-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2020; 10(2): 29-35
doi:10.5923/j.health.20201002.01
Received: Dec. 3, 2020; Accepted: Dec. 20, 2020; Published: Dec. 26, 2020

ACL Reconstruction along with Outcomes in Early and Late Presentation
Alamgir Adil Samdany1, Md. Rahimullah Miah2, Shankar Kumar Roy3, Abdul Gani Ahsan4, Baqi Billah3
1Department of Orthopaedics, North East Medical College Hospital, Sylhet, Bangladesh
2Department of Information Technology in Health, Northeast Medical Pvt Limited, Sylhet, Bangladesh
3Department of Orthopaedics, Sylhet Osmani Medical College, Sylhet, Bangladesh
4Department of Orthopaedics, Sylhet Women’s Medical College, Sylhet, Bangladesh
Correspondence to: Alamgir Adil Samdany, Department of Orthopaedics, North East Medical College Hospital, Sylhet, Bangladesh.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: The anterior cruciate ligament (ACL) is an important structure for maintaining stability of the knee joint, particularly in activities involving weaving, pivoting or kicking, which is the normal biomechanics of the knee. It is the most commonly injured knee ligament. The purpose of this study is to find out the commonest cause of ACL injury and the age group involved in our community. Whether the time gap between injury and treatment has any impact in the prognosis after ACL reconstruction. The knee becomes unstable with a ruptured ACL and the joint may become more damaged over time. ACL reconstruction is the surgical treatment of choice. Methods: This was a prospective observational study conducted at the department of orthopaedics in North East Medical College Hospital over a period of 8 years. About 200 admitted patients had ACL reconstruction done during this time. Data were collected in respect to patient’s profile, diagnosis and ACL rupture records. All patients were stratified by primary and secondary tears, age, sex, side of injury, activity level and graft type of reconstruction. Results: The study showed that about 67% of male and 33% female patients had ACL reconstruction and rehabilitation. The study also represented that ACL rupture patients were more in 2013 but it is reduced in 2018 due to increase individual’s awareness. From 2012 to 2019, the 200 individual ACL reconstructions were done by two specialist surgeons. The age group was between 16 to 51 yrs. Most of the injuries were sports related. Many of them were household injuries. Only few accounted for accidental injuries. Conclusion: The incidence of ACL tears in orthopaedics patients increased over the last 8 years. Females were at higher risk except in the 17 to 18-year-old group. Peak incidence is noted during high school years. Allografts continued to be associated with a greater risk of secondary ACL injuries. Nonoperative treatment carried more risk of contralateral tears than ACLR. These data help target the most at-risk patients for ACL prevention programs.
Keywords: Anterior Cruciate Ligament (ACL), Graft tear, Incidence, Secondary
Cite this paper: Alamgir Adil Samdany, Md. Rahimullah Miah, Shankar Kumar Roy, Abdul Gani Ahsan, Baqi Billah, ACL Reconstruction along with Outcomes in Early and Late Presentation, Journal of Health Science, Vol. 10 No. 2, 2020, pp. 29-35. doi: 10.5923/j.health.20201002.01.
Article Outline
1. Introduction
- At present anterior cruciate ligament (ACL) is among the most commonly performed procedures in knee surgery, which tears are understood to transpire with growing regularity in early patients [1]. Previously it reflects the efforts to start a feasible, dependably positive reconstruction techniques, but in the 20th century we all witness a collective cognizance of interest in the ligament and its lesions. A number of 200 ACL rupture was recorded in our study period within 2012 to 2019, while more than 150000 new ACL ruptures annually in USA [42]. Types of injury were variable. Diagnosis, treatment and recovery was affected by various factors [2,3,10,5,6,7]. Patients presented early had better outcome than late group. ACL is important for maintaining stability of the knee joint [59], particularly in activities involving weaving, pivoting and kicking [8,9,10,11]. The knee becomes unstable with a ruptured ACL [12] and the joint may become more damaged over time [13,14,15,16]. ACL reconstruction is the surgical treatment of choice [17,18,19,20]. General principle of ACL reconstruction restores functional anatomy of a knee joint [21,22,23]. The therapeutic response after ACL rupture is deprived of patients and without surgical reconstruction, the ACL lacking knee is inadequate [41]. For this reason, these are the patient’s happenings and such ACL deficiency can lead to future progressive changes [43,44,45,46].The aim of this study is to evaluate the cause of ACL rupture [24] with outcomes in early and late presentation in injured patients at the department of Orthopaedics at North east Medical college Hospital.
2. Methodology
- The prospective observational study conducted at the department of Orthopaedics in North East Medical College Hospital (NEMCH) in Sylhet, Bangladesh over a period of 8 years from 2012 to 2019. Sample size was 200 in number both male and female patients. Data collectionPrimary data collected from the NEMCH pertaining on anterior cruciate ligament (ACL) injury causing rupture with primary tears and secondary tears including accidental, sports, households and others from the existing ward. Meanwhile secondary data were collected from diverse sources government hospitals, private health centres, clinics, NEMCH central library, journals, daily news, books and relevant websites.Informal DiscussionInformal discussion is integrated with the patient’s guardian like father, mother or relative at NEMCH. Other data were collected through informal counselling with them to observe patient’s complication or major problems. This informal discussion was also used to be aware with them to recover from ACL rupture.Inclusion criteriaAge group patients between 16 to 51 years with students, players, households, businessman and other profession. Some of them require non-operative treatment, who have no or minimal anterior tibial subluxation and no additional intra-articular injury. Those who have the marked anterior tibial subluxation and additional intra-articular damage.Exclusion criteriaPatients were included the occurrences of ACL rupture diagnosis [25,26,27]. Total 200 patients were selected recorded careful history through physical examinations and their diagnoses were performed. Among 200 patients, males were 133 and 67 of female’s patients.Data CompilationAll general information regarding ACL rupture’s history, clinical examination, investigation, diagnosis, management and follow up data were compiled according research objective.Data Analysis and InterpretationCompiled data were integrated for analysis and interpretation findings through standard data analysis software like SPSS version 26, MS Excel 2019 and R programming version 3.6.
3. Results
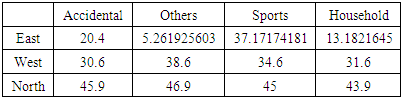
- During the study period, 200 patients were included at the department of Orthopaedics in North East Medical College Hospital. ACL presentation were recorded in respect to history, clinical examination, ACL tears between male and female with different years. The study shows that 67% male and 33% female were treated as ACL reconstruction rehabilitation from 2012 to 2019, which as shown in Figure 1. In 2013 maximum patients were 35 males but minimal 3 female patients in 2019.
 | Figure 1. ACL reconstruction rehabilitation among male and female |
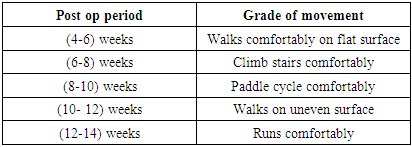
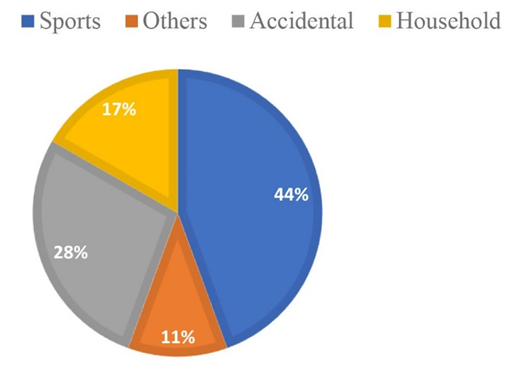 | Figure 2. Types of injury causing ACL rupture |
|
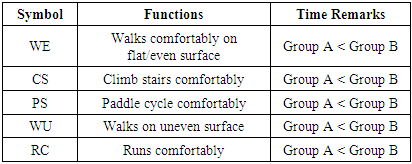
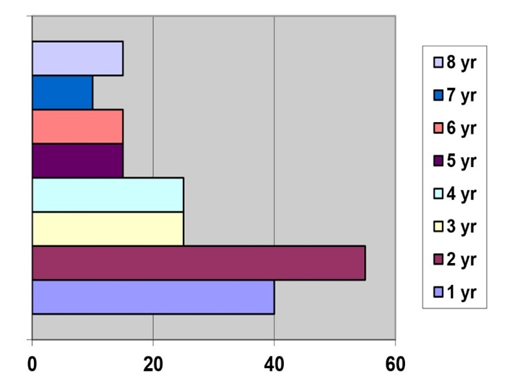 | Figure 3. Number of patients diagnosed in time |
|
|
|
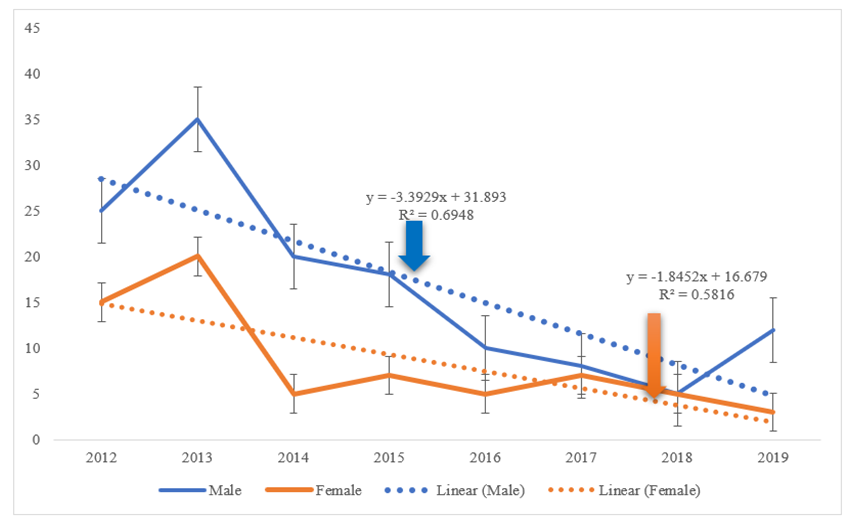
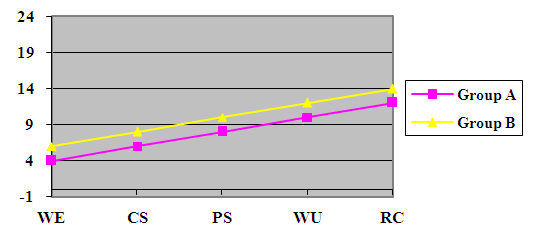 | Figure 4. Time difference in recovery for both groups |
4. Discussion
- ACL rupture is one of the commonest sports injuries in this region. Usually occurs in young age group. So far presentation to a specialist is delayed [28,29]. This delayed presentation causes further structural damage to the knee [30,31,32,33,58]. Outcome was quicker and expected in patients who presented early [34]. ACL reconstruction is an excellent operation in terms of alleviating symptoms and getting patients back to their functional state [35,36]. Early diagnosis, early treatment is less destructive to the knee [37]. The primary outcomes of an ACL tear should be contingent upon in making the diagnosis [59,60]. Through analysis of NEMCH data on a captured population of patients, we were able to calculate true incidence numbers for a large metropolitan population of orthopaedics patients. We also found that the percentage of ACL injuries surgically reconstructed increased, and the average time from injury to surgery increased significantly over our study period [38]. In earlier, the importance of ACL reconstruction technique was documented by Fick [48]. Modifications of this technique have been described by a number of authors [52,53,54,55,56,57]. This study is the first of its kind to identify an increase in the incidence of ACL tears in young patients over the last 8 years. These data are novel in that they report incidence of ACL injury within a known, closed cohort. Data were obtained on a yearly basis, so the admitted indoor database allows for correction of patients entering and leaving the operative and non-operation plans [39]. These measures should add to a more complete understanding of what we have suspected in terms of increases in orthopaedics ACL injury over time. Ligament purpose and instruments of rupture was determined by Cadaver studies, who encouraged repair for the acute injury and conventional treatment for chronic ruptures [49]. Enduring follow-up evaluations do not validate the hope that anatomic repositioning of the residual ligament would result healing. The study advised to evade the later development of a painful, disturbed joint with recurrent effusions, following arthritis fluctuations and the attendant enduring infirmity [51]. Research into ACL reconstruction area remains, while many medical practitioners now practice variations of this technique. Research and innovation prosper in this field with advances in clinical outcomes being accomplished continuously. Knowledge of the evolution of ACL reconstruction is helpful to those who continue to try to progress the outcomes of the technique in order to additional the changes previously completed, but also to lessen the risk of reiterating the faults of the historical.
5. Challenges
- The study has some challenges due to misusing of cutting-edge technology in developing countries including expertise and application. The data were collected from a specific regional private medical institution in Sylhet. Therefore, the injury and surgical treatment rates may reflect regional differences and thus may not be representative of other areas of Bangladesh and in other countries. The people covered under this presentation plan also probably represent people of a certain socioeconomic class. Patients with a different quality of age may have more or less exposure to at-risk activities and higher barriers to access of care, which may affect the overall incidence rate [37,40]. The presentation database itself has limitations. We attempted to identify repeat injuries in patients who have a new diagnosis code after 4 months, and this assumption fails to include new injuries that occur in the first 4 months after return to sport [21]. For patients with multiple injuries, we were unable to distinguish between primary tear of the contralateral knee and a recurrent tear of the originally injured knee. In addition, patients with ACL injuries could have been missed by entering or leaving the health insurance plan before getting the health codes required for inclusion, so the incidence may actually be higher than that which is reported here. Despite these limitations [37], this is the first study quantifying and showing an increase in the incidence of ACL tears in young aged sport players [50].
6. Conclusions
- This study is the first to show that the incidence of ACL tears in orthopaedics patients has significantly steadily increased in stipulated time. Both male and female adolescents have a peak incidence during high school years. ACL reconstruction is an excellent operation in terms of alleviating symptoms and getting patients back to their functional state. Early diagnosis, early treatment is less destructive to the knee. The presented ACL reconstruction is a main area of research wide-reaching [41]. Future studies identifying the mechanism of injury in young patients will be helpful for proposing prevention training.
Disclosure
- Data AvailabilityThe data are being used to support the findings of this research work are available from the corresponding author upon request. Competing InterestsThe authors declare no potential conflict of interests in this research work.
ACKNOWLEDGEMENTS
- The authors acknowledged the authority of Northeast Medical College, affiliated with Sylhet Medical University, Sylhet, Bangladesh for kind support.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML