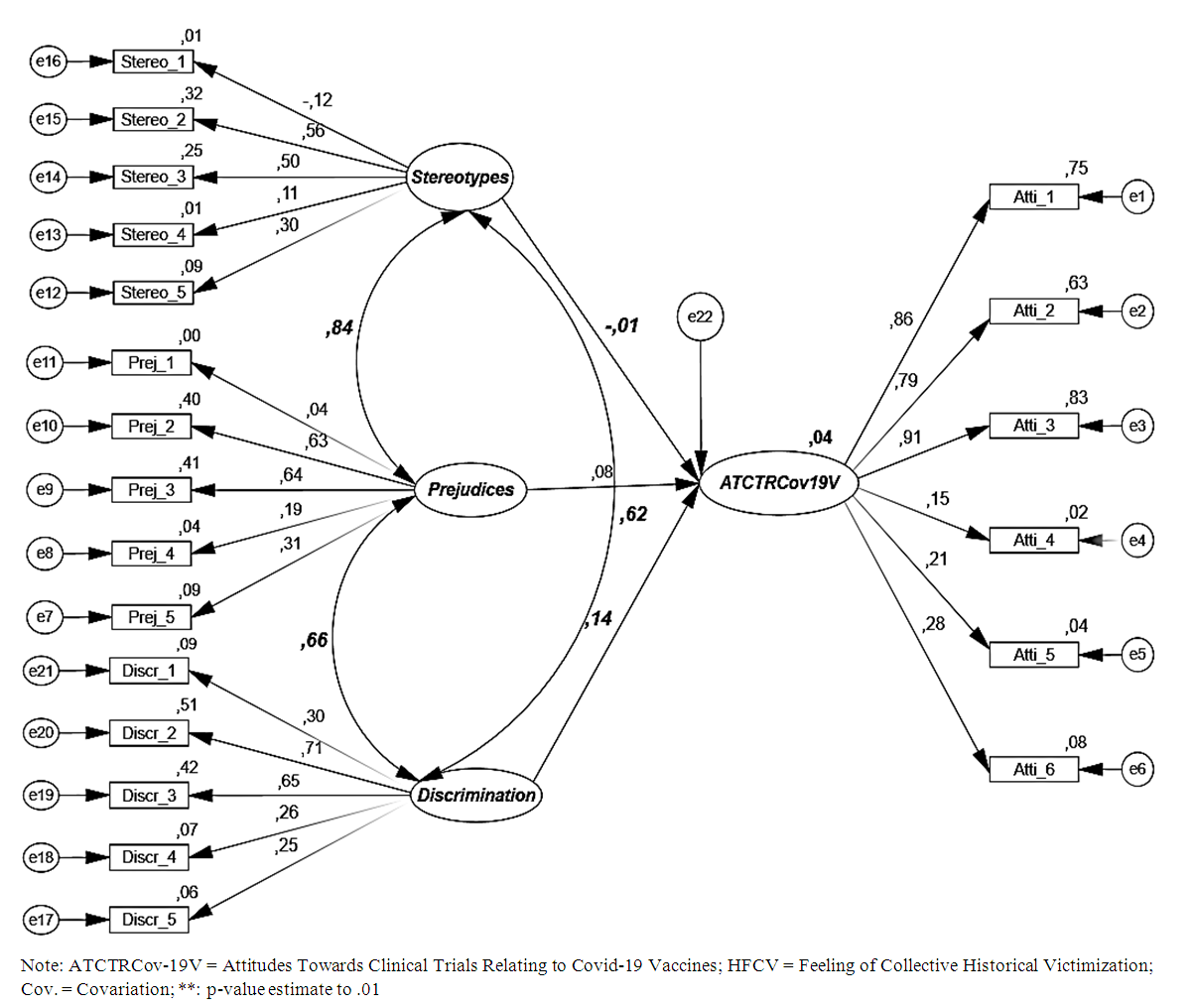
4.5. Second Level of Verification (Confirmatory): Moderation Test of the Interaction Effect between HFCV and ATCTRCov-19V by IC and IE in Structural Equation Modeling
- SEM reveal interesting results from the point of view of moderations of the link between HFCV and ATCTRCov-19V. These results differ from those analyzed in the linear regression model in Figure 2 in that they suggest negative and positive predictive indices, indicating that IE and IC moderate the relationship postulated in the hypothesis differently. This new result revealed by SEM shows that HFCV negatively predicts ATCTRCov-19V (β= -.16, ie a prediction rate of -16%). However, HFCV positively predicts IE (β= .22, i.e. a prediction rate of IE of 22%) and IC (β= .64, ie a prediction rate of IC of 64%). A positive interaction is observed between IC and IE (β= .67, or 67% interaction between these two latent factors). Following the logic of moderation, we note, however, that IC positively moderate the link between HFCV and ATCTRCov-19V (β= .43, i.e. a moderation of 43%), while IC moderates this link rather negatively (β= -.05, i.e. a negative moderation of 5%). The AMOS MLR method determined statistical parameters that attest to the good quality of the integrative model of the moderating factors of the postulated link.Table 2 (see appendices) of the Model Fit Index shows a significant CMIN/DF (CMIN/DF= 3.826<5%, p= .000). But the index X 2 is acceptable despite the p-value <5% (X 2 = 856.92; df= 224; X 2/df= 3.825 close to 5; p= .000<.05), which is not favor of an acceptable model. However, some clues may provide information on the reliability of the ATCov-19VT prediction model. Indeed, the RMSEA index is less than or equal to .1, i.e. 10% with a very good PCLOSE index (RMSEA= .088<.1, i.e. 8.8%<10% and PCLOSE= .000<.5, i.e. 0%<5%). The normalized adjustment index is valid and tends towards 1 (NFI or Δ1= .732). This is also the case for delta 2 (IFI or Δ2= .787). Likewise, the coefficients Rhô 1, Rhô 2, CFI, PRATIO, PNFI and PCFI (see Table 2 in appendices) resulting from the model of moderations of the link between HFCV and ATCTRCov-19V are similar to the coefficients resulting from the preliminary model of Figure 1 and Table 1. Beyond these reasonably acceptable additional data, it can be said that the SEM model of moderation of the interaction between HFCV and ATCTRCov-19V by IC and IE is valid. All these indices attest to a substantially good fit of the model. We conclude that IC positively and significantly moderates the link postulated in the hypothesis (ATCTRCov-19VßIC, β= .293; SE= .112; CR= 2.61; p= .009), while IC moderates negatively and not significantly this link, by reducing the strength of the negative effect between HFCV and ATCTRCov-19V (ATCTRCov-19VßIE, β= -.016; SE= .044; CR= -.364; p= .716) as noted in the model of Figure 3 (see Table 2).
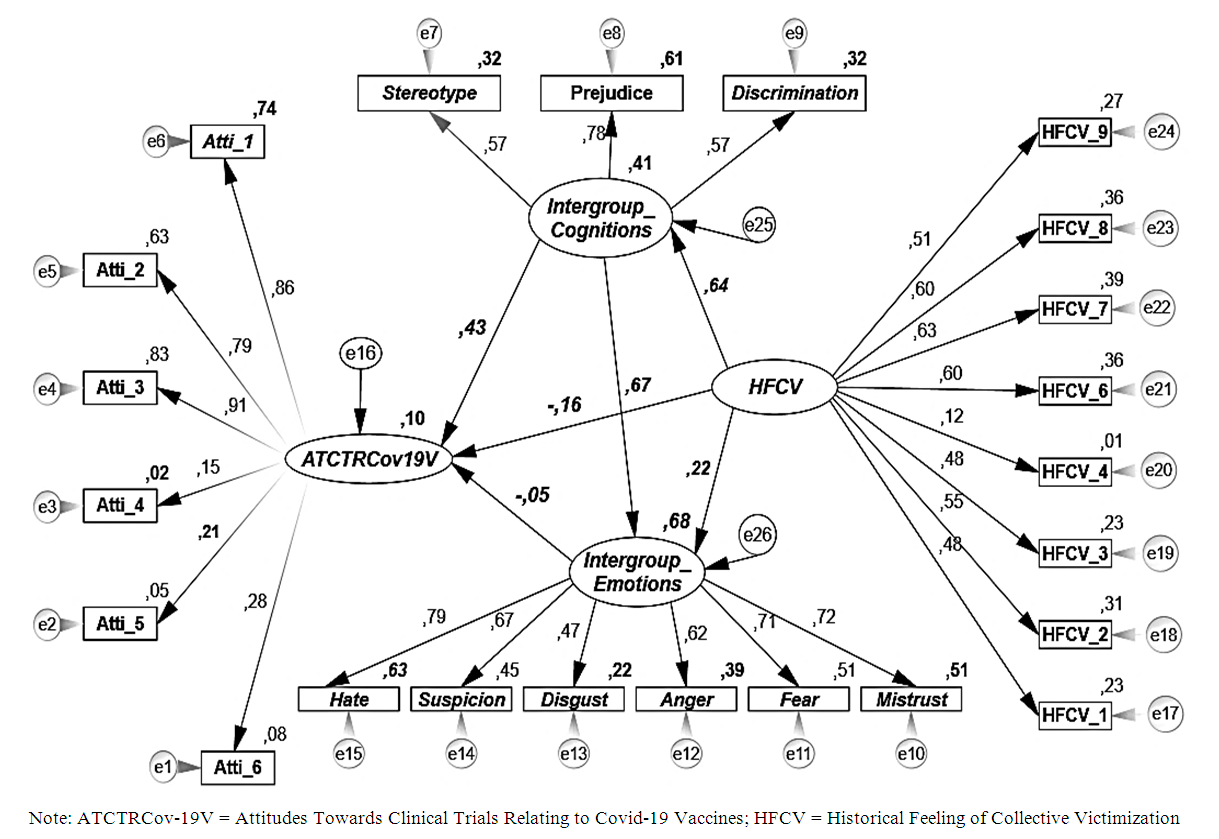 | Figure 5. SEM model of moderation of the interaction between HFCV and ATCTRCov-19V by IC and IE |
5. Discussion
- The present study tested the hypothesis that anti-Western emotions and cognitions have a moderating effect on the link between the feeling of historical collective victimization and the attitudes towards clinical trials of Covid-19 vaccines in the African context. Concretely, it was expected that: hatred, anger, fear, mistrust, disgust, suspicion, stereotypes, prejudices and discrimination generated by the feeling of historical collective victimization felt by Africans against Westerners because of the experiences of clinical trials of drugs and vaccines that have killed and severely disabled thousands of people on the continent since the colonial period, lead them to adopt a negative attitude towards clinical trials relating to vaccines against Covid-19. The data collected provides empirical support for this prediction.The observations made in this research are in agreement with the propositions of the theory of intergroup emotions (Smith, 1993), which postulates that when a social identity is salient, related situations or events produce intergroup emotions (Frijda, 2007). These emotions determine intergroup attitudes and behaviors (Mackie & Smith, 2015; Spanovic et al., 2010). They are better predictors of collective action than the perception of objects and events (Van Zomeren et al., 2008). Concretely, depending on the perception that individuals have of the situation or event, they experience specific emotions which will in turn trigger tendencies to action or particular behaviors (Frijda et al., 1989; Roseman et al., 1990). In this vein, Esses and Dovidio (2002) point out that when members of a group experience anger, it generates impulse and desire or intention to act against its source. Tausch et al. (2011) also claim that anger predicts support for normative forms of confrontation. On the other hand, hatred generates a negative assessment of outgroup members as being inherently bad and as a serious, lasting and intractable threat to ingroup (Mackie & Smith, 2015). The behavioral consequence of hatred is not a confrontation or aggression aimed at changing or correcting a situation. Rather, it is prejudice or annihilation (Fischer & Roseman, 2007; Halperin, 2008). On the other hand, those who experience fear tend to flee from its source and not to confront or attack the offending outgroup (Dumont et al., 2003). In addition, disgust towards an outgroup predicts the desire to attack it (Mackie et al., 2000). It generates more extreme and aggressive intergroup behavior in individuals, which may consist of violent attacks (Spears et al., 2009).In the specific field of health, the literature notes that negative intergroup emotions (mistrust, fear, anger towards vaccines or clinical trials) are one of the reasons for the refractory attitudes of certain populations (Africans in particular) towards clinical trials of vaccines and vaccines which are developed in the West in most cases (Cara, 2020; Desclaux et al., 2020). In this vein, Larson (2019) reports that the Ebola hemorrhagic fever vaccination campaign has been hampered by deep mistrust in eastern Congo. In communities where public health campaigns were carried out by Westerners, vaccination was viewed with suspicion and hostility. In this wake, Cara (2020) reveals that the announcement of the first tests of the Covid-19 vaccines has aroused fear, mistrust and anger among Africans. Desclaux et al. (2020), going in the same direction, note that in Cameroon, Senegal, Benin as well as in Burkina Faso, between 60 and 70% of people say that they would not accept the anti-Covid-19 vaccine if it was offered to them. These authors indicate that this reluctance can be explained by a complex assemblage of arguments and social representations which arouse doubt and suspicion. Added to this are mistrust of health workers, social spread of false information, and myths that Africans are protected against Covid-19, which generate mistrust and suspicion around clinical trials of vaccines and drugs against this disease (Samarasekera, 2021).The specialized literature reveals that in Africa, the negative emotions manifested in the area of vaccines can be explained by the past medical experiences that Westerners have carried out on the continent (Noko, 2020; Yahya, 2017). In other words, they stem from the past of victimization of Africans in the domain of health. This past is the source of a feeling of collective historical victimization; that is, a state of mind that results from one group perceiving itself as the target of harm intentionally inflicted by another group (Bar-Tal et al., 2009). This arises from an experience of considerable harm, entrenched in the collective memory of a society as serious and unfair (Paez & Liu, 2011). It generates negative intergroup behaviors that can be concretely manifested by a reduced empathy towards the suffering of outgroups, the decrease in the will to forgive them for the harm committed, the increase in their level of dehumanization and the justification of the aggression of their members (Schori-Eyal et al., 2014; Wohl & Branscombe, 2008).The results of this research also reveal that intergroup cognitions (prejudice, stereotypes and discrimination) impact on the link between the feeling of collective historical victimization and attitudes towards clinical trials of covid-19 vaccines in Africa. Indeed, the past of victimization of Africans in the health sector, the sources of which are the various fraudulent clinical trials carried out by Westerners on the African continent, generates a set of anti-Western representations which, in turn, push populations to be reluctant towards western medicine. Clearly, collective victimization manifests itself in hostile intergroup behavior (Belmonte & Rochlitz, 2019). More concretely, Aberson (2015) asserts that past experiences, positive and negative, predict the affective dimensions of prejudice, while uniquely negative experiences explain cognitive dimensions of prejudice such as stereotypes. The latter have long been associated with negative outgroup expectations (Spencer-Rodgers & McGovern, 2002). These expectations influence both information and social judgment (Ybarra et al., 1999). Because negative stereotypes generate negative expectations of the outgroup, they appear with negative emotions (Stephan & Stephan, 1996). It is in this logic that the hostile intergroup cognitions and emotions manifested by Africans in the face of Westerners are situated. Indeed, they remind Africans of the painful history of slavery, colonization, defeat, humiliation, domination and exploitation. Their memory is associated with enslavement, subjugation, exploitation, humiliation, and even mass killings. Its humiliating and disastrous character creates an emotional shock in Africans which results in negative representations that fuel the development of anti-Western cognitions and emotions (Choma et al., 2013; Jasini et al., 2017).For the literature, the history of collective victimization is likely to reinforce intergroup anxiety and perceptions of threat; thus reducing empathy towards the threatening outgroup (Techakesari et al., 2015; Visintin et al., 2016; 2017). It predicts intolerance as well as a high level of perception of threat (Skritka et al., 2006). In the specific case of this study, Westerners are seen by Africans as a source of threat. However, the perception of threat reinforces intergroup prejudices, negative stereotypes and leads to discrimination and opposition to pro-outgroup policies (Ramos-Oliveira & Pankalla, 2019; Renfro et al., 2006). Thus, the negative attitudes of Africans towards clinical trials carried out by Westerners can be explained by the fact that the latter constitute a threat to their physical and psychological well-being; hence the anger, mistrust, and even fear they arouse. This is the source of avoidance reactions and self-protective behaviors that manifest themselves, for example, in the refusal of clinical trials and vaccines.
6. Conclusions
- To limit the spread of diseases, pharmaceutical companies, most of them Western, must find drugs and vaccines. To do this, they must go through clinical trials involving humans. This is the case with Covid-19 pandemic. However, the announcement of the first trials on the BCG vaccine in Africa generated strong opposition to this project. The main basis for this opposition was the previous clinical trials of vaccines and drugs carried out on the continent, which have resulted in thousands of deaths and left profound consequences for hundreds of thousands of people. In this vein, the present research hypothesized that anti-Western emotions and cognitions (hatred, anger, fear, mistrust, disgust, suspicion, discrimination, stereotypes and prejudices) have a moderating effect on the link between the feeling of collective historical victimization and attitude towards clinical trials of vaccines relating to Covid-19 in the African context. The data collected support this prediction. They thus contribute to the understanding of the explanatory factors of the attitudes of individuals towards clinical trials of vaccines or even vaccines by revealing that to impact on the willingness of Africans to participate in clinical trials or to be vaccinated, it is necessary first to address the reluctance linked to the past of victimization to which they are subjected by the promoters of the said tests and vaccines. The reason is that the anti-Western emotions and cognitions which result from it strongly condition their health behaviors.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML