-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2018; 8(2): 19-25
doi:10.5923/j.health.20180802.01

Continence Home Care: A Qualitative Study of Family Carers and Community-based Continence Care Providers
D. Wayne Taylor1, Jacqueline J. Cahill2
1The Cameron Institute, Canada
2The Canadian Continence Foundation, Canada
Correspondence to: D. Wayne Taylor, The Cameron Institute, Canada.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Incontinence is an embarrassing and debilitating condition that has become a major, growing health concern for men and women of all ages worldwide. Fecal incontinence (FI) remains the understudied of the incontinence twins. This exploratory, qualitative, home-based care study was conducted in southern Ontario, Canada to identify the knowledge, confidence, skills and perceptions of personal support workers and family carers. There is a need for on-going education and training of both paid and volunteer FI care-givers; a long overdue de-stigmatization of FI and the proper listing of it as a disability that impairs livelihood and quality-of-life; and public-private-notforprofit collaboration to optimize the care provided elders living at home with FI.
Keywords: Bowel, Continence, Fecal, Home care, Incontinence
Cite this paper: D. Wayne Taylor, Jacqueline J. Cahill, Continence Home Care: A Qualitative Study of Family Carers and Community-based Continence Care Providers, Journal of Health Science, Vol. 8 No. 2, 2018, pp. 19-25. doi: 10.5923/j.health.20180802.01.
Article Outline
1. Introduction
- Incontinence is an embarrassing and debilitating condition that has become a major, growing health concern for men and women of all ages worldwide. Incontinence is the lack of voluntary control over urination or defecation or both. Many urinary and fecal incontinent patients do not have access to or knowledge of evidence-based medical therapy and their quality of life suffers because of the stigma inherent. Qualitative studies and epidemiological data have repeatedly shown that patients do not understand the actual meaning of the word “incontinence”, whether this is urinary or fecal, thus both conditions have been often under-reported [1-5]. In particular, several years may pass beyond onset before incontinent women will present their symptoms to a physician or other health care provider and/or be referred to a specialist [1, 6-8]. FI is often suffered in silence without seeking health care [9, 10].Fecal incontinence remains the understudied of the incontinence twins – fecal (FI) and urinary (UI) - in terms of academic and clinical research reports, interest and understanding; and despite progress on the FI front, the gap is growing. In previous work by the authors in 2013 a rudimentary search of the electronic academic search engine, Google Scholar, identified 337,000 articles written about UI compared to only 74,000 that studied FI [9]. In 2018 the same type of search revealed 538,000 papers on UI versus 131,000 for FI [11]. This represents an unmet need in both attention and care of FI given that the prevalence rate for UI has been estimated at 28% in the non-institutionalized population overall [12]; the prevalence of FI at 18% [13]; and the prevalence of double incontinence (DI) - FI presenting concurrent with UI - at 55% [14]. The epidemiology and the socio-economic consequences of UI have been well-defined in the incontinence literature whereas the community prevalence and adverse impact of FI remain less understood. The main reason is the use of different interview questions in highly selected and hospital-based populations that has resulted in widely varying reported prevalence rates and impacts [15]. In Canada, the prevalence rate of FI ranged from 2% in a community-based sample of middle-age subjects and 3% in the nulligravid secondary school female teenage population, to 8% in post-partum women following obstetrical anal sphincter injury, and 46% amongst the elderly in long-term hospitals [15-18]. There is little reliable research data with respect to the perception, knowledge, and health-care seeking behavior of Canadians with FI let alone the confidence and competence of care-givers whether professional or family. Many incontinent patients in Canada are treated by their family physician. These general practitioners have reported that they are not adequately trained to provide proper care for incontinent patients and they seldom treat or refer to a specialist right away [19]. Recent research showed that professional care-givers in long-term facilities (nursing homes) also were not confident in their skills to care for FI residents [9].Like many post-industrial societies, Canada has an aging population with an ever-increasing burden of chronic diseases and disorders that puts great strain on limited community care capacity. This paper looks at the care of incontinence in the community against this backdrop. One answer to the capacity issue has been to delegate many care protocols to unregulated, lesser trained health care adjutants (such as personal support workers in the Canadian province of Ontario) or family members of the incontinent. Unit costs in this home-care scenario of care are 5% of the cost for equivalent care in an institutional setting [20]. Economic strategists would say, home care or community care, due to its perceived cost-effectiveness and geographical dispersal of point-of-care, is “stuck in the middle” – starved for resources needed to be effective with no real economies of scale for efficiencies [21].The objectives of this study were to determine of personal support workers (PSWs) and family carers their:a. general continence knowledgeb. fecal incontinence knowledgec. fecal incontinence perceptionsd. confidence when dealing with people with fecal incontinencee. skill level when dealing with people with fecal incontinencef. in-class education for dealing with fecal incontinence (PSWs only). andg. on-the-job training for dealing with people with fecal incontinence (PSWs only).
2. Methods
- Almost all staffing for continence care in the home in Ontario is by personal support workers (PSWs – 1 year community college; non-clinical supportive care only) who are supervised by registered practical nurses (RPNs – 2.5 year community college; limited scope of nursing practice) or registered nurses (RNs – 4 year university baccalaureate degree; full nursing scope of practice). Given the limited and decreasing number of hours of public home care available in Ontario, and the growing demand for same, much home care, especially continence care, is provided by family members either living with the incontinent individual or travelling from their home to provide care in the subject individual’s home [22]. This study did not investigate the role of private-pay care.This home-based care study was conducted in southern Ontario, Canada. No previous similar research of this kind was found. For that reason, an exploratory, qualitative study was designed and conducted using a structured interview protocol of 83 questions (36 close-ended on a 10-point Likert-type scale; 39 on a binary, yes-no scale; 2 open-ended; 6 demographic). Questions were derived from the Self-Learning Package – Continence Care Education by the Registered Nurses’ Association of Ontario (2006). Some were re-worded so that clinical language could be better understood by family members interviewed [23]. Social desirability bias and “yes-saying” bias, both potentially high in face-to-face interviews, was controlled for by the utilization of a well-trained and experienced interviewer very familiar with the subject matter and the samples being interviewed [24].A community care agency was approached and provided researchers with access to 12 personal support workers (9 day shift, 3 evening shift) and 10 family member carers for a sample of 22. A sample of family physicians was also invited to participate but withdrew due to the lack of financial compensation for them.Hard copies of the questionnaire were shared with respondents. Responses were recorded on an electronic tablet with the respondents’ permission, verbatim. Data were entered into an Excel spreadsheet; frequencies and means calculated for each setting and the sample as a whole and for each category of carer. Data were analyzed to identify care-giver gaps in knowledge, confidence, education, training and skills in caring for incontinent patients generally and FI patients specifically. No statistical analysis involving significance values was conducted as the sample size was not deemed adequate. Sample size was average, however, for qualitative research of this nature where no similar studies exist in the literature. Sample size was also adequate for saturation [25] which was observed amongst the raw data [23].Participants in the study were presented with informed consent documents which identified the title of the project, the names of the researchers and their affiliations, the project’s objectives, and assured them that their data would be kept anonymous, confidential and in a safe place. Ethics approval was obtained from a registered medical ethicist and the Research Ethics Board of the Peterborough Health Center. It was deemed to be a quality improvement project meeting the requirements of the Tri Council Policy Statement as they apply to informed consent.
3. Results
- All, but two, of the PSW staff interviewed were female with an average age of 52 years, ranging from 32 to 68. The family members were evenly split between male and female with an average age of 70 years, ranging from 62 to 82 years of age. All PSWs had a community college (post-secondary, non-degree) education whereas only half of the family members had any post-secondary education. The average length of practice amongst the PSWs was 12 years with a range of <1-28 years. The average length of experience with incontinent patients for the PSWs was 11 years which is typical of the industry where employers seldom start new employees with incontinent cases. The average family member had 4 years of experience dealing with someone who was incontinent.Generally, staff was long-serving, middle-aged permanent employees qualified for their positions. Patients were in their later years of life as were their family carers. Although incontinence can strike at any age regardless of gender, the preponderance of FI and DI is found within the older half of a population pyramid [26]. In an aging population such as Canada’s this is a growing challenge of significance as can be seen in Figure 1.
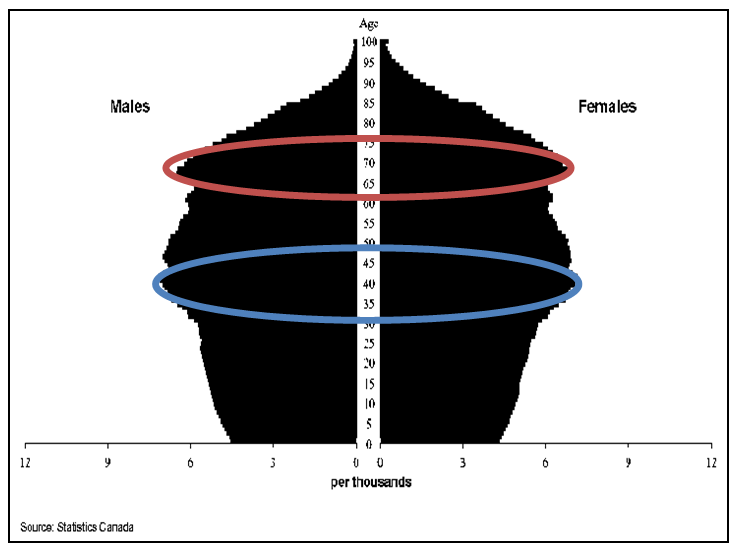 | Figure 1. Canada’s ageing population pyramid (or, muffin) 2031 projection |
3.1. General Continence Knowledge
- When it came to general continence knowledge respondents collectively did not fare well. Of the 22 binary questions in this section only 1/3rd of the questions had more than 75% of the respondents knowing the answer. Five questions were evenly split between yes and no answers. These included the physiological reasons for incontinence, factors contributing to incontinence, the value of using a voiding diary in the assessment and management of incontinence, patients’ perceptions of their incontinence, and how to teach others about scheduled voiding. In effect this showed that both PSWs and family carers caring for someone in the home were just as apt to be minimally coping with the patient’s incontinence as actually helping the patient to mange his/her incontinence. Another four of these questions were answered overwhelmingly negative. Neither PSWs nor family members seemed to understand the components of a comprehensive assessment in the management of incontinence, the components of a functional assessment, the use of a 3-day voiding diary in developing an individualized prompting protocol, or how to teach others about incontinence. Again this provided evidence that caregivers in the home knew incontinence when they saw it and what to do in the immediate, but did not know how to manage incontinence as a chronic condition.These results were not surprising for family members but disappointing for PSWs as these scores were much worse than those recorded for PSWs in residential long-term care facilities as reported elsewhere [27].
3.2. Knowledge of Fecal Incontinence
- Ironically, the driving question behind this research, to investigate health professionals’ and family carers’ knowledge of fecal incontinence, was rewarded with respondents generally having a better understanding of FI than incontinence in general; the difference between acute diarrhea and chronic FI; the relationships between laxatives and FI, between medications and FI, between diet and FI, and how to properly clean someone with FI. Respondents lacked knowledge about the causes of FI, the proper care of skin irritations due to FI, the use of a voiding diary, and how to manage constipation and fecal impaction. This showed rudimentary and coping knowledge of treatments but not true chronic condition management care knowledge. Again to be expected amongst family members of the demographic interviewed but surprising and disappointing for the PSWs given that this was part of their professional duty when called to the homes in question.
3.3. Confidence Level
- The overall level of confidence that respondents had when dealing with patient/family members with FI varied. Confidence amongst family carers was low with an average score of 4.8/10 across all 9 questions in this category, whereas PSWs had a high confidence level of 8.2/10 - with 10 being extremely confident. This was consistent with the 8.9/10 reported elsewhere for nursing home PSWs [27].Family members were not at all confident when escorting their family member to the washroom on time, dealing with relatives with depression, or taking care of skin irritation. This was fairly consistent with the knowledge levels reported above. Although more confident than family, PSWs were also less confident in dealing with depression and skin irritations than the other items questioned.
3.4. Skill Level
- The overall level of self-skills as reported in the interviews by respondents also greatly varied. Family members believed that their skill levels were low with an average score of 4.0/10, where 10 represented being highly skillful. PSWs, on the other hand, scored higher with 7.5/10. The latter was disappointing given long-term care institutional PSWs scored higher at 9.1/10 [27]. The care of FI in a home-setting is challenging.As with their confidence, family members did not feel they were at all skillful in escorting their relative to the washroom on time, caring for skin irritations, or dealing with their loved one’s depression (when present). PSWs also cited care of skin irritations as something at which they could improve their skills.
3.5. PSW In-class Education
- The PSWs were interviewed about their in-class FI education which, it seems, cannot necessarily be blamed for their lack of confidence and/or skills in some areas of FI management. Generally they reported that their education had been adequate in conveying to them the knowledge and skills to deal with FI. On a10-point scale where 1 equaled no in-class FI education and 10 equaled lots of in-class FI education the average response was 8.0 with the lowest scores being in dealing with odour, escorting to the washroom in time, and changing incontinence products frequently.
3.6. PSW “On-the-job” Training
- PSW interviewees believed they received very good “on-the-job” education and training in FI care. Respondents rated their on-the-job training overall quite highly with an average answer to questions being 8.1/10. The only items that scored below average were in history-taking, dealing with depressed individuals, dealing with odour, and dealing with accidents. The last item was of interest as, by definition, incontinence is an accident waiting to happen (unless managed clinically [28] which neither PSWs nor family members were doing).Several times the issue of depression arose and the inability to understand and handle it along with incontinence. This is indicative of the growing acuity and co-morbidly of home-living patients. Mild depression and onset dementia is quite common amongst men and women living at home who are also incontinent [29] – either co-existent or caused by it. Although this study did not investigate co-morbidities with the incontinence, in the open-ended questions the two additional conditions often were referenced.
3.7. Family Perceptions of FI
- Family carers of family members with FI were asked 7 questions about their perceptions of the home care of FI to reveal some of the challenges they faced in either directly providing care for their loved ones or in arranging public care. Family respondents unanimously reported that:• the cost of incontinence products inhibited them from buying the right products to meet patient needs;• they viewed incontinence as a disability and should be treated as such legislatively to provide greater government subsidization; and• at times they felt stressed to the point of not being able to cope any longer.When asked what the worst thing about caring for someone with FI they responded:• travelling to and from a family member’s residence to provide care;• embarrassment and shame in needing family members to help;• the shame of having others to endure the odour;• pretending all is okay when it is not;• sores preventing getting into a wheelchair and going outside;• accidents;• constant changing of absorbent products; and• repeatedly undressing and redressing.Family carers were also asked what the one thing would be that would make then consider institutionalizing their loved one who was suffering from FI. They responded:• worsening dementia or dementia becoming violent;• if could no longer cope with, clean, change, care for the family member;• the family carer became ill too;• fewer than 2 PSW visits per day; and• worsening (undefined) of the FI.Finally, family interviewees were asked an interview closure question of anything further they wished to contribute to the study. Their answers were:• absorbent and other FI products are expensive; this depresses the incontinent individual to the point of not wishing to go outside which prevents live-at-home carers from going out as well;• accidents when left alone;• high cost of products when living on a fixed income with no government support; and• skin irritation, for the most part, being preventable requiring the carer to be vigilant and diligent.
3.8. PSW Perceptions of FI
- As with the family carers interviewed the PSWs in this study were also asked 7 questions about their perceptions of the care being provided to FI patients in the home. Overwhelmingly (10/12) PSWs worried that caring for incontinence in a home-setting could result in falls and other health concerns possibly leading to unwanted institutionalization – a sequence of events documented in the literature [31, 32]. Most (9/12) felt that their professional training equipped them for consultation on incontinence and (8/12) that they had the right tools and education to support individuals living with FI. Like family carers, PSWs (8/12) too viewed incontinence as a disability. When asked what they felt would help them perform their job more easily, PSWs responded:• more time to work with the patient on continence and other matters; all the time with the patient was spent on “accidents” and nothing else got done, or, accidents were ignored to tend to other matters and patients left in soiled products (multiple responses);• more in-class and on-the-job training whereas mostly now just accrued experience (multiple responses); • having specific products indicated for patients being available and accessible when needed;• enlarged bathrooms so PSWs can work with patients in the bathroom; and• more and better product knowledge to pass onto patient.There seemed to be a bit of a disconnect between the PSWs satisfaction with their education and training with respect to FI and an identified need for more as most of it was accrued on the job. This was consistent with previous findings amongst PSWs in long-term care facilities [27].When asked an interview closure question of anything further they wished to contribute to the study the PSWs answered:• the smell sometimes, especially of stoma bags, can be overpowering for PSWs and patients alike and embarrassing for patients;• PSWs are not allowed to disimpact bowels, insert suppositories;• more pamphlets and educational materials to leave with or go over with patients and family members;• if family members could take patients to the toilet more frequently; and• not all FI products are equally effective for the elderly.
4. Discussion
- The preponderance of the scholarly incontinence literature focuses on UI not FI; on the epidemiology and biomechanics of FI and not the “caring” aspect of the equation; on institutional settings rather than care in the home; and on the clinical rather than the personal – the actual burden FI places on the individual and family. This exploratory study attempted to redress this imbalance. It also corroborated research that shows the increasing acuity levels and number of co-morbidities experienced in homecare today and the need for a new way of thinking about homecare [33].The growing acuity and complexity of care being required in the home setting and the severe restraint of budgets, staffing, time and resources in public health systems, non-clinical staff – such as PSWs in the case of Ontario - are being expected to provide extended levels of care beyond their scope of practice. Based upon the results of this study there is an opportunity for stakeholders to collaborate in moving the at-home paradigm of FI care from one of merely coping to a proper management of the disorder. Based upon this small sample of responses it was clear that several universal themes thread themselves across cases of FI being treated at home. Overall, family care of FI at home was a coping measure limited by time, cost and the ability of the carer to maintain the care regimen required. When FI was combined with onset dementia and skin irritations it made this a situation all the more difficult as family members were not professionally trained and often of a similar age as the FI individual. Outside, paid-for, visiting care provision is often inadequate to supplement or replace family care in the home setting in Ontario, in terms of both quantity and quality, due to fiscal restraint.Given the demographics of the sample interviewed, both PSW and family carer, and the cognitive dissonance among PSWs regarding the value of their formal education and training versus their perceived need for more, it is suggested that informal in situ education and training for both family members and paid care providers follow the principle of “participatory training” as recommended elsewhere by the authors [27]. Pamphlets will not be enough. Small group discussions, practice-by-doing, and the traditional medical model of learn one – do one – teach one will help in the retention and put-to-use of the knowledge being imparted to learners [34].A first tranche of participatory education could include topics such as: the value of using assessments, histories and diaries in moving from coping strategies to disorder management; dealing with people living with incontinence who co-present with depression and onset dementia, and; the timely prevention and proper care of skin irritations accompanying and/or caused by FI and its treatment. Since educational resources are scarce it is also suggested that those tasked with this education seek to partner with vendors of continence supplies and technologies who may have a specialized understanding, body of knowledge and skills to share with PSWs and family carers in the front lines of FI care at home. This potential public-private partnership could benefit the patient, the patient’s family member(s), and their formal care providers. Some of this proposed education may challenge the limits of the scope of practice of PSWs and cross over into territory historically preserved for nursing or others. If so, then the appropriate self-regulatory bodies and government offices should work together to improve the homecare situation for the patient, and overcome historical anachronisms that deny appropriate care whether, by means of delegation, extended practice or other means.The literature shows that FI has been and continues to be highly stigmatized [9, 10, 30] and this stigmatization seems to lead to government support policies that ignore the problem by not recognizing the burden of the disorder as eminent enough for FI to be considered a disability which would entitle it to greater funding and support. The responses about financial barriers provided in this study corroborate this.Although the first study of its kind, the results could be used proactively by homecare service providers, government contracting agencies, patient advocacy groups and provider groups in any publicly funded health system in a post-industrial country where resources are scarce in meeting the growing complex care needs of particularly elders living at home.
5. Conclusions
- This exploratory study of PSWs and family carers taking care of people living at home with FI in Ontario, Canada adds to the field of knowledge qualitative evidence that supports on-going education and training of both paid and volunteer FI care-givers; the long overdue de-stigmatization of FI and the proper listing of it as a disability that impairs livelihood and quality-of-life; and public-private-notforprofit collaboration to optimize the care provided elders living at home with FI.
ACKNOWLEDGEMENTS
- The authors wish to express their appreciation for an unrestricted research grant provided by Essity Hygiene and Health AB (Canada) which made this study possible, as well as the managers and staff at Transcare Community Support Services and the families they serve for the access they gave.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML