-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2018; 8(1): 4-11
doi:10.5923/j.health.20180801.02

Knowledge and Beliefs on Antimicrobial Resistance among Clinicians: Step towards Antibiotic Stewardship
Rucha Ridhorkar1, Neena V. Nagdeo2
1II MBBS Student, NKPSIMS, Nagpur, India
2Associate Professor, Dept. of Microbiology, NKPSIMS, Nagpur, India
Correspondence to: Neena V. Nagdeo, Associate Professor, Dept. of Microbiology, NKPSIMS, Nagpur, India.
| Email: |  |
Copyright © 2018 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

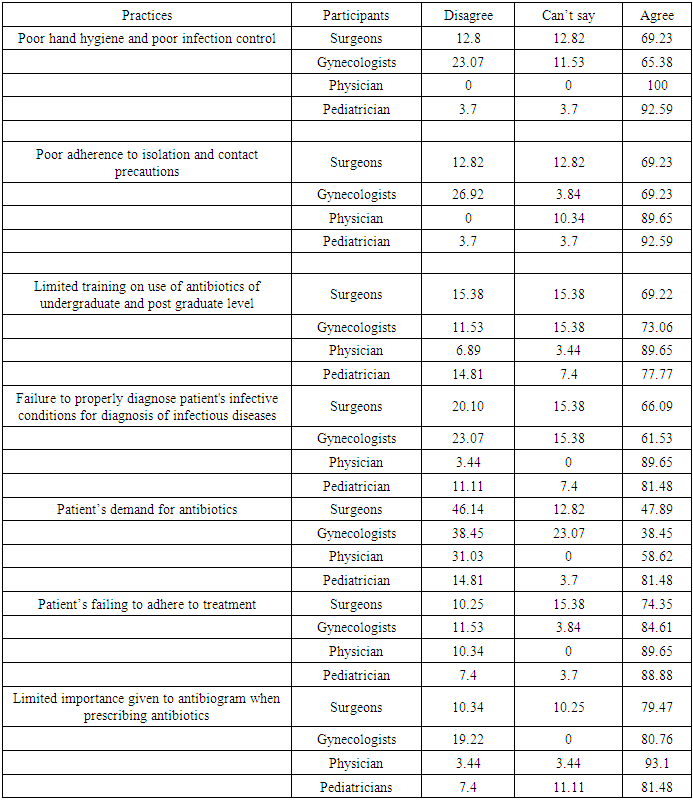
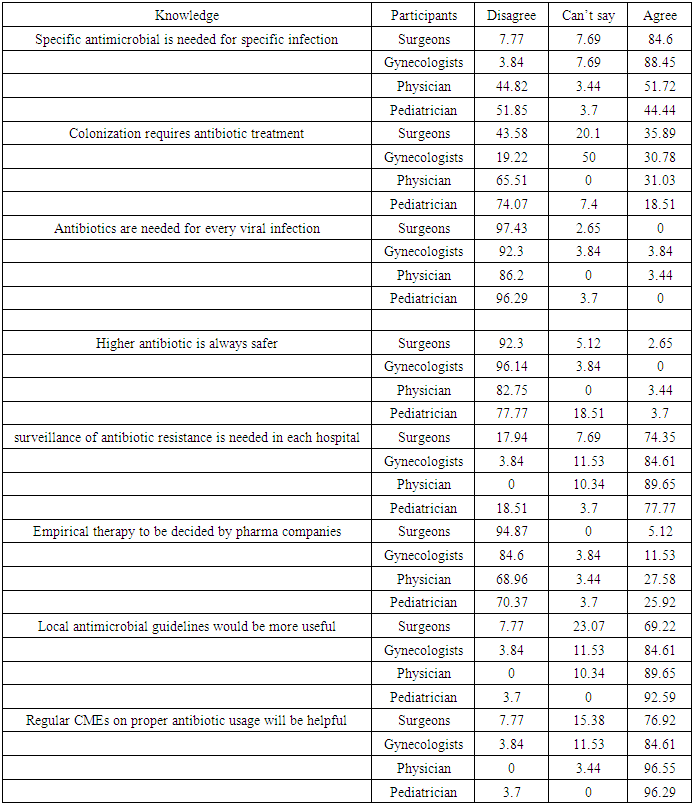
Emergence of antimicrobial resistance is well recognized as a global threat to human health. Antimicrobial stewardship is a coordinated program that promotes the appropriate use of antimicrobials. There is a need for increased education and awareness about inappropriate use of antimicrobials amongst the public and healthcare professionals. Hence this study was planned to conduct a survey, to assess the knowledge and beliefs on antibiotic resistance amongst the clinicians.100 clinicians were included in this study which included physicians, pediatricians. Surgeons and Gynecologists and obstetricians. A structured questionnaire was provided online to the participants. More than 90% of physicians followed by 81% of pediatricians strongly agree that ignorance to antibiogram while prescribing antibiotics is a crucial aspect is promoting antimicrobial resistance. Need of regular Continued Medical Education (CMEs) on proper antimicrobial usage was unanimously agreed upon by all 4 groups.Our study showed that 90% of the pediatricians and physicians agree to poor hand washing and poor infection control practices being the factors responsible for contributing to antimicrobial resistance. Failure to properly diagnose patient's infective conditions for diagnosis of infectious diseases were reasons agreed upon by 60% of surgeons and gynecologists and 90% of physicians and pediatricians. 81% pediatricians and 60% of physicians felt that patient’s demand for antibiotics being contributory. However, 90% of all four groups agreed upon patients failing to adhere to treatment and discontinuing prescribed antibiotics midway the treatment being a significant cause.
Keywords: Antibiotic resistance, Awareness, Knowledge
Cite this paper: Rucha Ridhorkar, Neena V. Nagdeo, Knowledge and Beliefs on Antimicrobial Resistance among Clinicians: Step towards Antibiotic Stewardship, Journal of Health Science, Vol. 8 No. 1, 2018, pp. 4-11. doi: 10.5923/j.health.20180801.02.
1. Introduction
- Emergence of antimicrobial resistance is well recognized as a global threat to human health. Resistance has emerged even to the newer and more potent antimicrobial agents like carbapenems. Antimicrobial resistance is closely linked to inappropriate antimicrobial use. [1] Antimicrobial stewardship is a coordinated program that promotes the appropriate use of antimicrobials, improves patient outcomes, reduces microbial resistance, and decreases the spread of infections caused by multidrug-resistant organisms. Antibiotic Stewardship Programs can both optimize the treatment of infections and reduce adverse events associated with antibiotic use. [2, 3]Misuse and overuse of antimicrobials is one of the world’s most pressing public health problems. Infectious organisms adapt to the antimicrobials designed to kill them, making the drugs ineffective. [1] People infected with antimicrobial-resistant organisms are more likely to have longer, more expensive hospital stays, and may be more likely to die as a result of an infection. [1]There is a need for increased education and awareness about inappropriate use of antimicrobials amongst the public and healthcare professionals. [4] It is imperative to have standardized national treatment guidelines for clinicians so that antimicrobials are used rationally. Many strategies have been proposed for the rational use of antibiotics which can be done through educational interventions and strict antibiotic policy. [4] Knowledge of antimicrobial resistance is important for framing antibiotic policy. [5] Before educating the private practitioners it is necessary to know about the awareness amongst them regarding antibiotic resistance. [4] Hence this study was planned to conduct a survey, to assess the knowledge and beliefs on antibiotic resistance amongst the clinicians.OBJECTIVE: To assess the knowledge of antimicrobial resistance amongst clinicians.
2. Materials and Method
- Type of study- cross sectionalStudy population- 100 clinicians (Private Practitioners) were included in this study. They were divided into 4 groups comprising 25 participants in each group. Group A- physicians.Group B- pediatricians.Group C- surgeons.Group D – Gynecologists and obstetricians.A structured questionnaire was provided online to the participants. The response was analyzed by percentages. All the information obtained during project was not revealed to anyone. Procedure was performed only after obtaining the consent from Health Care Workers (HCWs) and permission from Institutional Ethics Committee of NKPSIMS, Nagpur, India.
3. Results
- The questionnaire was divided into 3 main sections. First was related to questions concerned with practices contributing to antimicrobial resistance (Table 1). Following responses were obtained from the participants.
|
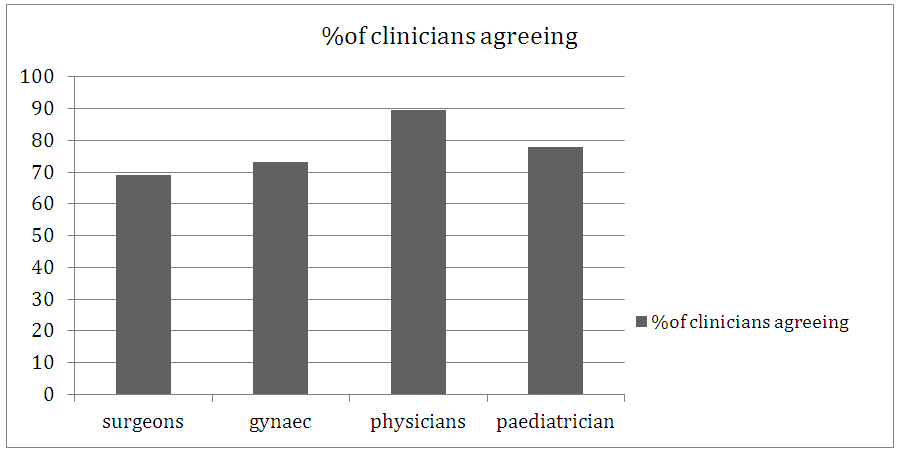 | Figure 1. Inadequate training on use of antibiotics |
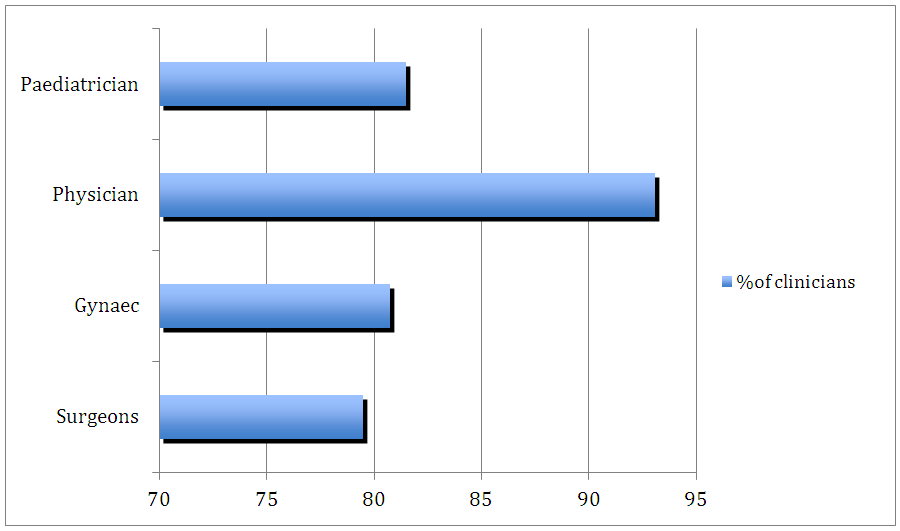 | Figure 2. Ignorance to Antibiogram |
|
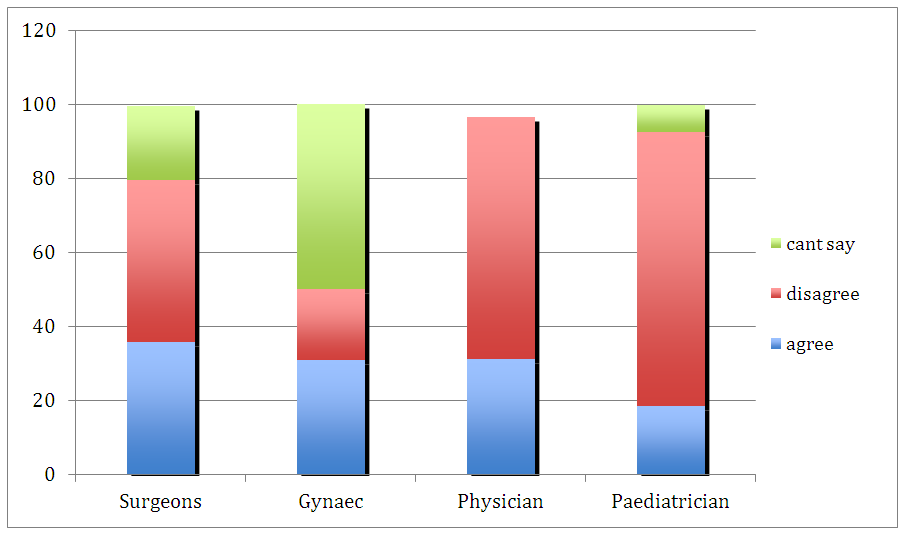 | Figure 3. Responses to need of antibiotics for every viral infection |
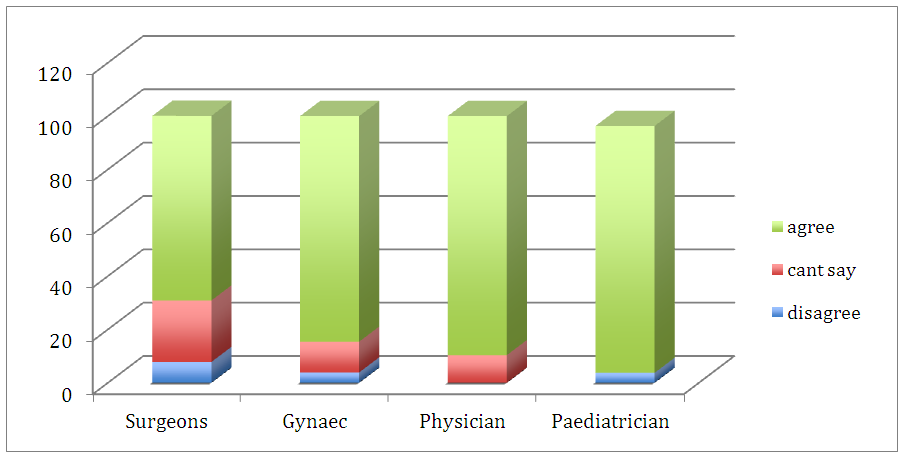 | Figure 4. Responses to need of local antimicrobial guidelines |
|
|
4. Discussion
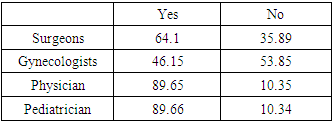
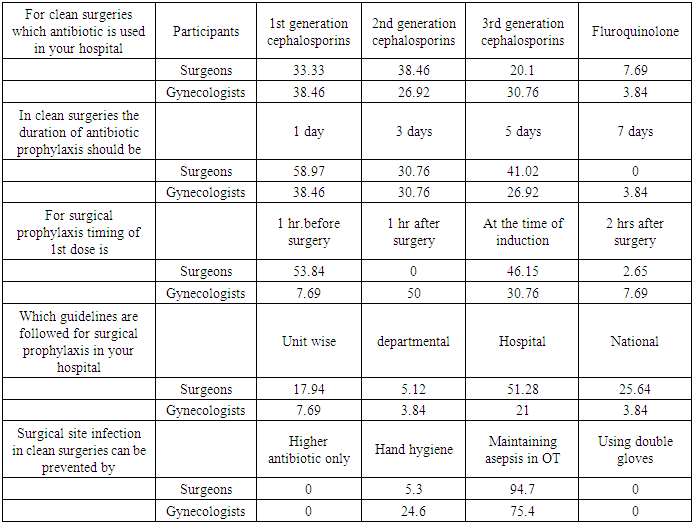
- This study was conducted to assess the knowledge of antimicrobial resistance amongst clinicians. A structured questionnaire was given to all the participants and the responses were analysed. Our study showed that 90% of the pediatricians and physicians agree to poor hand washing and poor infection control practices being the factors responsible for contributing to antimicrobial resistance, whereas only 75% of surgeons agree for the same. In a study conducted by C. William Wester only 45% respondents believed that this is the important cause. [6] Shah et al study showed that only 31% believed in hand hygiene to be significant in reducing antimicrobial resistance. [7] In our study 75% of all of the four groups of clinicians agreed on poor adherence to isolation and contact precautions contributing in antibiotic resistance.Inadequate training on use of antibiotics at undergraduate and postgraduate level is a poignant parameter contributing to antimicrobial resistance. 89% of physicians followed by 77% pediatricians in our study agree that limited training of antibiotics at undergraduate and Post graduate level contribute in development of antimicrobial resistance. Providing education on antimicrobial stewardship for health care professionals was identified as most important intervention to combat anti microbial resistance by Kheder SI. [8]Failure to properly diagnose patient's infective conditions for diagnosis of infectious diseases were reasons agreed upon by 60% of surgeons and gynecologists and 90% of physicians and pediatricians in our study.This study revealed that 81% pediatricians and 60% of physicians felt that patient’s demand for antibiotics being contributory for antimicrobial resistance. However, 90% of all four groups agreed upon patients failing to adhere to treatment being a significant cause. In a study by Bayeh Abera 86% respondents believed patient’s poor adherence to prescribed antibiotics is the reason [9], while in a study done by Giblin et al 68% participants agreed for this factor [10] and in a study by N. Shanmuga vadivoo 93% agreed for poor adherence to treatment and 54% participants believed that patient’s demand for antibiotics contribute for antimicrobial resistance. [11] Responses to limited importance given to antibiogram when prescribing antibiotics in our study shows that more than 90% of physicians followed by 81% of pediatricians strongly agree that it is a crucial aspect is promoting antimicrobial resistance. Study conducted by Bayeh Abera states that 12.3% clinicians felt that there is a lack of access to local antibiogram. [9] Second section was regarding knowledge and awareness regarding antimicrobial agents used by the participants in our study. 80% of surgeons, gynecologists and only 50% of physicians and 44% Pediatricians agreed upon need of specific antimicrobial for specific infection whereas 44% of pediatricians disagreed. In a study conducted by Srinivasan A, 97% participants agreed that better use of antimicrobials would help to decrease resistance. [12] While Costelloe C [13] reported that of the 170 physicians who completed the survey, 88% agreed antibiotics are overused in general.In our study 75% of paediatricians, 50% of surgeons and physicians and only 19% of gynaecologists disagreed for use of antibiotic in case of colonization. More than 90% of all four groups strongly disagree upon antibiotics being needed for every viral infection and higher antibiotic being always safer. Study by C William Wester states that 97% physicians believed that widespread and inappropriate use of antibiotics were important cause of antibiotic resistance. [6]In this study 90% participants agreed upon the need of surveillance of antibiotic resistance in each hospital. 90% of surgeons and gynecologists disagreed upon empirical therapy to be decided by pharma companies whereas about 70% of physicians and pediatricians disagreed. In response to need of local antimicrobial guidelines, 70% of surgeons and 90% of gynecologists, physicians and pediatricians agreed. Shrinivasan A. mentioned in his study 77% participants believed that locally developed guidelines for antimicrobial use would be more useful than national guidelines. [12]Need of regular CMEs on proper antimicrobial usage was unanimously agreed upon by all 4 groups in our study. While 65% physicians responded that they need further training on antibiotic stewardship as reported by Bayeh Abera. [9] Costelloe C in his study mentioned that 90% wanted more education about antimicrobials and 67% wanted more feedback on antimicrobial selections. [13] Our study shows that about 90% of Physicians and Pediatricians have attended some sessions on Rational use of antibiotics whereas only 64% of surgeons and 46% of gynecologists have undergone some training. Jennifer Bowes Reported 74.2% had formal training in rational use of antibiotics. [14]For surgical antimicrobial prophylaxis by surgeons and Gynecologists the responses in our study shows that around 30% participants in both the groups are using First, Second and Third generation cephalosporins for surgical prophylaxis. According to ASHP guidelines first generation cephalosporin cefazoline is regarded as the drug of choice which is effective against commonly encountered organisms in surgical procedures and has a relatively low cost. [15] In a study conducted by Neena Nagdeo third generation cephalosporin Ceftriaxone was used in 67.5% cases in pre interventional analysis and prophylactic agent was continued for 3-5 days. [16] In our study 50% of both groups agreed upon duration of antibiotic prophylaxis to be of 1 day.Optimal timing of antibiotoic administration is considered an important factor for effective prophylaxis. [17] Inappropriate timing may result in low plasma concentration of the antimicrobial agent at the time of incision and throughout the procedure contributing to higher infection rates. [18] In our study only 40% surgeons and 30% Gynecologists know that timing of antibiotic prophylaxis should be at the time of induction. More than 90%of surgeons and 75% of gynecologists believe that maintaining asepsis in Operation Theatre can contribute in prevention of surgical site infection .Rest believe in proper hand hygiene. Antibiotics used empirically in 80% of the hospitals included ceftriaxone and fluroquinolone in our study whereas Amoxycillin and cloxacillin are most commonly prescribed antibiotics in Ethiopia. [19]More than 90% of surgeons and 75% of gynecologists believe maintaining asepsis in OT can contribute in prevention of surgical site infection in clean surgeries. Rest believe in proper hand hygiene.
5. Conclusions
- Antimicrobial resistance is closely linked to inappropriate antimicrobial use. Antibiotic Stewardship Programs can both optimize the treatment of infections and reduce adverse events associated with antibiotic use. Knowledge of antimicrobial resistance is important for framing antibiotic policy. Before educating the private practitioners it is necessary to know about the awareness amongst them regarding antibiotic resistance. Hence this study was planned to conduct a survey, to assess the knowledge and beliefs on antibiotic resistance amongst the clinicians.The data generated will help in policy formulation and program development for educating the clinicians regarding appropriate use of antibiotics, which will be a first step towards antibiotic stewardship program.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML