-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2017; 7(1): 7-8
doi:10.5923/j.health.20170701.02

Dyschromatosis Symmetrica Hereditaria (DSH): A Case Report with Unusual Presentation
Khalid Al Hawsawi 1, Samaher Ibrahim Alaauldeen 2, Nouf Hassan Albarnawi 2, Wafaa Abdulkareem Altaezi 2, Rawan Eid Hudairy 2, Waseem Alhawsawi 3, Bugis Lina 4
1Dermatology Consultant, Head of Dermatology Department, King Abdul Aziz Hospital, Makkah, Saudi Arabia
2Medical Intern, Umm Al-Qura University, Makkah, Saudi Arabia
3King Saud Bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
4Umm Al-Qura University, Makkah, Saudi Arabia
Correspondence to: Khalid Al Hawsawi , Dermatology Consultant, Head of Dermatology Department, King Abdul Aziz Hospital, Makkah, Saudi Arabia.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Dyschromatpsis symmetrica hereditaria (DSH), acropigmentation of Dohi, and reticulate acropigmentation of Dohi are all synonyms of one condition. DSH is a genetic pigmentary skin condition of autosomal dominant inheritance characterized by presence of mixture of hypopigmented and hyperpigmented macules on dorsae of hands and feet. It rarely affects the face and distal parts of fore-arms and legs. The generalized form of this disease is called dyschromatosis universalis hereditaria. Here-in we reported unusual case of DSH, being a late onset as well its localization to the feet only. A 30-year-old female presented with 15-year- history of asymptomatic slowly progressing skin lesions on her feet. Family history revealed presence of similar case in her father. There is no consanguinity between her parents. Skin examination revealed multiple non-scaly hypopigmented and hyperpigmented macules on dorsae of her feet. Wood lamb examination showed no enhancement. According to the above clinical findings, a diagnosis of DSH was made. Patient was reassured that this is a hereditary disease that has no curative treatment. It does not progress. It is localized to dorsae of hands and feet. She was satisfied by using camouflage. She refused the other modalities of the treatment.
Keywords: Dyschromatpsis symmetrica hereditaria, Reticulate acropigmentation of Dohi, Acropigmentation of Dohi
Cite this paper: Khalid Al Hawsawi , Samaher Ibrahim Alaauldeen , Nouf Hassan Albarnawi , Wafaa Abdulkareem Altaezi , Rawan Eid Hudairy , Waseem Alhawsawi , Bugis Lina , Dyschromatosis Symmetrica Hereditaria (DSH): A Case Report with Unusual Presentation, Journal of Health Science, Vol. 7 No. 1, 2017, pp. 7-8. doi: 10.5923/j.health.20170701.02.
1. Introduction
- Dyschromatpsis symmetrica hereditaria (DSH), acropigmentation of Dohi, and reticulate acropigmentation of Dohi are all synonyms of the same condition. DSH is a rare autosomal dominant hereditary skin disease. Few cases of autosomal recessive inheritance have been reported. It was first described by Toyama in 1929. [1] It is characterized by presence of mixture of hypopigmented and hyperpigmented macules on dorsae of hands and feet. It rarely affects the face and distal parts of fore-arms and legs. [1, 2] It is caused by heterozygous mutations in ADAR (DSRAD) gene that encodes double stranded RNA-specific adenosine deaminase. The gene locus responsible for DSH has been mapped to chromosome 6q24.2 – q25.22. [3-5] Majority of patients are Japanese or Chinese. DSH appears during infancy or early childhood and stops spreading before adolescence and persists for life. [1, 3]
2. Case Report
- A 30-year-old female presented with 15- years - history of asymptomatic slowly progressing skin lesions on her feet. Patient has been seen by many dermatologists where she was diagnosed to have vitiligo. She was prescribed topical treatment for vitiligo but without benefit. Family history revealed presence of similar case in her father. There is no consanguinity between her parents. Past medical history and review of system were unremarkable. Skin examination revealed multiple non-scaly hypopigmented and hyperpigmented macules on dorsae of her feet (figure 1). Wood lamb examination showed no enhancement. According to the above clinical findings, a diagnosis of DSH was made. Patient was reassured that this is a hereditary disease that has no curative treatment. It does not progress. It is localized to dorsae of hands and feet. It rarely affects the face and distal parts of fore-arms and legs. The patient was satisfied by using camouflage. She refused the other modalities of the treatment.
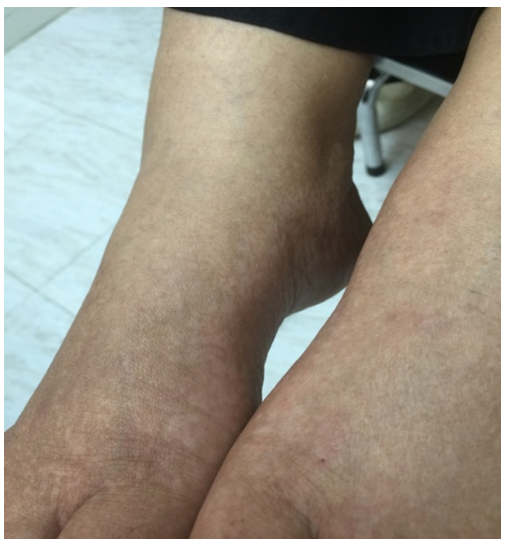 | Figure 1. Dorsae of feet of the patient showing mixture of non-scaly hypopigmented and hyper pigmented macules |
3. Discussion
- DSH is a rare pigmentary hereditary skin condition. It is characterized by numerous small rounded hypopigmented and hyperpigmented macules on dorsae of hands and feet. It rarely affects the face and distal parts of fore-arms and legs. [1-5]The onset of DSH usually appears during infancy or early childhood. Our patient showed a late onset DSH. It appeared first at the age of 15- year- old. The other unusual feature in our case was the absence of lesions on her hands. In some patients with dyspigmentary skin disorder, one might not be able to see both hyper-pigmentation and hypo-pigmentation but a careful examination will enable you to see both hyper-pigmentation and hypo-pigmentation.The diagnosis of DSH is a clinical diagnosis. The main differential diagnosis in our patient was vitiligo. Our patient has hyper-pigmented macules in-between the hypo-pigmented macules. This late feature is typical for DSH.Neurological manifestations have been reported to be associated with DSH in minority of cases. [6] Our patient has no neurological manifestations. Histopathologically, the hyperpigmented macules of DSH show increased number of melanocytes in the epidermis, whereas the hypopigmented macules show decreased number of melanocytes in the epidermis. [1, 4] Treatment of DSH includes camouflage, miniature-skin graft, and excimer laser therapy. [7] Our patient was satisfied by using camouflage. She refused the other modalities of the treatment.
4. Conclusions
- DSH is a rare autosomal dominant hereditary pigmentary skin disorder. It is characterized by presence of mixture of numerous small rounded hypopigmented and hyperpigmented macules on dorsae of hands and feet. It rarely affects the face and distal parts of fore-arms and legs. The diagnosis of DSH is a clinical diagnosis. The main differential diagnosis in our patient was vitiligo. Presence of mixture of hyper-pigmented macules and hypo-pigmented macules on dorsae of hands and /or feet is typical for DSH. The main treatment is by reassuring the patient. Camouflage, miniature-skin graft, and excimer laser therapy have all been tried for treatment of this condition.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML