-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Applied Psychology
p-ISSN: 2168-5010 e-ISSN: 2168-5029
2016; 6(4): 121-129
doi:10.5923/j.ijap.20160604.06

A Pilot Evaluation of a Multidimensional Treatment Model (MTM) of 8 to 12 Year Old Students with Mild Attention Deficit and Hyperactivity Disorder
Aliakbar Torabi
Department of Health, IRAN’s Ministry of Education, Iran
Correspondence to: Aliakbar Torabi, Department of Health, IRAN’s Ministry of Education, Iran.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Purpose: This study aimed to identify the Multidimensional Treatment Model (MTM), for students with ADHD 8 -12 years as an approximately inclusive and stable treatment. Methods: In this study 100 students. The students ranged in age from 8-12 years students; these were placed in two groups. Fifty students as control group and fifty students experimental group were included. Study measures pretest exam taken from Vanderbilt Assessment Scale. It was given to their parents and teachers included (NICHQ, 2002). The experimental group with their parents and their teachers were enrolled by (MTM) for 4 months while control group were not enrolled. The post measures were taken from the VAS. Results: Pre-test and post-test database interpretation, showed significant improvement in the group of students who were in the MTM group. Conclusion: In this study in addition to the current methods of treatment for children with ADHD, other Treatment techniques such as brief hypnosis, mental imagery, and mind games (chess) because of having a more stable and more persistent treatment may be of assistance.
Keywords: Multidimensional Treatment Model (MTM), Students with Attention Deficit and Hyperactivity Disorder (ADHD)
Cite this paper: Aliakbar Torabi, A Pilot Evaluation of a Multidimensional Treatment Model (MTM) of 8 to 12 Year Old Students with Mild Attention Deficit and Hyperactivity Disorder, International Journal of Applied Psychology, Vol. 6 No. 4, 2016, pp. 121-129. doi: 10.5923/j.ijap.20160604.06.
Article Outline
1. Introduction
- At present, there are two well-established evidence-based treatment strategies for childhood ADHD: medication and behavior therapy. As such, one may ask, why is anything else needed? Current evidence-based interventions, however, providing symptomatic relief too many patients, have several significant limitations, making them far from a panacea [1]. Attention deficit and hyperactivity disorder (ADHD) is the most common disorder of school children in the absence of proper identification and intervention can lead to irreversible complications. It is a prevalent developmental disorder that can seriously impair a child’s cognitive, emotional, social and academic performance as well as their family life across multiple contexts such as school and home [2]. ADHD as a chronic disorder even reduces self – concept of students because self- concept of children with chronic illnesses undoubtedly influences their attitudes and perceptions [3]. The goal of treatment for children with ADHD is to decrease the symptoms, improve adaptive functioning and enhance the well-being of the children and their family through comprehensive assessments and intervention program [4]. A multimodal treatment can be the most effective treatment of ADHD [5]. The multimodal approach normally includes pharmacological treatments, psychological treatment (i.e. cognitive behavior therapy, family therapy), and psycho-education. Pharmacological intervention is the treatment of choice in children and adolescents with severe ADHD [6]. Multimodal approach to medication selection in the treatment of children and adolescents with ADHD. This study [5] found that this therapeutic approach produced positive effects on behavior management of children and adolescents with ADHD also positive parenting parents as a psychological treatment and control student behavior in the classroom by the teacher contributed to the success of this method [7]. Behavioral interventions are also recommended as a therapeutic approach. There were significant improvements in: parenting quality for positive parenting standardized mean difference (SMD) 0.68, for negative parenting (0.57), parenting self-concept (0.37), and child ADHD (0.35), conduct problems (0.26), social skills (0.47), and academic performance (0.28) [8]. Nero-feedback and standard pharmacological intervention in ADHD, in a study showed that behavioral rating scales that were completed by fathers, mothers, and teachers at pre-, post-treatment, two-, and six-month naturalistic in both groups, similar significant reductions were reported in ADHD functional impairment by parents; and in primary ADHD symptoms by parents and teachers [9]. Collaboration between Pediatric nurse practitioners and School Nurses: Meeting the complex medical and academic needs of the Child with ADHD has studied. This study showed that Optimizing partnerships with school nurses will provide better surveillance of treatment efficacy and can facilitate improved health and academic and social outcomes for children with ADHD [10]. A Parent-Teen Collaborative Treatment Model for Academically impaired high school students with ADHD showed that parent-teen collaboration is a promising standard behavioral treatment model for ADHD high school students [11]. Results of studying the effectiveness of playing chess as a treatment option for suggest a large effecting decreasing the severity of ADHD [12]. Several studies have documented the benefits of physical activity for children with ADHD at physiological skills and behavioral levels [13]. Physical activity as a treatment for ADHD children in a research has studied; this study suggested considerable potential for enhanced physical activity, in particular regular moderately intensive aerobic exercise, to be beneficial to the core inattentive and hyperactive/impulsive symptoms of ADHD [1]. But evidence suggests various therapeutic approaches such as pharmacological, psychological, social and physical treatment that sometimes reported many great success stories isn’t singly efficient for students with ADHD and their family’s concerns don’t will be removed. For example unfortunately, many parents are reticent to putting their child on just pharmacological treatment that may provoke side effects, such as insomnia, appetite suppression, or growth retardation [15]. Thus providing a relatively stable and comprehensive model is necessary to able to improve educational performance and psychosocial accommodation for such students.
2. Methods
- This study was an experimental research for students with ADHD from Tehran’s primary schools.
2.1. Identify of the (MTM)
- The Multidimensional Treatment Model (MTM), has tried common applied therapy approaches in addition, it has benefited from other treatment techniques such as mental imagery, and mind games (chess), (even brief hypnosis). This treatment model has combined and expanded from difference dimensions to make sure no aspect should be overlooked. The dimensions of the MTM in this study include: 1-Behavioral Therapy and Behavioral Cognitive Therapy (BT & CBT), 2- Family therapy (positive parenting training), 3- training and applying of school and teacher collaboration, 4- Nero feedback, 5- brief hypnosis and mental imaging 6-mind games (chess), 7-structural physical activity and sports, 8- pharmacological treatment (in selection). Generally all of the dimensions and clinical parameters are based on clinical works for treatment of students with ADHD 8-12ages.
2.2. Sample and Design
- In this study number 100 teacher nominated students from difference Tehran primary schools who their inclusion criteria were as follows: (1) age of 8–12 years, (2) diagnosis ADHD by DSM-V (3) normal intelligence based on either a WISC-R full scale IQ score above 80 or the average/above documented with the last year’s final school grades (50 persons as control group and 50 persons for experimental group). At first 150 students were sequentially included. Reasons for not entering into the study were either because they had at least another mental disorder e.g. Bipolar Depression (DSM-IV) or parents lived too far away to drive their children on a weekly basis or because the children did not enjoy clinical program (n = 50). The Mean age (SD) was 10.73 years (±2.24). The majority (92%) of participants had ADHD, combined type, and 65% were taking medication for ADHD.
2.3. Instruments
- The research instrument was Vanderbilt Assessment Scale (VAS) [14], performing this instrument for all of the participated parents and teachers both groups that including 47 questions for parents and 35 questions for teachers. In addition it consisted of two parts (Academic Performance and Classroom Behavioral Performance) in academic performance items; reading, mathematics and written expression and in Behavioral Performance items; relationships with peers, following directions/rules, disrupting, assignment completion, and organizational skills were discussed. It was standardized on 30 parents (mothers & fathers) and 32 teachers previously. Teachers form validity coefficient was 0.68 and reliability coefficient was 0.69 and parents form validity coefficient was 0.71 and reliability coefficient was 0.70.
2.4. Intervention Model Performance
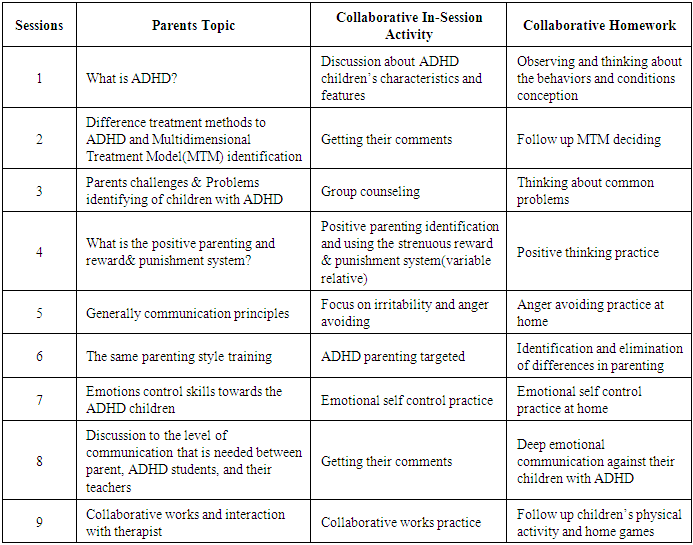
- The experimental group with their parents and their teacher took part in the (MTM) for 4 months: Step A: Making a therapeutic team involving: BT & CBT, hypnotherapy, parenting training, physical activity, chess specialists and a social worker. Step B: Lunching the trainable meeting for parents and collaborated schools teachers for overall justification. Step C: pretest Exam performance by Vanderbilt Assessment Scale (VAS) [14], for all of participated parents and teachers both groups. Step D: starting the clinical works for experimental group including students, their parents and related teachers (D1): 1 hour weekly BT & CBT by applying appropriate reward and punishment system and special control behaviors forms with parents and teachers collaboration. Filling the special forms is a procedural triangular collaboration of students, parents and teachers. In this special forms many factors for behaviors control: pre or post structural physical activity, writing, dictation, math and other students times at the classroom and doing homework, communication at parties or social situations times, have planned which should be based on the therapist's instructions and recommendations to be completed by the students, parents and teachers. Additionally, performance graphs were shown when it was convenient. (D2): 3 sessions weekly brief hypnotism and mental imaging for remembering daily behaviors and activities at classroom, home and other situations were employed. (D3): 3-6 sessions weekly chess playing (digital or human base) at the clinic and home under parents management. (D4): generally 9 sessions weekly positive parents training and communication against their children with ADHD, Table 1. (D5): 1 session teacher retraining about ADHD student’s communication and emotional control skill among such students. (D6): 3 sessions Nero- feedback was presented to the students as a computer game (puzzles, races, Pac-man, etc.) in which they had to concentrate to win. Specifically, students were instructed by the trainer to develop and prolong the strategy that best helped them to win points in the game. The students received visual and auditory reinforcement contingent on their success in controlling microvolt of theta or beta. (D7): physical activity and exercise weekly involving 3 -6 times of swimming and playing in the water at a safety poll, and other aerobic activity 45-60 minutes per session recommended. (D8): pharmacological treatment: Medication prescribed with parental consent by psychiatrist’s administration although after reduction of symptoms frequency, gradually dosage reduced it removed for some cases during the study. (D9): weekly following-up the comments of parents and teachers and reporting to the researcher by social worker by getting the specially forms. (D10): generally 16 sessions among 4 months (1session per a week), clinical works were down. In sum, a session had a length of 35 min approximately. Each 1 session 5 runs included. There were short pauses between runs that enabled them to relax so that the clinical times of mental imaging increased 10-25 SEC per each session, Table 2. (D11): management and registration of intervention model’s progress through interaction with colleagues and drawing reportable diagrams, by researcher. Step E: posttest's conducting for both groups. Step F: Collecting and preparing data for statistical projects.
|
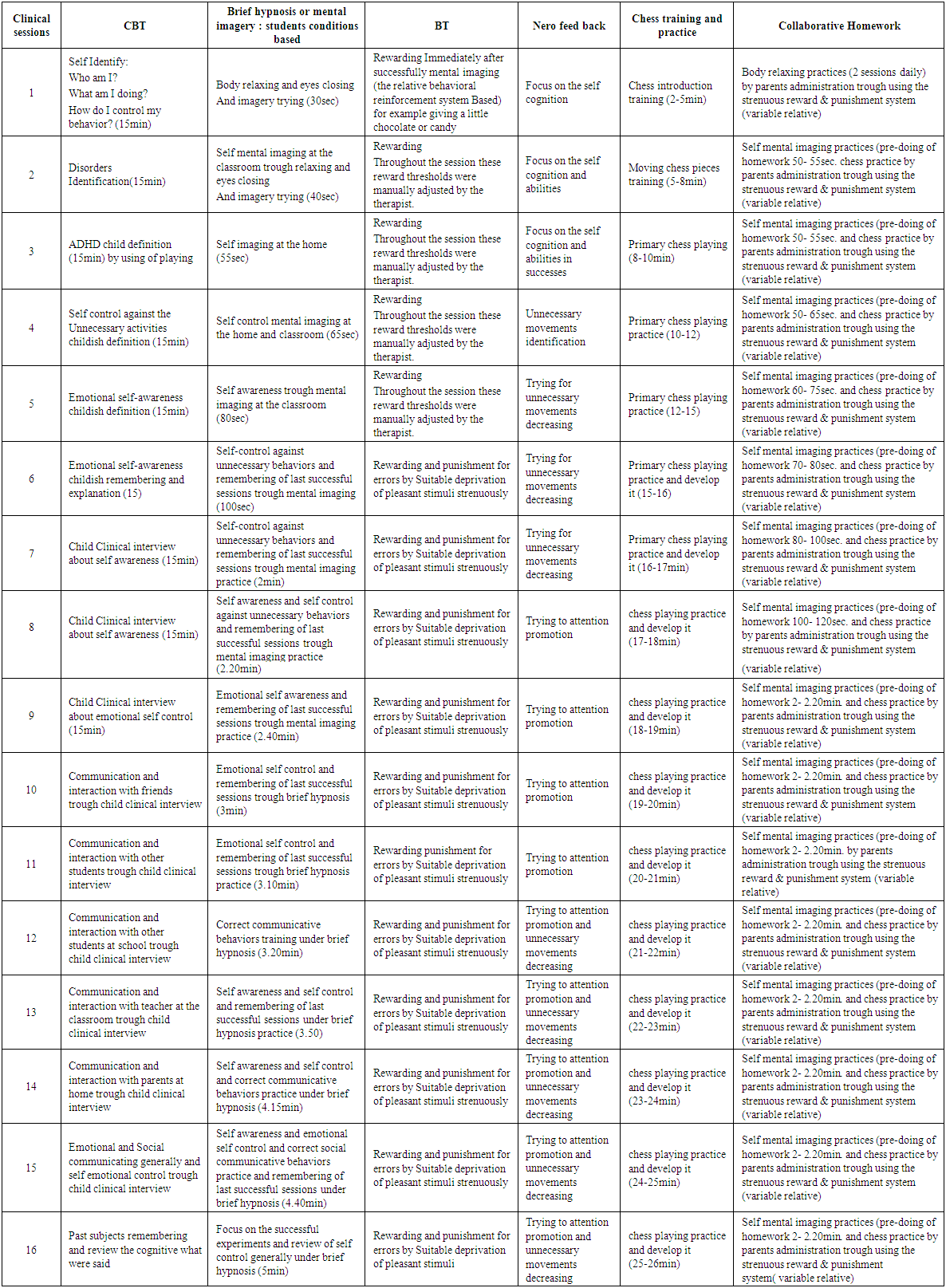 | Table 2. Clinical Works and Collaborative Homework |
2.5. Statistical Projects
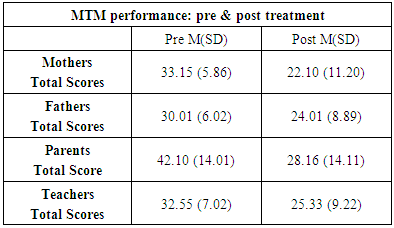
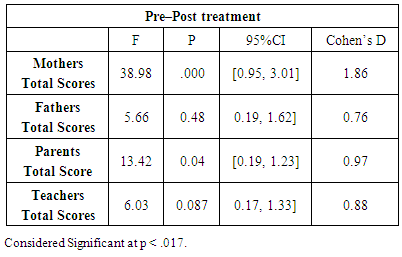
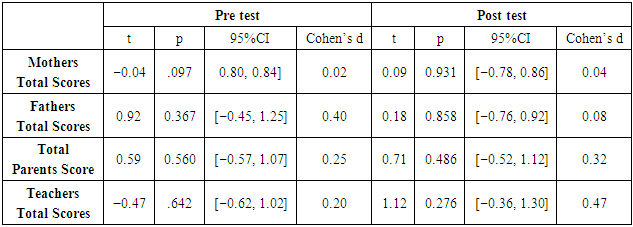
- The collected data were analyzed by using inferential e.g. ANOVA for the model’s effectiveness on decreasing disorder severity among of the students with ADHD and t-tests to determine the significant difference between pretest and posttest (in SPSS). Within subject change scores were calculated from the difference in pre- to post-test scores and the cutoff point for considering statistical significance was set at p < .05. In addition means and standard deviations (SD) were calculated for the variables considered in the study. Table 3
|
3. Results
3.1. Feasibility
- Finally one hundred persons completed the study, indicating an elevated adherence rate. Two children dropped out after two MTM sessions. As might be expected, no adverse events were reported in any students. On average, students attended the 14 sessions (87.50%). students reported an average of nearly two hours per week of mind playing and chess practice at home and six hours per week physical activity (swimming) at a pool(home collaborated activities). Medical treatment was continued for all of participant who received medication formerly also for all of the students with parents satisfaction.
3.2. Pre- and Post-treatment Assessment
- Eighty five percent of the 100 (85%) parents and 70 of 82 (85.36%) teachers in the post treatment’s Mean and SD versus the pre treatment assessment reported a reduction in the Vanderbilt Assessment Scale (VAS) [14]. Following the convention used in MTM trials, a clinically significant decrease in ADHD severity was observed as a reduction of 38% or more in (VAS) score. Thus, 88% parents and 78.57% teachers reported at least a 41% ADHD severity reduction in the (VAS). There were statistically significant pre- to post-intervention improvements in ADHD severity as measured by (VAS). These analyses separating by student’s gender were repeated. In males (n = 65), significantly improved (19.54 ± 5.47 vs 14.92 ± 5.91, p < .05, respectively). In females (n = 45), however, the (VAS) improved after MTM (37.42 ± 9.53 vs 30 ± 8.1, p< .05. In order to test the magnitude of the difference between pre- and post-intervention’s effect sizes (VAS) calculated. The improvement in ADHD severity scores from base-line did not vary by age, commitment (MTM), and hours of collaborative activity practice at home. The effect sizes for MTM performance assessment, was considered trough (VAS) questionnaires exposition by ANOVA. Table 4
|
|
4. Discussion
- Nevertheless, our sample was limited, making it unfeasible to conclude that MTM and medication are equivalent treatments for ADHD. Concerning posttest assessments, overall participants receiving MTM, achieved improvements two months and even six months after completing. Concerning the effect of treatment performance at post test better at the pre test was observed. Overall, taking in consideration large and medium effects sizes throughout the different behavioral evaluations, MTM effects are comparable. Data suggested those mothers and teachers more bevioral improvements than fathers consequently, a more pronounced improvement in ADHD could be expected. Therefore, margin for pre-post improvement was lower for the participants. Thus, the items of MTM are effective to ADHD. A larger improvement for inattention in comparison to hyperactivity/impulsivity according to parents was also consistent with previous studies [16, 17]. Other studies could examine what is needed for MTM effects retention in over longer periods of time. For example Nero-feedback has found that behavioral improvements were maintained after 4 months [18, 19], and even after 2 years after completing the training [20]. This study also indicated that 83% of parents were satisfied with the MTM, so they were not satisfied to pharmacological treatment alone. The application of MTM that it should be emphasizes. The importance of implementing principles of MTM items have been recently indicated [21-23]. Thus, factors of MTM animations playing, in Nero-feedback instructions given to participants, and reward thresholds may play a crucial role [24]. This study’s findings support the some studies concerning MTM items such as Nero-feedback training [21-23], Chess training [12], positive parenting and family therapy [11], physical activity [1] teachers and school collaboration [11] and also a small range of options [23]. Our findings support this procedure, and suggest that MTM efficacy would be compromised when it is not implemented, as reported by other authors [25, 23].Another limitation that: MTM did not include transfer training to reach generalization of regulatory skills to daily life activities. Presumably, a better outcome could have been achieved if these strategies would have been incorporated during training. At the same time, this design was a good indirect way to measure the degree of satisfaction for MTM. The importance of this study relies on being the first randomized-controlled trial that compares pre & post test of MTM parent and teacher reports, including two assessments at pre and post treatment. These assessments have been useful to demonstrate that the majority of children treated with MTM are able to maintain many of their progress and even continue improving. These particularly positive results for MTM suggest that actively training the brain may produce certain lasting beneficial effects in contrast to pharmacological intervention. Furthermore, another important aspect of our study has been the use of multiple evaluators (mothers, fathers, and teachers) and the inclusion of a measure of academic performance.This study showed statistically significant clinical improvements in both inattentive and hyperactive symptoms from pre- to post when MTM was employed A significant majority of parents reported some improvement in ADHD severity in their children, and nearly half of the parents reported a 41% decrease in ADHD severity. In addition, effect size estimates in the present study were large, similar to the effect sizes of MTM reported for treating ADHD in students received benefits from MTM.A decrease in the P score versus the baseline for parent-rated scales after MTM was found. Both inattention and hyperactivity symptoms improved according to the pre-and post-treatment results. However, many previous studies has shown that CBT & BT, positive relation parents, chess and physical activity can help improve social and cognitive skills in children with ADHD [15]. A recent study suggests the beneficial effects of chess playing compared to other extracurricular activities in children. This study reported that those playing chess were more likely to improve their cognitive abilities, problem-solving capacity, and coping in contrast to the sports group [26]. The results have shown that MTM can provide a product of an improvement of executive functions in ADHD students. Executive functions include some cognitive processes core to ADHD. Executive functions are involved when behavioral, cognitive practice, brief hypnosis and mind imagery and playing chess, i.e. the ability to think ahead, acting memory, self imaging at the classroom situation and at home, analyze the effectiveness of interaction with parents and teachers, plan chess moves before they are made and impulsivity control in Nero- feedback. Another reason that helps to explain why MTM is beneficial to ADHD students is that these students benefit from variable relative reinforcements, immediate feed-back, interesting brief hypnosis, mind imagery and relaxation and structural physical activity. Clinical improvement was found in both genders. This is important because many studies have recently reported that the female gender is a marker of a worse prognosis in students diagnosed with hyperactivity disorder it means that hyperactivity is frequently a ‘‘hidden disorder’’ in girls. Even though more boys than girls are diagnosed with ADHD [27] both genders equally respond to psycho-stimulant treatment [28]. As suggested here, girls can also benefit from MTM. Additionally the pharmacological treatment is a selective treatment in students with ADHD by their parents [6]. But it seems that, medication is necessary to decrease the level of ADHD symptoms for students to benefit from MTM, at least initially. In other words, MTM appear to have a complete role to psychotherapy within the multidimensional treatment schema for students with ADHD. A correlation between IQ and ADHD improvement after the MTM was found. Furthermore, in a recent study, the authors reported strong evidence for their hypothesis that adults with high IQ who meet DSM-IV criteria for ADHD are more likely to report more impairment in executive functions than the general population [29]. Therefore; MTM could be a very interesting therapeutic complement to high IQ students with ADHD. This study may be the first study to benefit of mind imaging and brief hypnosis that can improve ADHD symptoms. To many other things employed, one of the strength points is that the pre and post-intervention design allows for the comparison of ADHD severity. Even using the 45% ADHD improvement criteria [30], a significant percentage of teachers and parents reported that the ADHD severity decreased in scale. This is important considering that reductions between 35% and 45% in the severity of symptoms are considered clinically meaningful [31, 32]. More-over, we used effect sizes to measure the magnitude of the association between MTM and the improvement in ADHD symptoms. This allowed us to which enables to measure this type of relationships more effectively than values, regardless of statistical significance. [33] However, effect sizes ‘‘satisfy statistical, not clinical, needs’’ [34]. Indeed, even if results are promising, we should bear in mind that the level of post-intervention ADHD symptoms displayed by most of students was still notable. These results must also be interpreted in light of several limitations inherent to naturalistic, descriptive studies [35]. First, the outcome measures were teachers and parent-reported scale. Out-come may bias their responses [36], [37]. However, all teachers and parents were unknown to their previous assessments, and some have suggested that the expectation of treatment benefit does not contribute to changes in treatment response in ADHD students [38]. Thus randomized and controlled studies were limited [38]. In addition, the resources are very limited in media; the descriptive intervention design was the most feasible at this point in time. In conclusion, more methodologically sound studies (i.e. including independent observations; randomized, controlled trial design studies) with larger samples are warranted.
5. Conclusions
- In this study other treatment techniques such as brief hypnosis, mental imagery, and mind games (chess) were applied in addition to the current methods for children with ADHD, because more stability and more persistent treatment. This study indicated that MTM might play an important role in the treatment for students with ADHD. High IQ students appear to be more particularly benefited. If results are replicated in more studies, MTM could be included as treatment with more confidence of ADHD. Thus, ‘‘MTM’’ could be potentially used as a high cost resource for improving ADHD students in the public school system.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML