-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2016; 6(5): 74-76
doi:10.5923/j.health.20160605.02

Erythema Annulare Centrifugum (EAC): A Case Report of Annually Recurring EAC
Hana Mshrai1, Boshra Fallatah1, Danya Alwafi2, Doaa Babkoor2, Haneen Al Sufyani1, Khalid Al Hawsawi3
1Medical intern, King Abdul Aziz Hospital, Makkah, Saudi Arabia
2Dermatology Resident, King Abdul Aziz Hospital, Makkah, Saudi Arabia
3Dermatology Consultant, Head of Dermatology Department, King Abdul Aziz Hospital, Makkah, Saudi Arabia
Correspondence to: Khalid Al Hawsawi, Dermatology Consultant, Head of Dermatology Department, King Abdul Aziz Hospital, Makkah, Saudi Arabia.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Erythema annulare centrifugum (EAC) is one of the figurate or annular erythemas. It is uncommon inflammatory condition characterized by persistent annular or arcuate erythematous eruptions that slowly enlarge centrifugally. Although EAC can be recurrent, annual recurrence is an unusual feature of EAC. Here in we present a 60- Year-old female who is a known case of hypothyroidism on L-thyroxine treatment, presented with 3- Year- history of recurrent slightly itchy skin lesions that recur once every year. Skin examination revealed multiple annular scaly erythematous plaques, ranging in size as small as 2 cm to as large as 10 cm over her arms, chest and thighs with a characteristic pattern of the scales that are arranged in a trail like pattern. Skin biopsy showed mild hyperkeratosis, mild spongiosis, and sparse perivascular mononuclear cellular infiltrate in the upper dermis. The patient was empirically treated with itraconazole capsule 200mg once daily for one month. The lesion disappeared and did not recur until time writing this paper for 18 months ago.
Keywords: Erythema Annulare Centrifugum, Figurate erythema, Erythema gyratum perstans
Cite this paper: Hana Mshrai, Boshra Fallatah, Danya Alwafi, Doaa Babkoor, Haneen Al Sufyani, Khalid Al Hawsawi, Erythema Annulare Centrifugum (EAC): A Case Report of Annually Recurring EAC, Journal of Health Science, Vol. 6 No. 5, 2016, pp. 74-76. doi: 10.5923/j.health.20160605.02.
1. Introduction
- Erythema annulare centrifugum (EAC) is one of the figurate erythemas. It is uncommon inflammatory condition characterized by polycyclic erythematous eruptions that slowly enlarge centrifugally in a rate of 1 to 3 mm/day. [1-3] It was first described by Darier in 1916. The incidence was reported to be approximately 1 case per 100,000 population per year. [1-5] Etiology of EAC is unknown, but it is probably due to a hypersensitivity reaction to a variety of agents, including drugs (penicillin, salicylates, hydrochlorothiazide), arthropod bites, infections (bacterial, mycobacterial, viral, fungal, filarial), food allergy (blue cheese Penicillium), malignancy as (lymphoma, multiple myeloma, breast cancer ), autoimmune and endocrine disease ( Hashimoto Thyroiditis, Sjogren syndrome). [4-8] Familial cases of EAC have been reported as "familial annular erythema". [5] EAC generally is classified into superficial type which is clinically characterized y by presence of trailing scales at edges of the lesions and histopathologically by presence of perivascular cellular infiltrate in superficial dermis with pronounced epidermal changes, and deep type which is characterized clinically by having infiltrated borders and histopathologically by presence of perivascular cellular infiltrate in the deep dermis with minimal epidermal changes. [3-8] EAC occurs at any age but more commonly in fifth decade of life. Male to female ratio are equal. It can present at any part of the body but more commonly on trunk, the thigh, the legs and buttock. [7-9] A characteristic histopathological feature of EAC is the presence of a “coat sleeve” pattern of the perivascular cellular infiltrate in the dermis. “Coat sleeve” pattern is a tight (sharply demarcated) mononuclear cellular infiltrate around blood vessels of the dermis. EAC is self-limited disease with variable course that lasts as little as few weeks or as long as three decades. [3-7]
2. Case Report
- A 60 Year-old- female who is a known case of hypothyroidism on L-thyroxine treatment for the last 2 years, presented with 3- Year- history of recurrent slight itchy skin lesions. Over the last 3 years, every year she develops skin lesions that start as small pimples which then expand slowly every day forming a large rings that persist for few months and then start to disappear gradually without treatment. Systemic Review, past medical history and family history were all unremarkable. Skin examination revealed multiple annular scaly erythematous plaques of variable sizes ranging from 2 cm to 10 cm over her arms, chest and thighs with scales that have a trail like pattern (Figure 1). Skin biopsy taken from the edge of the lesion showed mild hyperkeratosis, mild spongiosis, and sparse perivascular mononuclear cellular infiltrate in the upper dermis (Figure 2). Skin scrapping for KOH and fungal culture were negative. Complete blood counts, peripheral blood film, ESR, blood urea, creatinine, liver function tests, blood sugar, Thyroid function tests, VDRL test, urine examination, X-ray chest, abdominal ultrasonography were within normal limits, or normal or negative. On the basis of the above clinicopathological findings, the diagnosis of Erythema Annulare Centrifugum was made. The patient was treated empirically with itraconazole capsule 200mg once daily for one month. The lesions disappeared and did not recur until time of writing this paper for 18 months ago.
 | Figure 1. Multiple annular erythematus plaques with scales in a trail like pattern |
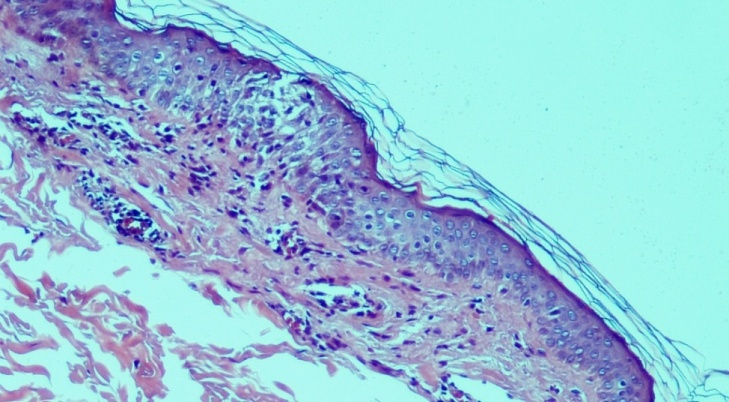 | Figure 2. Histopathological features of the skin lesions showing mild hyperkeratosis, mild spongiosis, and sparse perivascular mononuclear cellular infiltrate in the upper dermis |
3. Discussion
- EAC is a rare benign inflammatory condition presents as polycyclic erythematous eruptions that slowly enlarge centrifugally. The border of the expanding ring may be topped by microvesicles or may show a fine collarette of scales on its trailing edge. [3-8] EAC may be under diagnosed since there are many conditions that look similar to EAC, these include tinea corporis, subacute cutaneous lupus erythematous, annular pityriasis rosea, erythema migrans, erythema marginatum, erythema gyratum repens and secondary syphilis. [3-8] Although trailing scales can also be seen in pityriasis rosea and tinea corporis, recurrence is not a feature of pityriasis rosea. The less pronounced scales as well as the negative fungal culture are not in favor of tinea. Absence of constitutional symptoms, and absence of history of travel abroad are against erythema migrans. Erythema gyratum repens is characterized by concentric rings with wood-grain appearance. The skin lesions that expand in a rate of 1 to 3 mm/day with trailing scales are highly suggestive for EAC. EAC in our case could be secondary to hypothyroidism in spite that its onset was before the hypothyroidism. However the persistence of EAC after treatment of hypothyroidism can be explained by the fact that the exact cause of EAC is still unknown. Although EAC can be recurrent, annual recurrences, like in our case, is an unusual feature of EAC. Similar cases have been described in the literature. [8] EAC usually resolves once the underlying disease has been successfully treated. [9] Topical medications like corticosteroids, tacrolimus, calcipotriene, oral metronidazole, subcutaneous etanercept and subcutaneous interferon-α have been all used with some benefit. Some authors recommend the empiric use of antibiotics or antifungal for the treatment of EAC. Although our patient responded well to empiric use of itraconazole, this does not indicate that the underlying cause was a fungal infection because EAC is self limited disease. [9]
ACKNOWLEDGMENTS
- No sources of funding were used to assist in preparation of this manuscript. The authors have no conflicts of interest that are directly relevant to the content of this review.
Consent Statement
- Consent has been taken from the patient for purpose of using patient's photographs for publication in print or on the internet.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML