-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2016; 6(2): 22-29
doi:10.5923/j.health.20160602.02

The Effectiveness of Different Health Education Strategies in People with Pre-diabetes: A Randomized Controlled Trial
Shu-Chuan Chang 1, Mark Hayter 2, Hsiu-Chen Yeh 3, Tsung-Cheng Hsieh 4, Yu-Lun Kuo 5
1Department of Nursing, Buddhist Tzu Chi General Hospital & Department of Nursing, Tzu Chi University, Hualien, Taiwan
2Department of Health and Social Care, University of Hull, Hull, UK
3Department of Nursing, Buddhist Tzu Chi General Hospital, Hualien, Taiwan
4Institute of Medical Sciences, Tzu Chi University, Hualien, Taiwan
5Department of Nursing, Tzu Chi University of Science and Technology, Hualien, Taiwan
Correspondence to: Yu-Lun Kuo , Department of Nursing, Tzu Chi University of Science and Technology, Hualien, Taiwan.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background. People with pre-diabetes often lack knowledge of their risks of developing diabetes. In one of our previous study, Multi-Approach Health Education was shown evidence to be effective on health behavior of reducing risks of developing diabetes. However, which one approach is really effective and efficient need further investigation. Purpose. To examine the effects of different intervention strategies on diabetes prevention knowledge, exercise, dietary behavior, and physiological indicators for people with pre-diabetes. Methods. This was a randomly controlled trial. People who received health examination and were found fasting blood glucose higher than normal, between 100 - 125 mg/dl in 2011 were recruited. Three types of intervention were randomly assigned to 3 groups respectively. The control group (n=51) received a health education lecture. One experimental group (n=48) received the identical lecture plus telephone encouragement. The second experimental group (n=41) received the identical lecture plus a health reminder poster in their daily life. The outcomes were evaluated for the change in knowledge of diabetes prevention, exercise behavior, dietary behavior, and physiological outcomes at 6 and 12 weeks after the lecture of three groups, respectively. Results. Three intervention strategies were equally efficacious at inducing positive behavioral changes but overall the magnitudes of physiological changes were the same. In general, the maximum change in parameters was achieved after 6 weeks and maintained in the second 6 weeks of the study. Conclusions. Educating people with pre-diabetes about their condition can have a positive effect upon their health behaviors. However, education lecture coupled with a telephone follow up or plus educational posters were found no more effective than lecture alone. The lecture alone of health education may be enough for people with pre-diabetes, but the long term effect needs further investigation.
Keywords: Pre-diabetes, Categories of increased risk for diabetes, Impaired fasting glucose, Diabetes prevention, Health education strategies
Cite this paper: Shu-Chuan Chang , Mark Hayter , Hsiu-Chen Yeh , Tsung-Cheng Hsieh , Yu-Lun Kuo , The Effectiveness of Different Health Education Strategies in People with Pre-diabetes: A Randomized Controlled Trial, Journal of Health Science, Vol. 6 No. 2, 2016, pp. 22-29. doi: 10.5923/j.health.20160602.02.
Article Outline
1. Introduction
1.1. Background
- Diabetes is the fifth leading cause of death among Taiwanese people [1]. Not only does it take the lives of Taiwanese people directly, but also it has a chronic negative influence on the quality of life of those afflicted and caregivers. People with pre-diabetes (after 2010 called “categories of increased risk for diabetes”) are at high risk of developing diabetes. In recent years, the number of people diagnosed with pre-diabetes has increased annually. In the U.S., over 97 million people are considered at pre-diabetic stage and at high risk of developing diabetes [2]. In Taiwan, the investigational study about the incidence of hypertension, hyperglycemia, hyperlipidemia during the period between 2002 and 2007 indicated that, 7.1 out of every 1,000 Taiwanese people will have hyperglycemia [3]. On average, 25,000 people develop new onset hyperglycemia annually with people aged between 40 and 59 being the most rapidly growing demographic [1]. According to the revised standards set by the American Diabetes Association in 2010, pre-diabetes is defined as one of the following conditions: (1) impaired fasting glucose (IFG), with fasting plasma glucose between 100 and 125 mg/dL, (2) impaired glucose tolerance (IGT), with 2-h OGTT plasma glucose between 140 and 199 mg/dL, (3) HbA1C between 5.7% and 6.4% [4]. In comparison to adults with normal blood glucose, the pre-diabetes mortality increases by 40% [5]. Specifically, the probability for developing diabetes and the risks of stroke and kidney diseases are 3, 2.9, and 2.4 times that of the general population in people whose blood glucose exceeds 167 mg/dL two hours after eating. A number of large-scale studies in China, America, Finland and Japan have provided strong empirical evidence that behavioral interventions that include regular exercise, dietary modification and weight control can reduce the risk or delay the development of diabetes [6-9]. As a result, the American Diabetes Association promotes the prevention of diabetes by encouraging active lifestyles, including (1) increased consumption of vegetables, fruit, and whole grains, decreased consumption of fats and oils, (2) regular exercise for at least 30 min per day, and (3) control of ideal body weight [10]. One limitation of this strategy is that people with pre-diabetes who do not know their own condition are unlikely to spontaneously adopt active lifestyles even though they are at risk of developing diabetes. A previous study [11] at a medical center in Eastern Taiwan in 2006 and 2007 found that, at a group health examination, 74% of people who had fasting blood glucose between 100 and 125 mg/dL were unaware that they had pre-diabetic symptoms prior to receiving notification from the hospital. In 2007, the authors of this study implemented a multi-approach health education intervention for preventing diabetes aimed specifically at people with pre-diabetes in eastern Taiwan. This study, randomly assigned the participants to an experimental group (41 people) and a control group (35 people). The experimental group received multi-approach health education intervention that included a diabetes-preventing lecture, a poster, a campaign bowl, and telephone reminders every 2 weeks after returning home. The control group only received ordinary diabetes prevention handout. The intervention period was 6 weeks. The results indicated that this multi-interventional approach health significantly increases exercise behavior, and diabetes prevention knowledge of people with pre-diabetes. In previous study, analysis of the effectiveness of the components of the multi-approach intervention to determine which components were most effective in altering the participant’s behavior were inconclusive. Thirty three percent of the participants believed that the diabetes-preventing lecture had the greatest influence, 21% believed the diabetes-preventing poster, 8% believed the campaign bowl, 13% believed the telephone reminders to be most effective while 25% reported that all four of the interventions were effective [11].Although this study showed the effects of combining strategy of four interventions, it is not possible to determine which of the interventions had the greatest influence on changing diabetes prevention behaviors. Furthermore, studies to date explore the effects of telephone reminders or written educational material for diabetic patients [12], not people with pre-diabetes. Therefore, in this study the inventions were resource and time consuming for the health workers and the goal of our current study was to determine which of the two most influential interventional protocols, the telephone reminders or the written educational material (i.e., diabetes-preventing poster) would be most effective individual intervention in supplementing the positive behavioral effects observed after an educational lecture.
1.2. Aim
- The aim of the study was to assess the effect of different types of health education interventions on the knowledge of diabetes prevention, exercise behavior, dietary behavior, and physiological indicators for people with pre-diabetes.
2. Methods
2.1. Design
- This was a single-blind and randomized study with three intervention protocols. A control lecture only group (LO group), a lecture plus regular three weekly telephone reminders group (LPTR group), and a lecture plus poster group (LPP group). Participants with the enrollment criteria received the “Fasting Blood Glucose Follow-up Notification” and were told there were three different time schedules with the same content of diabetes prevention lecture they could attend. The different types of interventions were randomly assigned to the three groups according to the random table by researcher. Participants did not know the groups to which they would be allocated. The pre-lecture (0 week) evaluation was administered right after the informed consents forms were signed. Participants in each group were evaluated for their knowledge of diabetes prevention, exercise behavior, dietary behavior, body weight, BMI, body fat and fasting blood glucose at the initiation of the study (week 0, pre-lecture) and again at week 6 and week 12 post lecture.
2.2. Participants
- People between 40 and 64 years old with elevated fasting blood glucose level between 100 and 125 mg/dL were included in this study. People who were already diagnosed with type 1 or type 2 diabetes, had a history of psychological illness, or had other serious illnesses (such as liver disease, kidney disease, or cancer) were excluded from this study. Sample size calculation was performed using the G power software version 3.1. To achieve 80% power with a significance level of 5%, the total of 105 participants (35 per group) were required for the study by considering the effect size of 0.3.
2.3. Interventions
- This study employed combinations of three types of interventions, namely, diabetes prevention health education lecture (LO), diabetes prevention health education lecture plus telephone reminders (LPTR) and diabetes prevention health education lecture plus diabetes prevention poster (LPP). Each of the group educational lectures was conducted for 50 min by the researcher with certification of nurse and diabetes educator using presentation. The content of lecture included: the definition of pre-diabetes, reasons for insulin resistance, morbidity of high-risk group, the seriousness of diabetes, and prevention methods. The participants were taught to implement diets that were “low in oil, low in sugar, low in calories, low in sodium, and high in fiber”, and to “perform at least 30 min of medium-intensity regular exercise at least 5 days per week (optimally every day)”. The lecture included information about ideal body weight and blood glucose levels. The lecture was designed to increase a patient’s health consciousness and enhance their motivation to prevent diabetes.The LPTR group received telephone encouragements once every 3 weeks for 12 weeks on the 3rd, 6th, 9th and 12th week after the diabetes prevention health education lecture by the same researcher. Telephone conversations were designed to show concern and encouragement to continue compliance with the intervention behaviors. The LPP group received a diabetes prevention poster, the poster included the following important instructions: (1) do more exercise, (2) eat healthy food, (3) control body weight at the ideal levels, and (4) pay attention to their own blood glucose. The bottom of the poster also provided an exercise record form for participants recording their personal activity time and type daily. Posters were provided after the lecture to the LPP group. The participants in this group were encouraged to place their poster in prominent position in their house, so they could be easily reminded of the health behaviors they must implement after returning home.
2.4. Procedure of Data Collection
- After the study was approved by the Institutional Research Board (IRB) and the research institute, “Fasting Blood Glucose Follow-up Notification” were sent according to people with abnormal fasting blood glucose from the group health checkup in 2008 and 2009 at a medical center in Hualein region of Eastern Taiwan. The notification explained the research aim to encourage them to attend the diabetes prevention health education lecture at a meeting room in the hospital. After the consent forms were signed, the baseline evaluation was administered. All measurements were administered in the same place by the same researcher. The study period was from December 2010 to October 2011.
2.5. Measurements
- The outcome variables of this study were divided into three parts; physiological indicators (fasting blood glucose, body fat, weight, and BMI); diabetes prevention behaviors (exercise and dietary behaviors), and knowledge of diabetes prevention. Fasting blood glucoses were measured using a commercial blood glucose meter (Model ZXD27BDAR, OneTouch UltraEasy, China). Body fat and weight were tested using a commercial body fat monitor (Model BF-700, Tanita, Japan). All testing equipments which were suitable for the qualified, calibrated and maintained.The Diabetes Prevention Knowledge Scale of 8 single choice questions was used to evaluate the diabetes prevention knowledge of the participants. Each correct answer equaled 1 point. An incorrect answer equaled 0 point. Higher total scores represent better knowledge of diabetes prevention. The Cronbach’s α prior to intervention was .64. This scale was a modified version of that developed by Guo et al. (2008) [11].The Exercise Behavior Scale comprised 3 questions of the participant’s “exercise frequency”, “exercise duration”, and “exercise intensity” over the past month. Exercise frequency included four choices, “0 days per week”, “1 to 2 days per week”, “3 to 4 days per week”, and “5 to 7 days per week”. Exercise duration included four choices, “no exercise or less than 10 min”, “more than 10 min but less than 20 min”, “more than 20 min but less than 30 min”, and “more than 30 min”. Finally, exercise intensity included four choices, “never exercise”, “light exercise (participants report feeling relaxed)”, “medium-intensity exercise (participants report some sweating and breathing heavily, but do not feel exhausted)”, “intense exercise (participants report very heavy breathing with a rapid heartbeat and full-body sweating)”. Each question used a 4-point scoring method for calculation, with answers providing 1 point, 2 points, 3 points, and 4 points. The total points were the result of multiplication of the points for the above three questions. The maximum points were 64 and the minimum were 1. Higher total scores represent better exercise behavior among participants. The Cronbach’s α prior to the intervention was .81. This scale was developed by Guo et al. (2008) [11]. The Dietary Behavior Scale comprised 7 questions regarding intake of fat and oils (3 questions), sweets (1 question), vegetables (1 question), grains and cereals (1 question), and low-glycemic index fruits (1 question) to evaluate the dietary habits of the participants over the past month. Every question had four choices, “never consume”, “consume 1 to 2 days per week (occasionally)”, “consume 3 to 4 days per week (often)”, and “consume almost every day”. These questions were scored using the 4-point scoring method. The total score was the result of combining the points for each question. The maximum score was 28 points and the minimum was 7 points. High total scores represent better dietary behavior among the participants. The Cronbach’s α prior to intervention was .53. This scale was a modified version of that developed by Guo et al. (2008) [11]. The demographic variables including gender, age, married status, education level, inhabitance, medical insurance, hyperglycemia history, hyperlipidemia history, obesity history, hypertension history, gestational diabetes mellitus history, diabetes family history were collected at the pre-test by questionnaire.
2.6. Ethical Considerations
- This study was approved by the Institutional Research Board (IRB) and the research institute, Permit number TCRD-9847. All participants were provided detailed explanations of the research purpose and procedures. The informed consents were signed before the participants were enrolled in the study.
2.7. Data Analysis
- The statistical analysis was performed based on intent-to-treat population without the imputation of missing data. The categorical variables were analyzed using the Chi-square test or Fisher’s exact test. With respect to the continuous variables, an ANCOVA model with the independent variables of group, season, and their interaction was used to evaluate the differences among groups adjusted by the effect of season. In addition, a Paired t test was used to analyze the change from 0, 6 and 12 week time points within groups. When p < .05, a statistically significant difference was achieved. All statistical analyses were performed using SPSS 17.0 statistical package software.
3. Results
- In 2008-2009, the Medical center records showed 615 people as having fasting plasma glucose between 100 and 125 mg/dL after routine testing of group health examination. Of the 444 healthy cases with pre-diabetes aged between 40 and 64 contacted, 140 cases agreed to participate in the study which was stopped after the participants completed 12-weeks intervention according to the study design. Among the 140 participants enrolled into the study for the baseline evaluation, 122 people completed the first post-test at week 6 (n: LO group=46, LPTR group=41, LPP group=35; drop-out rate=13%), and 109 people completed the second post-test at week 12 (n: LO group=43, LPTR group=35, LPP group=31; drop-out rate=22%) (Figure 1). Reasons for the drop-out included personal reasons, moving house, lost-to-follow up, and withdrawal from the study. No statistically significant differences were observed in the demographic variables and baseline data of the dropped-out participants among the three groups, also there were no statistically significant differences between them and participants who completed the study.
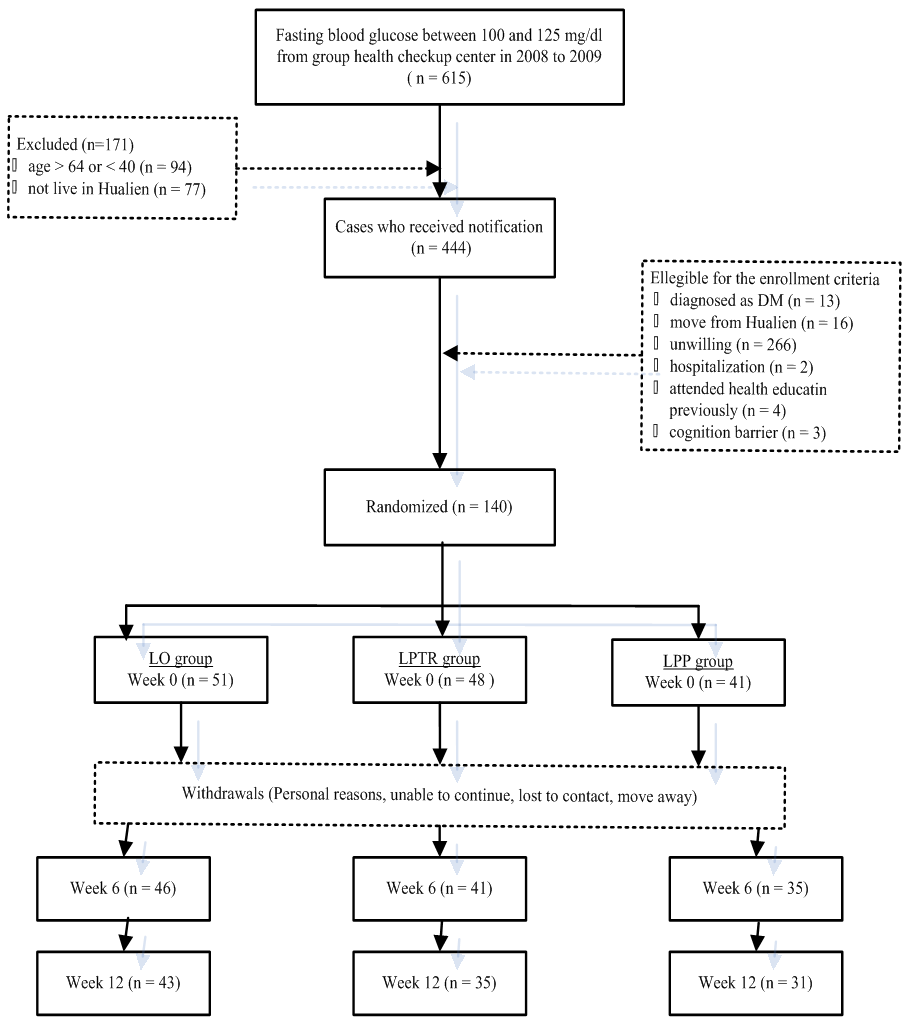 | Figure 1. Flow chart for participants’ enrollment |
3.1. Baseline Data
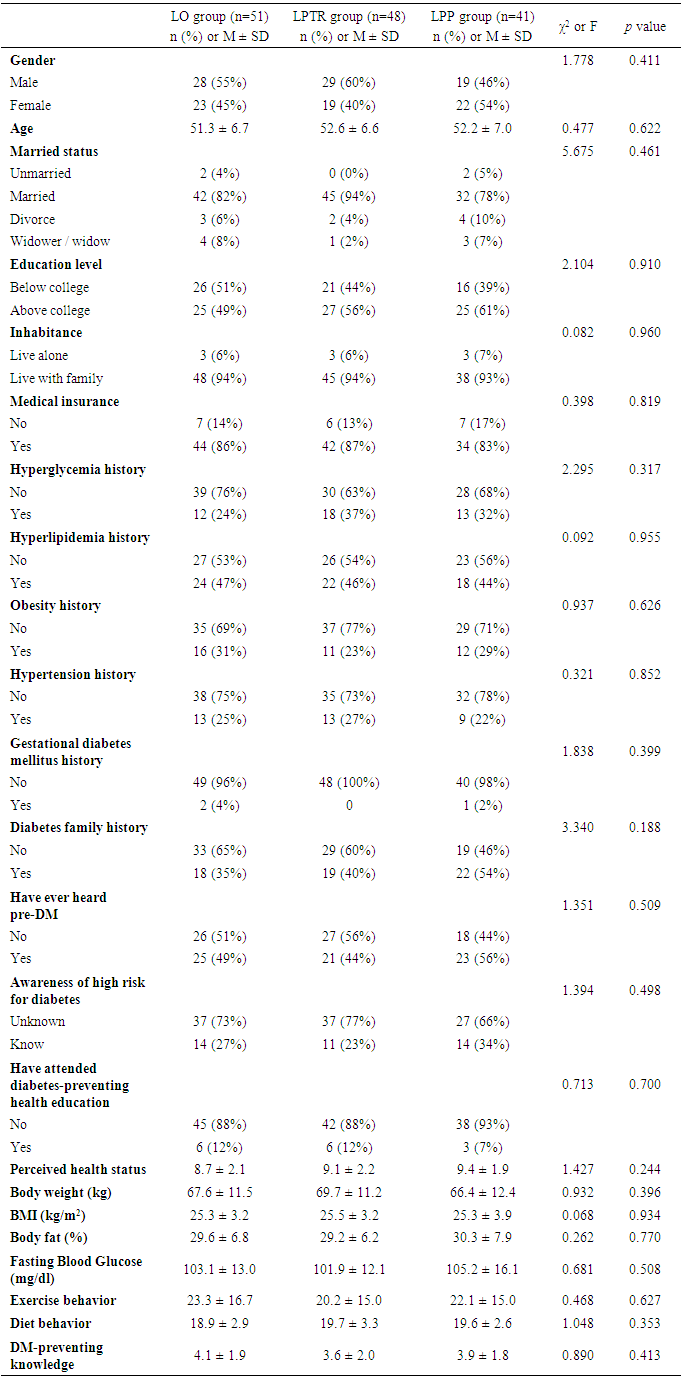
- The average age of participants in each group was between 51 and 53 years old. The proportion of men was between 46 % and 60%, and that of woman between 40% and 54%. Between 78% and 94% of the participants were married. No statistically significant differences among the three groups were observed in the demographic variables and baseline data, including physiological indicators, diabetes prevention behaviors, and knowledge scores (Table 1).
|
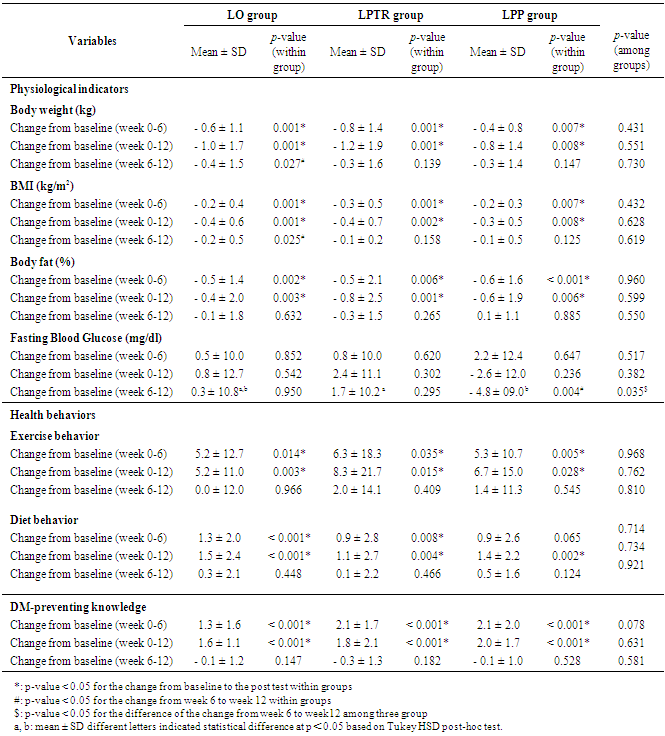
3.2. The Results of the Change from 0 Week to 6 and 12 Weeks within Groups
- Table 2. showed that within each group, relative to 0 week, measurements and scores of the body weight, BMI, body fat, exercise behavior and diabetes prevention knowledge had significantly improved by 6 and 12 weeks of intervention. “Dietary behavior” (p = .065) of the LPP group was the only measure to have failed to reach significance by 6 weeks of intervention but had significantly improved by 12 weeks of intervention. However, no statistically significant improvement was observed in the fasting blood glucose within groups at either 6 and 12 weeks after intervention. Comparison of the changes between 6 and 12 weeks after the intervention indicated that body weight (p = .027) and BMI (p = .025) of the LO group and the fasting blood glucose (p = .004) of the LPP group reached significant difference. However, the other measures did not achieve significant difference. In general, the maximum change in parameters was achieved by 6 weeks and maintained in the second 6 weeks of the study.
|
3.3. The Results of Comparison among Groups after Interventions
- An ANCOVA model was used to analyze the differences of the change from 0 week to 6 and 12 weeks among the three groups. After confirming that no interaction existed between season the participants enrolled and groups, further analysis and comparisons were conducted. Table 2. showed that no significant differences among groups were found for changes in body weight, BMI, body fat, exercise behavior, dietary behavior, or diabetes prevention knowledge at 6 or 12 weeks after interventions from week 0. Of all variables, only fasting blood glucose (p = .035) was significantly different among groups for the change at weeks 12 from weeks 6. The result of post-hoc test showed the effect of LPP group was significant better than the LPTR group (adjusted p= .036) in the improvement of fasting blood glucose.
4. Discussion
4.1. Discussion of Results
- This study demonstrates that over the 12 weeks, each of the intervention strategies of lecture only, lecturer plus 3 weekly telephone reminder and lecture plus written educational poster were equally effective at inducing significant improvements of diabetes prevention knowledge, exercise and dietary behaviors, and modest, yet still significant, changes in body weight, BMI, and body fat. This finding differs from the results of [13], who showed that a single health educational intervention to a group of middle age patients with type 2 diabetes did not improved their blood glucose, body weight or relevant knowledge. The reason for this difference is not known but it could be speculated that the fact that 79% of subjects in the current study were unaware of their pre-diabetic status until enrollment in the study may have had a large positive motivational influence on their behavior to avoid the undesirable label of diabetes. The additional interventions of a 3 weekly telephone reminder or a written educational poster to supplement the educational lecture had no additional stimulatory behavioral or physiological effect on our pre-diabetes cases. We have previously published that telephone reminders once every 2 weeks, and written educational reminder poster as part of a multi-interventional protocol, were in total, effective interventions that altered the behavior and decreased the subsequent risk profile of pre-diabetes cases [11]. Thus telephone reminders and written educational reminder poster per see are not ineffective interventions but rather the lack of effect in the current study probably results because telephone reminders and written educational material were utilize below the intervention threshold required to positively influence behavior of people with pre-diabetes. Thus, if telephone intervention reminders are to be the sole viable intervention, because they are immediate yet resource undemanding on health workers, then a higher frequency than was employed in the current study is essential if the behavior of people with pre-diabetes is to be influenced robustly.The current study clearly shows that informing, previously uniformed people with pre-diabetes about their condition can have a modest but positive effect upon their health behavior. Of the 140 participants who agreed to undertake this study 111 people (79%) were unaware that they were at high-risk of developing diabetes. In addition, 125 people (89%) had never received diabetes prevention health education. These high percentages are consistent with an earlier Taiwanese study [11]. In light of the fact that health education, coupled with motivational encouragement, can reduce the risk of developing diabetes thereby decreasing the medical cost associated with chronic diabetes [14], we suggest that medical agencies in general, and in Taiwan in particular, should place greater emphasis on regularly conducting diabetes screening activities and sending follow-up notifications and educational information to people with fasting blood glucose that exceeds 100 mg/dl. Ideally, the educational information should inspire people with pre-diabetes to perform further oral glucose tolerance test (OGTT) and implement positive lifestyle, such as diet modification, regular exercise, appropriate body weight and monitoring of their own blood glucose level.
4.2. Study Limitations
- Fasting blood glucose was the most unreliable variable measured in this experiment and is known to be strongly influenced by the consumption of different types of foods. The Taiwanese Association of Diabetes Educators suggested in December 2010 that HbA1C be listed as preferred predictive indicator [15]. Therefore, we suggest that future studies include HbA1C testing to determine blood glucose levels. With respect to the measurement of dietary behavior, use of diet diary to record the amount and variety of daily meal should be considered instead of Dietary Behavior Scale for providing more clear information. The diary can present the imperceptible changes in dietary behavior of the participants. The sample size and duration of study period in the present study might also not be enough to provide sound evidence about the effect of planned interventions. Therefore, the larger sample size and longer duration of study period are also suggested in future studies.
4.3. Relevance to Clinical Practice
- Education of pre-diabetes to the positive health consequences of lifestyle changes can have modest beneficial effects upon the behavior of people with pre-diabetes. However, in order for these behavioral changes to be translated into robust improvement in physiologies supplementary reminders for people with pre-diabetes need to be of sufficient frequency and encouragement to surpass their specific activation threshold.
5. Conclusions
- This study assessed the impact of telephone reminders and a written educational poster on diabetes prevention knowledge, dietary and exercise behaviors, and physiological indicators on people with pre-diabetes given a single health education lecture. Relative to pre-lecture measurements, modest, but significant, improvements in every assessed measurement, except fasting blood glucose, were induced by 6 weeks and maintained across the 12 week study. However, supplementary interventions of a three weekly telephone reminders or a written educational poster were no more effective than the educational lecture alone. Supplemental health interventional protocols need to be of sufficiently high frequency so as to encourage and maintain large changes in compliance of people with pre-diabetes. The current study shows that informing, previously uniformed people with pre-diabetes about their condition can have a modest, but positive, effect upon their health behavior. Health intervention protocols that fail to incorporate encouragements above a critical, patient dependent threshold of frequency or motivation may waste health care resources and have no significant influence on the behavior and physiological indicators of people with pre-diabetes.
ACKNOWLEDGEMENTS
- This study was supported by grants from the Buddhist Tzu Chi Medical Center, Hualien, Taiwan (Grant No. TCRD9847).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML