-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2017; 7(2): 33-37
doi:10.5923/j.health.20170702.03

Demographic Characteristics and Management Challenges of Retnal Vein Occlusion in Ekiti State, Nigeria
Iyiade Adeseye Ajayi, Olusola Joseph Omotoye, Ajite Kayode Olumide, Titilope Taiwo Alegbeleye, Funmilola Kumolalo
Department of Ophthalmology, Ekiti State University Teaching Hospital, Ado-Ekiti, Nigeria
Correspondence to: Iyiade Adeseye Ajayi, Department of Ophthalmology, Ekiti State University Teaching Hospital, Ado-Ekiti, Nigeria.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

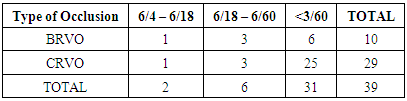
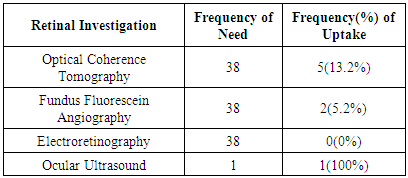
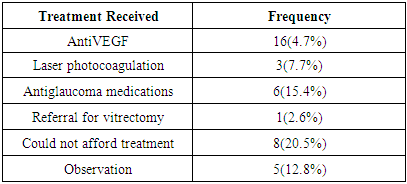
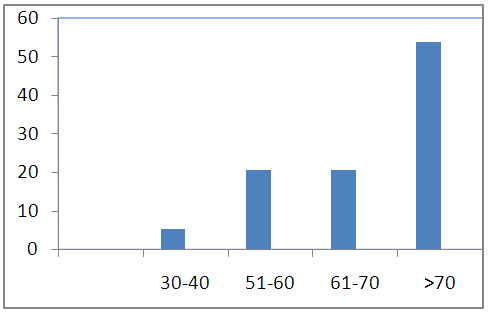
AIM: To assess the demographic characteristics and risk factors among patients with RVO in a state-owned tertiary eye care centre and to review the challenges in the management of these patients. Methods: Medical records of all consecutive new patients diagnosed as having any form of RVO over a 3year period were extracted from the Retinal disease register. Demographic characteristics, history of systemic conditions and ocular diseases were obtained. Record of Visual acuity at presentation, total cholesterol, Intraocular pressure at presentation as well as uptake of recommended investigations were recorded. Data were analysed using Statistical Package for Social Sciences 20.0. Statistical significance was inferred at P < 0.05. Results: RVO accounted for 39(9.63%) of retinal diseases in our centre. The age of the patients ranged from 38-85years with a mean age of 68.1years (SD 12.4). Majority of the patients (94.8%) were aged above 50years. Females were more with a male to female ration ratio of 1: 1.6. Central RVO accounted for 29(74.4%) of the cases. There were 31(71.5%) of the patients with visual acuity less than 3/60 at presentation. Many of our patients had late presentation ranging from 1month to 48months after the onset of symptoms, with high incidence of complications like macular edema 22(56.4%), retinal neovascularisation 9(23.1%), neovascular glaucoma 4(10.3%). Hypertension 29(74.4%), diabetes 6(15.4%) and hyperlipidemia 6(15.4%) were the common systemic conditions found while glaucoma was a common ocular disorder in 20(51.3%) of our patients. CONCLUSION: RVO was a common retinal disorder in our centre with patients with CRVO accounting for a larger percentage with more females than males. Many patients presented with complications of chronicity and a greater number could not carry out the required investigations because of financial constraints.
Keywords: Retinal vein occlusion, Challenges, Management, Central retinal vein occlusion, Branch retinal vein occlusion
Cite this paper: Iyiade Adeseye Ajayi, Olusola Joseph Omotoye, Ajite Kayode Olumide, Titilope Taiwo Alegbeleye, Funmilola Kumolalo, Demographic Characteristics and Management Challenges of Retnal Vein Occlusion in Ekiti State, Nigeria, Journal of Health Science, Vol. 7 No. 2, 2017, pp. 33-37. doi: 10.5923/j.health.20170702.03.
Article Outline
1. Introduction
- Retinal vein occlusion (RVO) is a retinal vascular disorder characterized by engorgement and dilatation of the retinal veins with secondary intraretinal hemorrhages mostly, intraretinal edema, retinal ischemia including cotton wool spots, retinal exudates and macular edema [1]. It is the second most common sight-threatening retinal vascular disorder after diabetic retinopathy [2, 3]. In the developing countries where about 90% of the world’s blind population reside, retinal diseases are among the leading causes of blindness after cataract [4].Depending on the site of occlusion, the two broad types of RVO are 1) Central retinal vein occlusion (CRVO) wherein the whole retinal venous system is involved with the presumed site of increased venous outflow resistance located at or posterior to the lamina cribrosa and; 2) Branch retinal vein occlusion (BRVO) where the venous engorgement involves only branches of the retinal venous network [5]. Hemi-CRVO is a terminology used for a particular variant of CRVO where only one of the two trunks of an intraneural central retinal vein is occluded.The pathogenesis of RVO is still not completely understood but the condition has been reported to be due to a combination of three systemic changes (Virchow’s triad) which comprises venous stasis, degenerative changes of the vessel wall and blood hypercoagulability [6]. There are recognized ophthalmic and systemic risk factors among which are hypertension, hyperlipidemia, diabetes mellitus, hypercoagulable state, prior stroke, glaucoma and reduced ocular perfusion pressure [5]. A study in the developed world found no gender disparities in the occurrence of the disease [7]. Retinal ischemia and macula edema are the most common vision threatening complications in RVO [8] with potential severe consequences for the people affected, including visual loss with costly social repercussions [9]. The introduction of powerful diagnostic tools such as Spectral Domain Optical Coherence Tomography and the widespread diffusion of Intravitreal drugs such as Vascular Endothelial Growth Factor inhibitors or implantable steroids have dramatically changed the management and prognosis of RVO [10].
1.1. Study Objective
- The purpose of this study was to assess the demographic characteristics and risk factors among patients with RVO in a state-owned tertiary eye care centre as well as to report the challenges in the management of these patients. The result from this study will assist in planning towards preventing avoidable blindness in RVO.
2. Subjects and Methods
- Ekiti State University Teaching Hospital is a semi urban tertiary hospital with an established tertiary eye care service wherein there is a retina subspecialty clinic where all patients with retinal diseases are seen on a weekly scheduled clinic day. Medical records of all consecutive new patients diagnosed as having any form of RVO over a 3year period from January 2013 to January 2016 were extracted from the Retinal Disease Register. Ethical clearance was obtained from the Institutional Ethics and Research Committee. The study was conducted in line with the ethical standard according to the declaration of Helsinki. Data obtained included demographic characteristics and history of systemic conditions like hypertension, diabetes mellitus, hyperlipidemia and stroke. Presenting visual acuity were recorded. WHO guideline was used to grade the visual acuity (VA) with ≥6/18 as normal, <6/18 to >3/60 as visual impairment and <3/60 to no light perception as blindness. Intraocular pressures at presentation were recorded. For ease of computation, visual acuity was also entered as number of Snellen acuity chart lines read. Refractive status as well as numerical values of refractive error were recorded as spherical equivalent. Previous diagnosis or diagnosis of glaucoma at presentation was noted. Any other associated ocular morbidity was also noted. Patients uptake of required investigations and treatment offered was assessed.
2.1. Definition of Terms
- The diagnosis of ischemic CRVO was guided by the presence of clinical and functional features like poor VA, relative afferent papillary defect (RAPD), presence of multiple dark, deep intraretinal hemorrhages and multiple cotton wool spots [7, 10].Hyperlipidemia was defined as total cholesterol ≥7mmol/L while hypertension was defined as BP > 140/90mmHg measured on 2 or more times while patient was seated or previous diagnosis of hypertension [11].Data were analyzed using Statistical Package for Social Sciences 20.0. Means (Standard deviations) were used to describe the distributions of continuous variables. Categorical variables were described in percentages. Comparisons of categorical data were performed with the use of Pearson's chi-square test and statistical significance was inferred at P < 0.05.
3. Results
- Thirty-nine patients had retinal vein occlusion. This constitutes 9.63% of 375 retinal disorders seen during the period of study. The age ranged from 38years to 85years. Mean age was 68.08 years (SD ±12.41). There were 15(38.5%) males and 24 (61.5%) females giving a male: female ratio of 1:1.6.
 | Figure 1. Age Distribution of Respondents |
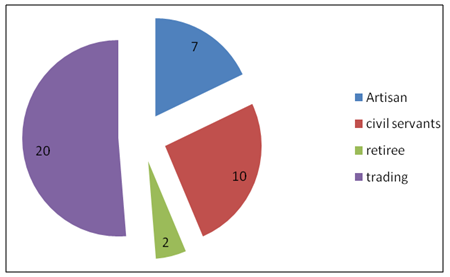 | Figure 2. Occupational Distribution of Patients |
|
|
|
4. Discussion
- Retinal vein occlusion constituted 9.4% of the patients with retinal disorders in our centre. This reiterates the fact that retinal vein occlusions are common retinal vascular disorders. This observed incidence is however slightly higher than those in reports from the south-south (27/364 in 5years, 7.4%) [12] and south-east [13] regions of our country. A much lower prevalence of 5.2 per 1000 have been reported in the United States, Europe, Asia and Australia [7]. BRVO constituted 8.96% of vitreoretinal disorders in Nepal [14]. The mean age of our patients was 68.1(SD 12.4) years with majority of them above 50years of age. This agrees with the fact that RVO presents mainly in the older population [7, 12] with more than 90% of cases of RVO occurring in the age group over 50 years [15]. We found more females than males in this study. This is also similar to the report from Fiebai et al [12] and Stem et al [16] but contrary to reports from the Western populations where male preponderance have been reported [6, 17]. Rogers et al from their prevalence study which consisted of combined data from 15 studies observed no gender difference in both BRVO and CRVO [7].There were more cases of CRVO (71.8%) than BRVO (28.2%) in this study. This finding though in agreement with the study by Fiebai et al from south south Nigeria [12] is contrary to studies from the western world where BRVO have been reported to be more prevalent [7, 8, 18]. Ischemic CRVO constituted about 64.1% of all cases, a value about six times the number of Non-ischemic cases. Majority of the patients presented with blindness in the affected eye. Most of these patients had central retinal vein occlusion. Typically, a patient with CRVO complains of a progressive, painless, and severe decrease in visual acuity (VA), without other symptoms. Loss of VA is usually more pronounced with ischemic compared with nonischemic CRVO [9, 19]. The VA at presentation has been demonstrated to have a key prognostic significance with an initial VA of 20/40 or better associated with a more favorable visual prognosis [20]. A review of the natural course of the disease has shown that the vision in patients with CRVO will most likely worsen or remain unchanged and that patients with poor vision initially have little hope of significant spontaneous recovery [11].There was a delay in presentation among our patients with varying duration up to 48months and mean of 7.2 months (SD 6.2). Good evidence exists to show that early treatment can be beneficial and that the risk of permanent structural damage to the fovea, poor visual prognosis and neovascularisation increase with prolonged duration of RVO [7, 9, 11].About 51.3% of the patients had glaucoma at presentation with a mean IOP of 21.30mmHg (SD 8.89). The patients with BRVO had relatively lower IOP compared with those with CRVO (P=0.048). Glaucoma has been reported as the most common ocular factor predisposing subjects to RVO with association in both CRVO [6, 21] and BRVO [6]. The increased IOP is thought to compromise retinal vein outflow and produce stasis. The higher risk of CRVO in blacks compared with whites has been further attributed to the higher prevalence of glaucoma in blacks [16].More than 70% of the RVO patients were hypertensive. Hypertension has been observed to be a predominant finding in 88% of recurrent RVO [22, 23]. We did not observe any significant greater odd for BRVO among our hypertensive patients. Some patients also had diabetes mellitus (15.4%). We found out that all our RVO patients with DM were also hypertensive. The diagnosis of hyperlipidemia was also made in another 15% of cases. None of the patients ever had stroke. Cardiovascular risk factors have been reported to be usual findings among RVO cases greater than 50years of age [25]. The above findings are similar to the findings by Fiebai [12] and Nwosu [13] although we have higher prevalence of hypertension and hyperlipidemia among our patients. Macular edema (56.4%), retinal neovascularisation (23.1%) and neovascular glaucoma (10.3%) were common features present in some patients at the time of presentation. Macular edema has been reported to be the most important cause of reduced vision in patients with RVO [17]. Retinal neovascularisation and neovascular glaucoma are usual features of ischemic RVO with greater correlation with increasing extent of non perfused retinal area and the development of anterior segment neovascularisation and neovascular glaucoma have been reported to occur in up to 23% of cases within 15months of occlusion [19]. The delay in presentation among our patients can also be a contributory factor to the high rate of features of complications like neovascularisation and blindness at presentation as delayed treatment have been found to decrease the ability of patients to benefit from treatment [22]. The uptake of investigations was very low (OCT 13.2%, FFA 5.2%). Most patients were financially handicapped so much so that about 20.5% could not afford the cost of prescribed line of treatment. Spectral domain OCT is an important tool in the management of patients with RVO as it helps to identify the location and quantity of edema within the retinal layers and subretinal space [26]. Fluorescein angiography as a complement helps to determine the degree of vascular incompetence as well as enlargement of the foveal avascular zone. Both investigations are required at baseline and for periodic check during follow up in patients with RVO. We observed from the occupation of these patients that majority were in the category of artisans, retiree and traders who are mostly low income people in this environment as their incomes are largely tied to the economy of the civil servants. Moreso these patients have no access to insurance cover and the available OCT facilities are located mostly in private-owned centres some considerable distance away from the state. The average cost of OCT and FFA in Nigeria is about 200 dollars each per check inclusive of transportation for our patients with the nearest available centre about 9hours return journey by road. The challenge with this is that for most of these patients who could not afford investigations treatment had to be based on clinical judgement only. For those who could not afford treatment the care givers were totally handicapped. Despite these odds, 47% of our patients benefitted from antiVEGF injection precisely bevazicumab and ranibizumab depending on their financial capabilities. 7.7% had retinal photocoagulation and one patient who had vitreous hemorrhage at presentation was referred for vitrectomy. All patients with coexisting medical conditions were also appropriately directed to relevant specialities for management. Newly diagnosed glaucoma patients were commenced on antiglaucoma medications and referred for co-management with the glaucoma specialist.Post treatment visual acuity assessment revealed 46.2% with 1 line visual gain, 23.1% with 2line visual gain and 12.8% with 3line visual gain.
5. Conclusions
- RVO is a relatively common condition in our centre. CRVO was found to be more common than BRVO with a female preponderance in both cases. The affected age group were mostly people above 50years of age although age as low as 38years was recorded. Many of our patients had late presentation with high incidence of complications like macular edema, neovascular glaucoma, retinal neovascularisation and blindness. Hypertension, diabetes and hyperlipidemia were systemic conditions found while glaucoma was a common finding in over 50% of our patients. Most patients were not able to do the required investigations due to financial constraints. Despite this, some patients who could afford treatment benefitted from antiVEGF, Laser and appropriate referral where necessary. We had varying degrees of visual improvement among some patients and believe advancing medical research have revolutionized treatment options for RVO patients as against the previous common notion of watchful waiting with limited options.
6. Recommendations
- We recommend an increased health awareness programme to enhance early presentation among patients with eye problems. We also recommend that the Government commence policies that will make health care more accessible and affordable. This we believe will improve on patients uptake of investigations and treatment.
ACKNOWLEDGEMENTS
- We wish to acknowledge Dr E.A Ajayi for taking time to read through the manuscript.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML