-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Applied Psychology
p-ISSN: 2168-5010 e-ISSN: 2168-5029
2016; 6(5): 156-161
doi:10.5923/j.ijap.20160605.04

An Online Educational Tool to Promote Psychological Well-being, Optimism, and Coping Self-Efficacy among People Living with an Ileostomy: A Pilot Study
Adam R. Nicholls1, Johanna Spiers1, Phil Simpson2
1Department of Sport, Health, and Exercise Science, University of Hull, Hull, United Kingdom
2York Teaching Hospital, National Health Service Foundation Trust, York, United Kingdom
Correspondence to: Adam R. Nicholls, Department of Sport, Health, and Exercise Science, University of Hull, Hull, United Kingdom.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

We assessed an online educational tool designed for people living with an ileostomy.Thirty-nine participants took part in a 10-week online educational tool, which included elements such as happiness profiling, understanding stress and coping, utilising social support, mindfulness skills, and emotional intelligence training. Participants completed questionnaires to assess the effects of the online educational tool on well-being, optimism, and coping self-efficacy at Time 1 (baseline), Time 2 (after the intervention), and Time 3 (three months after completing the online educational tool). Psychological well-being, optimism, use of problem-focused coping self-efficacy, and stop unpleasant emotions and thoughts coping self-efficacy were significantly higher, with large effect sizes, at both Time 2 and Time 3, than Time 1.The online educational tool appears to be a promising time and cost effective method of promoting positive outcomes, although additional testing is required before it could be used in conjunction with existing healthcare treatment.
Keywords: Inflammatory Bowel Disease, Multi-disciplinary teams, Nursing, Positive Psychology, Stoma
Cite this paper: Adam R. Nicholls, Johanna Spiers, Phil Simpson, An Online Educational Tool to Promote Psychological Well-being, Optimism, and Coping Self-Efficacy among People Living with an Ileostomy: A Pilot Study, International Journal of Applied Psychology, Vol. 6 No. 5, 2016, pp. 156-161. doi: 10.5923/j.ijap.20160605.04.
Article Outline
1. Introduction
- Ileostomies are used to treat a variety of conditions such as bowel cancer or inflammatory bowel disease (e.g., ulcerative colitis or Crohn’s disease). Recent figures revealed that over 1.3 million people across the world have an ostomy, which includes ileostomies, colostomies, and urostomies [1]. A review by Ang [2] suggested that stomas can negatively affect an individual’s physical, psychological, social, and sexual health, which can be stressful for some individuals. Ang [2] called for interventions to help people with ileostomies manage such difficulties. The scarcity of interventions is surprising as people with an ileostomy are more likely to have decreased well-being than the general population. Decreased well-being is associated with poorer life quality [3]. Many people living with an ileostomy struggle to come to terms with their stoma, which may result in body image difficulties and recalling their ileostomy surgery as a stressful memory [4, 5]. Issues with body image and stressful memories of surgery may impact the well-being of people with an ileostomy [3]. Well-being includes affective and psychological functioning, and consists of two specific perspectives: the hedonic perspective (i.e., happiness and life satisfaction) and eudiamonic perspective (i.e., psychological functioning and self-realization) [6]. Well-being represents positive mental health, with the terms well-being and positive mental health often used interchangeably [7]. Well-being and positive mental health are associated with people fulfilling their abilities, coping with stresses in life, and working productively or fruitfully [8]. As such, improving well-being among people living with an ileostomy may enhance life quality.Ileostomies may also have the potential to impact negatively on optimism. Scheier and Carver (1985) defined optimism as “a major determinant of the disjunction between two classes of behavior: (a) continued striving versus (b) giving up and turning away” (p. 227) [9]. Indeed, optimism influences how people appraise and cope with stressful events [10]. Three studies featuring people living with an ileostomy revealed that higher levels of optimism predicted reduced psychological distress and superior life quality [11, 12] and served as protective mechanism against negative moods [13], so enhancing optimism levels appears especially important for people living with an ileostomy.Given the potentially stressful nature of stomas [2, 14], coping also remains an important mechanism to help those living with an ileostomy to alleviate stress. Coping refers to cognitive and behavioral efforts to manage internal or external demands that are appraised as exceeding the resources of a person [15]. In a study that included people living with ileostomy, Hoffman [16] reported that problem-focused coping strategies (e.g., positive reframing and meaning making) were beneficial. Scholars, however, are yet to explore the underlying mechanisms that may underpin coping among people with ileostomy, such as an individual’s confidence in his or her ability to cope effectively with stress. This is known as coping self-efficacy (CSE) [17]. Scholars, however, are yet to explore the underlying mechanisms that may underpin coping among people living with ileostomy, such as an individual’s confidence in his or her ability to cope effectively with stress. Although CSE remains untested among people living with an ileostomy, higher CSE is associated with reduced stress among other people living with other disfiguring conditions, such as traumatic burns [18]. Living with an ileostomy can be very stressful for some individual [2, 11, 14], with individuals that have had this experienced this surgery often experiencing decreased well-being [3], and optimism [11]. It is therefore surprising that there is a lack of psychological educational programs to enhance the quality of life among individuals with an ileostomy. As such, we piloted an Online Educational Tool (OET), designed to enhance psychological well-being, optimism, and coping self-efficacy. If successful, such a resource could be a useful tool for stoma care and non-specialist nurses to encourage and enhance psychological care in people living with a stoma, without being a significant time or cost burden. Indeed, there is a shortage of specialist Stoma Nurses in countries such as the United Kingdom and the United States [19]. As such, these specialist nurses may have little time to provide the level of psychological care required. It is therefore unsurprising that people living with an ileostomy are in need of more psychological support than they currently receive [20]. As such, a time and cost effective psychological intervention that nurses can help patients access, could be a useful tool. Further testing is required, using an RCT design, before the OET could be used in healthcare settings. We hypothesised that well-being, optimism, and the different components of coping-self efficacy would increase from T1 (baseline) to T2 (after the intervention), and would be sustained at T3 (three months after completing the intervention).
2. Method
2.1. Participants
- Fifty-eight participants took part in this study, but 13 participants dropped out during the OET and six participants failed to complete the final assessment (Time 3). The final sample contained 39 participants (female n = 29, male n = 9, transgender female n = 1; M age = 51.33 years, SD = 13.53). Participants were Caucasian (n = 35), Afro-Caribbean (n = 1), Mixed Race (n = 1), Hispanic (n = 1), or did not report their ethnicity (n = 1).
2.2. The Online Educational Tool
- The OET consisted of 10 sessions, across 10 weeks (see Table 1 for the themes, content of activities, and purpose). On average, sessions lasted around 45 minutes. All outcome variables were assessed across three time points for each participant at Time 1 (pre-intervention), Time 2 (immediately after completing the OET), and Time 3 (three months after the OET finished).
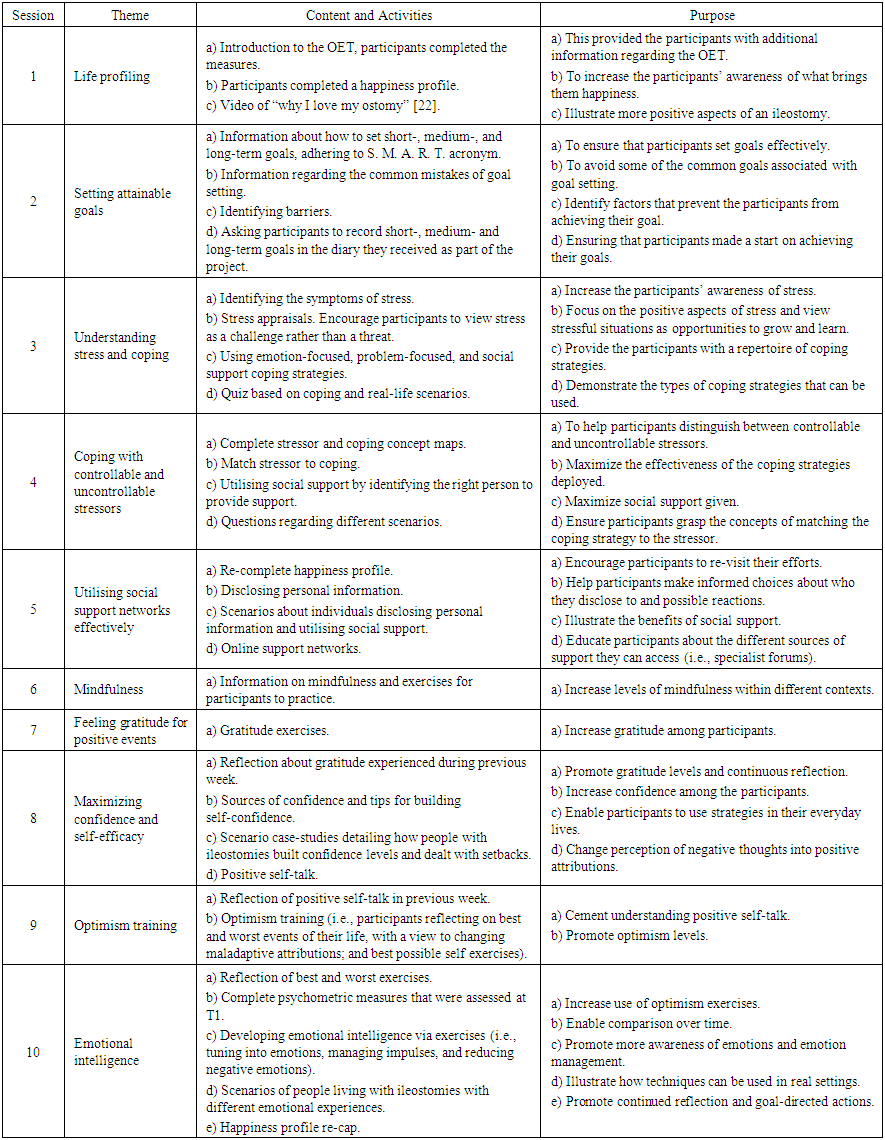 | Table 1. Session Theme, Content and Activities, and Purpose |
2.3. Outcome Variables
- Psychological Well-being. The 7-item, Short Warwick Edinburgh Mental Well-Being Scale (SWEMWBS) [7] assessed psychological well-being. Participants responded to the stem: “Below are some statements about feelings and thoughts. Please circle the number that best describes your experience of each over the last couple of weeks.” Participants answered questions such as “I’ve been able to make up my own mind about things” and “I’ve been feeling optimistic about the future.” All questions were answered on a 5-point Likert-type scale ranging from 1 = none of the time to 5 = all of the time. Tennant [7] reported Cronbach's alphas of .89 for students and .91 for their general population sample.Optimism. The Life Orientation Test-Revised (LOT-R) [22] assessed optimism. The LOT-R contains 10-items, which includes four filler questions Participants responded to the stem “Answer according to your own feelings, rather than how you think "most people" would answer.” Questions (e.g. “In uncertain times, I usually expect the best” and “Overall, I expect more good things to happen to me than bad”) are answered on a 5-point Likert-type scale, anchored at 0 = strongly disagree and 5 = strongly agree. Scheier [22] reported a Cronbach alpha of .78 for the LOT-R.CSE. The Coping Self-Efficacy Scale (CSES) [17] examined CSE. The CSES is a 26-item questionnaire that measures three higher-order dimensions of CSE: use problem-focused coping, stop unpleasant emotions and thoughts, and get support from family and friends. Participants respond to the stem “when things aren’t going well for you, or when you’re having problems, how confident or certain are you that you can do the following.” All questions are answered on an 11-item scale, anchored at 0 = cannot do at all, 5 = moderately can do, and 10 = certain can do. Questions captured the participants’ ability to “find solutions to your most difficult problems,” “stop yourself being upset by unpleasant thoughts,” and “get a friend to help you with the things you need.” The CSES [17] demonstrated adequate reliability, with a Cronbach’s alpha of .95.
2.4. Procedure
- After receiving ethical approval from a University ethics committee, we recruited participants from a range of online sources (e.g., stoma support forums, IBD peer support forums, and Facebook groups) by placing an advert that provided some information about the study. The inclusion criteria was that participants were aged 18 years or over, and had a permanent or temporary ileostomy. Participants that expressed an interest in taking part in the study were sent an information that provided more information about the study, such as the length of the OET, content of the OET, and information at the questionnaires the participants would be asked to complete. Participants also received a consent form, which they were ask to sign and return by post. Once we received the signed consent form, participants were sent a link to OET via their e-mail address. Following this, participants received a new electronic link each week for the new topic. If participants failed to complete a weekly session, they were sent a reminder e-mail. If participants had any questions regarding the weekly topics or activities within any of the sessions they could contact a research assistant by e-mail or telephone.
2.5. Data Analysis
- We conducted five one-way repeated ANOVAs. The dependent variables were the total scores on the SWEMWBS [7], the LOT-R [22], and the three subscales of the CSES [17]. Time of measurement represented the independent variable. We employed an alpha level of .05 and partial eta squared (η2p) indicated the effect size for each construct. Finally, we performed a Bonferroni adjustment on the p value to guard against Type I error rates as a consequence of multiple comparisons.
3. Results
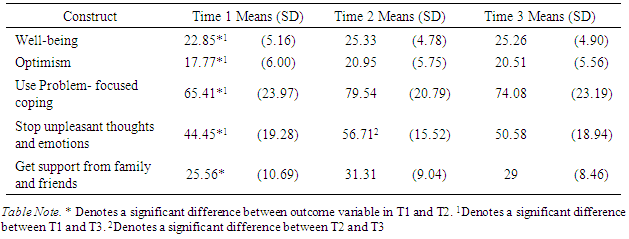
- The means and standard deviations for each outcome measure across the three time points are presented in Table 2. There were significant effects for time in well-being (Wilks Lambda = .78, F [2, 37] = 5.208, p < 0.01, η2p = .220), optimism (Wilks Lambda = .548, F [2, 37] = 15.252, p < 0.0005, η2p = .452), use of problem-focused coping (Wilks Lambda = .608, F [2, 37] = 11.938, p < 0.01, η2p = .392), stop unpleasant emotions and thoughts (Wilks Lambda = .507, F [2, 37] = 17.47, p < 0.0005, multivariate partial eta squared = .493), and get social support from family and friends (Wilks Lambda = .664, F [2, 37] = 9.341, p < 0.01, η2p = .336). Post-hoc analyses revealed that well-being and optimism were significantly higher at both T2 and T3 than T1. Use problem-focused coping and stop unpleasant emotions and thoughts scores were significantly higher at both T2 and T3 than T1. Although get support from family and friends was significantly higher at T2 than T1, the difference between T1 and T3 was not significant.
|
4. Discussion
- The overall purpose of this pilot study was to develop, run, and assess the effects of the OET among people living with an ileostomy. Surprisingly, resources to enhance psychological well-being or reduce stress among people living with an ileostomy are scarce, despite the benefits of such an intervention for this population. Our results suggest that the OET was successful in enhancing psychological well-being, optimism, and coping self-efficacy, which may be sustained over time. We quantitatively examined the effects of our OET, which was designed to enhance psychological well-being, optimism, and components of coping self-efficacy. Overall, we found support for our hypotheses because there were significant increases, with large effect sizes, in well-being, optimism, use problem-focused coping, and stop unpleasant emotions and thoughts from T1 to T2, which were sustained three months later at Time 3. There was also a significant increase in get social support from family and friends from T1 to T2, but this significant change was not sustained until T3. People living with an ileostomy are more likely to report reduced psychological well-being as a consequence of their ileostomy surgery [3]. Enhancing well-being, and therefore positive mental health, may improve the day-to-day lives of those living with an ileostomy. The OET helped enhance well-being among the participants from the start of the intervention to the end of the intervention, and these results were mostly sustained three months later.Optimism is a psychological construct with some similar outcomes to well-being, in terms of its association with reduced psychological stress and superior life quality [11]. The apparent success of our OET in enhancing levels from T1 to T2, which were sustained at T3, illustrates how this construct can be enhanced among people living with ileostomy and how improvements in the construct appear relatively stable for at least three months. The OET appeared successful in improving all aspects of coping self-efficacy from the start to the end of the intervention. Unlike psychological well-being and optimism, however, not all of the changes lasted until the final testing point three months later. The OET was successful in enhancing the participants’ belief in their ability to use problem-focused coping and thus solve any problems that might arise from the start of the study to three months later. In terms of stop unpleasant emotions and thoughts coping self-efficacy, there was a significant increase from baseline to the end of the intervention and three months later. There was, however, a significant decline in the scores in this scale from the end of the intervention to three months later. Furthermore, although the OET was successful in enhancing managing support from family and friends coping self-efficacy from T1 to T2, there were no significant differences from T1 to T3. Similar to the results with self-efficacy in managing unpleasant thoughts and emotions, the reasons for this finding are unknown. It could be that the element of the intervention which taught the participants how to use social support was less effective. Alternatively, it may be that people need regular encouragement in accessing social support from family or friends. A limitation of this study is that it did not contain a control group. The promising findings of this study could be built upon by an RCT, which would include a control group. Another limitation of this study is that we experienced the high attrition rate, which is typical of online based interventions [23]. In order to limit attrition, we encouraged participants to go back to earlier exercises, offered a prize draw for completion of all 10 weekly sessions, and included encouraging messages about how many weeks were left within the OET itself. Finally, it would be interesting to monitor the effects of the OET after 12 months, rather than the three month period in the present study. A unique feature of this OET is the fact that there was no face-to-face contact and all participants completed the different parts of the program on their computer. Our program could be adapted in the future so it could be completed on tablet or mobile phone devices whilst patients are in hospital. Online programs appear a cost and time effective way of delivering psychological training, and that they could be used independently or alongside healthcare treatment. Before this could occur, out OET needs to be tested via a randomized control (RCT) design. A limitation of this study is that there was no control group due to participant recruitment problems. The promising findings of this study could be built upon by an RCT design with a control group included.
5. Conclusions
- Online programs appear a cost and time effective way of delivering psychological training to people living with an ileostomy. Such training programs could potentially be used independently or alongside the healthcare treatment provided by specialist Stoma Nurses. Future research, however, is required to test the effectiveness of the online educational tool we developed within hospital settings and when the patient first receives his or her ileostomy. This may help reduce the burden on stoma nurses, as they may need to spend less time dealing with the psychological implications of the stoma surgery, which are addressed in the OET. Given these initial findings, refinements could be made to the OET, which could then be tested using an RCT design.
ACKNOWLEDGEMENTS
- We are grateful to all of the participants that took part in this study and the Ileostomy Association, who funded this project (grant number: AD13/res).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML