-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2015; 5(4): 76-79
doi:10.5923/j.health.20150504.03
Susac’s Syndrome: Is It Really a Rare Disorder?
Mousa A. Al Mejally1, Hanaa M. Kedah1, Muhammed Fatani2, Lida Amer1
1Neurology department, Hera General Hospital, Makkah, Saudi Arabia
2Dermatology department, Hera General Hospital, Makkah, Saudi Arabia
Correspondence to: Mousa A. Al Mejally, Neurology department, Hera General Hospital, Makkah, Saudi Arabia.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Susac's syndrome consists of the clinical triad of encephalopathy, branch retinal artery occlusion, and sensorineural hearing loss. The pathological mechanism is of unknown origin but is probably autoimmune, thus affecting the capillaries and arterioles of the brain, retina, and cochlea. Here we report the case of a 19-year-old girl who presented to our emergency department with a history of diffuse throbbing headache, confusion, incoherent speech, decreased hearing, and the inability to walk. On examination she was discovered to be encephalopathic with normal fundi and a full range of eye movement, moving all four limbs spontaneously, increased muscle tone all over, and with brisk reflexes. An MRI brain scan showed white matter lesions associated with Susac’s syndrome, and fluorescein retinal angiography and audiogram confirmed the diagnosis. She was treated with intravenous immunoglobulin during acute phase then every 6 weeks for subsequent 6 months along with oral steroids, with remarkable improvement. A four-year follow up period has revealed no further exacerbations to date.
Keywords: Susac's syndrome, Makkah
Cite this paper: Mousa A. Al Mejally, Hanaa M. Kedah, Muhammed Fatani, Lida Amer, Susac’s Syndrome: Is It Really a Rare Disorder?, Journal of Health Science, Vol. 5 No. 4, 2015, pp. 76-79. doi: 10.5923/j.health.20150504.03.
1. Introduction
- Susac’s syndrome is a seemingly rare and arguably, under diagnosed disorder given the diversity and mimickers. Our experience with this patient was good and successful, both during treatment and during the follow-up period. Since then, we have diagnosed another two cases, indicating that Susac’s syndrome is more common than we realized. As such, vigilance is required to ensure accurate diagnosis of the disorder, especially since the existing literature indicates that our case is the first instance of Susac’s syndrome reported from Saudi Arabia.
2. Case Presentation
- Three years ago, an otherwise healthy 19-year-old Saudi girl presented to the ENT with a three-week history of left ear pain, vertigo, nausea, vomiting, and gait instability, with the tendency to veer to her left side. ENT evaluation resulted in a diagnosis of vestibular neuritis, and she was treated with oral antibiotics and oral steroids with minimal improvement. Two weeks later she presented to the emergency department with a diffuse throbbing headache, confusion, incoherent speech, and increased left sided weakness. There was no history of previous febrile illness, trauma, convulsion, mouth or genital ulcers, joint disease, skin rash, or history of recent vaccination. The initial neurological evaluation revealed that she was confused, drowsy, disoriented, and incoherent speech i.e. encephalopathic. She had normal fundi with full range of eye movement. She could move all four limbs but movement on her left side was sluggish, with increased muscle tone all over and brisk reflexes, plantar was upgoing bilaterally. There were no signs of meningeal irritation, and systemic examination was unremarkable.
3. Investigations
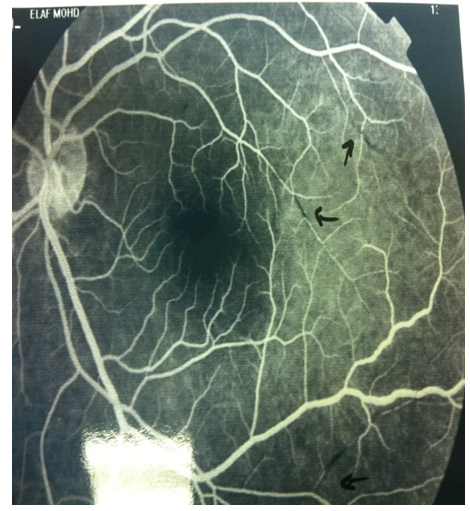
- Her MRI brain scan (Figure 1a) showed multiple white matter lesions in the periventricular region, centrum semiovale, and corpus callosum with minimal meningeal enhancement (Figure 1b). A subsequent MRA brain scan was normal. Cerebrospinal fluid (CSF) analysis showed mild lymphocytic pleocytosis of 19 cells/mm3, and gram stain, acid fast bacilli, latex, and cultures were all normal and the oligoclonal bands were absent in serum and CSF.
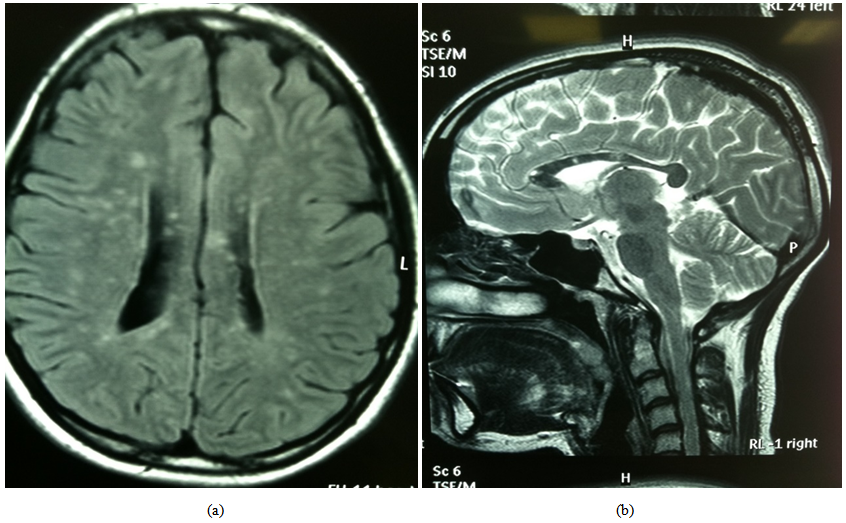 | Figure 1. Patient’s MRI FLAIR and T2 showed multiple high signal rounded leasions in periventricular regions and peculiar “punched out” at mid or central corpus callosum |
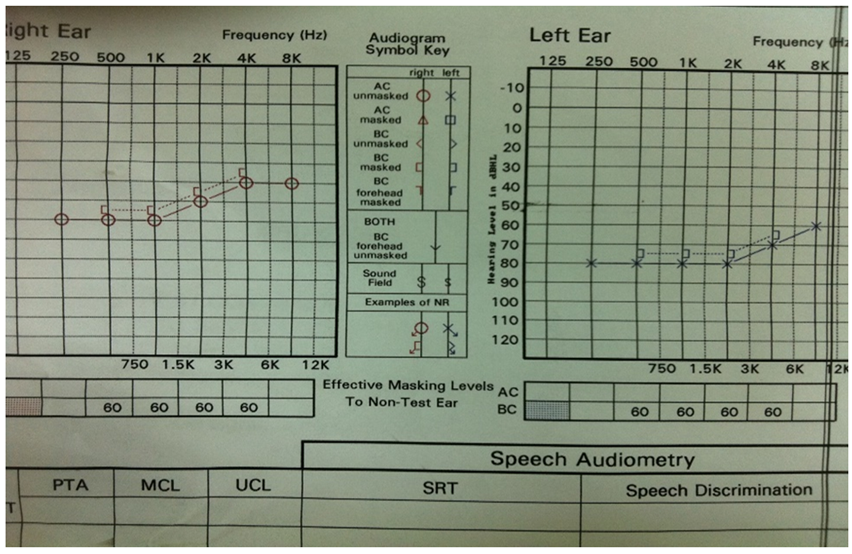 | Figure 2. Patient’s audiogram showing bilateral Sensorineural deafness more over left side |
4. Discussion
- Susac's syndrome consists of the clinical triad of encephalopathy, branch retinal artery occlusion, and sensorineural deafness. The pathogenesis of Susac's syndrome is unknown, yet an autoimmune microangiopathy that targets arterioles under 100 micm in the cochlea, retina, and brain is widely accepted as a potential pathogenesis, [1, 2, 3]. In 1975, John O. Susac reported two women with this syndrome, in 2013 Dorr published a systemic review on 304 cases with Susac syndrome and since then numerous new cases have been reported. However, this is not necessarily due to it being a rare condition, but rather because the disease is unappreciated and understudied. A review of the literature reveals that no cases have been reported from Saudi Arabia and thus our case is probably the first. Susac's syndrome generally affects young women, with a female to male ratio of 3:1. Individuals between the ages of 20 and 40 years are more prone to the disease, although Susac’s syndrome has been diagnosed in a patient as old as 58, [1, 2].The clinical triad may not present together acutely, although may occur at any stage between two weeks and two years or even more from onset. Migraine-like headache is an almost ubiquitous complaint that frequently precedes the onset of encephalopathy and progresses to confusion, cognitive and behavioural changes, and memory and psychogenic disturbances. MRI brain findings in Susac’s syndrome are typically small (1-7 mm), multifocal white matter lesions that frequently enhance during the acute phase (70%). Grey matter is involved in 70% of cases and leptomeningeal enhancement is present in only 33% of cases. Any part of the corpus callosum may be involved (70%), and the central location (snowball) appearance in T2 weighted imaging is characteristic and evolution into pathognomonic T1-hypointensities are typical of Susac’s syndrome and distinguishes it from multiple sclerosis and other demyelinating disorders, [4, 5]. Cerebral angiography is typically normal as the involved arterioles are tiny. The branch retinal artery occlusion is invariably bilateral and difficult to find, and retinal artery or arteriolar branch occlusions with patchy retinal infarcts cause impaired vision, black spots, and scintillating scotoma. The classic findings seen in fluorescein angiopathy are multifocal areas of hypoperfusion in the branch retinal arteries with hyperfluorescence of vessel walls and leakage, [3, 6]. Microinfarcts can also affect the cochlea and semicircular canals, and occluded end arterioles cause sensorineural hearing loss with lower tones being affected initially on audiometry. Hearing loss is usually bilateral and at variable degrees in each side. Tinnitus, vertigo, and gait instability are common at onset, [7]. Aggressive immunotherapy such as intravenous immunoglobulin and intravenous methylprednisolone in the acute phase is warranted to achieve rapid remission, and cyclophosphamide and cyclosporine are among other options. Scheduled intravenous immunoglobulin for several months may be useful to prevent relapse in the short period after the acute phase, whereas oral prednisolone, mycophenolate mofetil, and aspirin should be used to attain prolonged remission. The duration of therapy continues to be a dilemma and is dependent on the long duration of patient follow up, [8, 9].
5. Conclusions
- Susac's syndrome is a microangiopathy of unknown origin, probably autoimmune, affecting the capillaries and arterioles of the brain, retina, and cochlea. Diagnosis is made by identifying the characteristic MRI pattern, especially those in the central corpus callosum accompanied by the partial or complete clinical triad of encephalopathy, visual, and hearing problems, and fundus or retinal fluorescence angiographic findings of branch retinal artery/arteriolar occlusions. Aggressive immunotherapy is required to attain remission in the acute phase of the disease, and we suggest the combined use of intravenous methylprednisolone and immunoglobulin to achieve sustained remission, along with the use of scheduled intravenous immunoglobulin for the six months following the acute phase.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML