-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2015; 5(1): 11-17
doi:10.5923/j.health.20150501.03
The Role of Lifestyle in Reducing Stroke Morbidity and Mortality in Acute Stroke Patients Treated at Adam Malik Hospital of Medan, Indonesia
Fazidah A Siregar 1, Tri Makmur 2, Nurul Huda 3
1Faculty of Public Health, University of Sumatera Utara, Medan, North Sumatera, Indonesia
2Faculty of Medicine, Islamic University of Sumatera Utara, Medan, North Sumatera, Indonesia
3Food Technology Program, Universiti Sains Malaysia, Penang, Malaysia
Correspondence to: Fazidah A Siregar , Faculty of Public Health, University of Sumatera Utara, Medan, North Sumatera, Indonesia.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Strokes are common, and lifestyle contributes to this high incidence. To reduce the incidence of stroke, it is necessary to identify and understand the role of lifestyle in the occurrence of this disease. A hospital-based case control study was conducted. The cases and controls studied consisted of 55 hospitalized patients with stroke (confirmed by computed tomography scan) and 55 unmatched-age and sex controls that were hospitalized at the study hospital for condition other than stroke. Socio-demographic characteristics, medical information and lifestyle risk factors were collected from the cases and the controls by interview and recorded using questionnaire. Data analysis using SPSS release 20.0 and epi info release 6. Cross tabulation was used to select the significant variables and followed by trend and stratification analysis. The multivariate logistic regression used to determine the lifestyle predictors of stroke. The results revealed that age, smoking and a history of hypertension are all independent of each other in their risk for stroke. Hypertensive patients were found to have an 808.9-fold increase in the risk of stroke (OR: 808.9; 95% CI: 35.78-1824.7) when compared to non-hypertensive patients. The smoking of ≥21 cigarettes/day was found to result in a 64.09-fold increase in the risk of stroke (OR: 64.09; 95% CI: 2.07-198.1) compared to those who never smoked. These results indicate that hypertension was the greatest risk factor for stroke. Regular treatment for control hypertension and cessation of cigarette smoking through changes in lifestyle might contribute to a reduction in the incidence of stroke.
Keywords: Lifestyle, Stroke, Case control study
Cite this paper: Fazidah A Siregar , Tri Makmur , Nurul Huda , The Role of Lifestyle in Reducing Stroke Morbidity and Mortality in Acute Stroke Patients Treated at Adam Malik Hospital of Medan, Indonesia, Journal of Health Science, Vol. 5 No. 1, 2015, pp. 11-17. doi: 10.5923/j.health.20150501.03.
1. Introduction
- Stroke is one of the most common health problems and is a leading cause of morbidity and mortality worldwide. Approximately 20 million people each year will suffer from stroke, and 5 million of these will not survive [1]. Stroke is the second leading cause of death worldwide [2, 3]. In 2005, stroke accounted for 5.7 million deaths worldwide, with 87% of the deaths occurring in developing countries [4]. Stroke can cause disability and approximately 20% of stroke patients require institutional care after 3 months, and 15-30% experience permanent disability [5]. The result of Basic Health Research 2008 conducted in Indonesia showed that stroke is a major cause of death in Indonesia after tuberculosis and hypertension [6]. Indonesia’s recent data show there is an increasing trend in the incidence of stroke, death and disability [7]. The increased stroke risk in the community is related to a combination of an aging population physical change, environment, habits, and lifestyle that predispose the population to stroke [8].Data from Adam Malik Hospital showed that stroke is the most common disease in the neurology ward. In 2000, there were 243 patients treated in the neurology ward, and 65.5% were acute stroke patients, with a mortality of 16.05% [9]. While in 2011 the number of stroke patients treated at Adam Malik Hospital increased to 390 patients and 72% are ischemic stroke [10].Stroke is a multifactorial condition. A number of risk factors have been shown to be associated with stroke, including age, sex, heredity, hypertension, diabetes, hypercholesterolemia, dietary factors, obesity, smoking, alcohol intake, and physical inactivity [5, 11, 12]. However, the contribution of each risk factor to the outcome of stroke varies from one study to another. Risk factors for stroke were classified according to potential for modification (nonmodifiable and modifiable risk factors). Nonmodifiable risk factors include age, sex, race/ethnicity and genetic. Modifiable risk factors include, hypertension, diabetes, exposure to cigarette smoke, obesity, physical inactivity, alcohol consumption and poor diet. The various of risk factors for stroke are established and should be placed in identifying modifiable risk factor in achieving effective prevention strategies [13]. Many studies have revealed a relationship between lifestyle factors and stroke; however, the exact role of lifestyle factors in stroke risk is uncertain. Hypertension is the most important risk factor for stroke. Hypertension plays a role in arterial occlusion, embolic stroke and the rupture of cerebral aneurysms, which cause intracerebral hemorrhage [11]. Several studies have shown that blood pressure is closely associated with damage to both cardiovascular and cerebrovascular organ [12] and stroke events is related to a morning surge in blood pressure [14]. Current smoking has been identified as a risk factor in several studies [15-21]. The chemical ingredients in cigarettes accelerate the process of atherosclerosis and make it more difficult for blood to move through the vessels, which can increase blood pressure. There is a dose-response relationship in which heavy smokers are at higher risk for stroke than are light smokers. The consumption of high-energy food with excessive fat intake and low fiber and micronutrient intake will predispose people to stroke risk by increasing blood cholesterol and obesity. High cholesterol contributes to the formation of atheroma and leads to atherosclerosis [11]. A cohort study by Albala et al, the Northern Manhattan study of 3,183 stroke-free community residents over 40 years of age between 1993 and 2001, found that total fat intake above 65 g/day significantly increased the risk of stroke [22]. A population case control study by Jamrozik et al of 501 cases and 931 controls in Perth, Western Australia, from 1989 to 1990 found that the consumption of meat more than four times weekly was associated with an increased risk of stroke [21]. Similarly, a study by Fung in Boston of 791 cases of stroke between 1984 and 1998 found that a high intake of red and processed meats may increase the risk of stroke (RR: 1.58; 95% CI: 1.15 to 2.15) [23]. The role of alcohol consumption is still controversial. A study of 694 stroke patients by Hiroyasu et al in Japan from 1990 to 2001 found that light to moderate alcohol consumption might reduce stroke risk, whereas heavy drinking caused a 1.5- to 2.0-fold increased risk of stroke [24]. However, these findings are not consistent with those of Djousee et al, whose population-based case cohort study on 5,209 subjects in Framingham found that total alcohol intake was not associated with a risk of ischemic stroke and had protective effects among subjects 60 to 69 years old [25]. Regular physical activity 3 to 5 days per week with intensity for 20 to 40 minutes is an important component of primary prevention against stroke in the elderly [26] and can be expected to reduce the risk of stroke. Several studies have examined the association between exercise and stroke occurrence [11, 26]. The Northern Manhattan Stroke study found that moderate- to heavy-intensity physical activity is a protective factor against the risk of ischemic stroke [26]. Stroke is an important health problem among the elderly. Many attempts had conducted but the incidence of stroke is still high. The efforts to reduce the incidence of stroke should be based on risk factors that may influence, in particular, risk factors related to lifestyle. Therefore, identifying and understanding the lifestyle risk factors may contribute to the reduction in stroke morbidity and mortality. Therefore, a study to identify the lifestyle risk factors in acute stroke patients were treated at Adam Malik Hospital of Medan was undertaken to help health organization to enhance intervention to public in reducing stroke morbidity and mortality, specifically in Adam Malik Hospital of Medan, Indonesia.
2. Methods
- Study Design and Population: The present study was carried out at Adam Malik hospital (Medan, North Sumatera) from September 2001 to January 2002. The study was designed as age-and sex-unmatched hospital case control study. Cases: The study consisted of 55 hospitalized patients with stroke and confirmed by computed tomography (CT) scan. The cases recruited for this study were new patients who were experiencing for the first time the specific symptoms and neurological signs of stroke and then confirmed with head CT scan. The patients were conscious and expressed a willingness to participate in this study.Controls: The controls were selected from among patients who were treated at the study hospital for conditions other than stroke. For each case of stroke, one control was selected. The controls were unmatched to cases with respect to age and sex, and fifty-five controls were selected in the same manner. Sample Size: Two proportion formulas were used to determine the sample size. We used an average odds ratio (OR) of 3.0, a hypertension prevalence of 70% [27], and an allowable error of 5%, and for a power study of 80%, the calculated sample size was 55 [28, 29]. Therefore, a total of 55 cases and 55 controls were included in this study. Study Instruments: Socio-demographic data, medical information and lifestyle variables were collected by interview and recorded using a semi-structured questionnaire. Information on each of the patients lifestyle was collected including smoking, alcohol consumption, fat and calories intake and physical activity. Risk factors: Nine risk factors namely age, hypertension, diabetes mellitus, smoking, overweight, fat intake, calories intake, smoking, alcohol consumption and physical activity were identified. The history of hypertension was used in the present analysis and was defined as having a diastolic blood pressure above 90 mmHg. Diabetes was defined as having a random blood sugar in excess of 200 mg%. Overweight status was determined by the body mass index obtained by measuring the weight and the height. Overweight was identified if the body mass index exceeded 25.1. Measurements of fat and caloric intake were taken based on 2 x 24 hour food recall [30]. Participants were asked how often each food was eaten and the portion size. The total fat and caloric intake was calculated by summing the fat and caloric intakes from all foods and then comparing the result to the recommended dietary allowance (RDA). High caloric intake was identified if the intake of calories exceeded 120% RDA, and a high fat intake was identified if the fat intake exceeded 30% of total calories. Data on smoking were used to classify subjects as nonsmokers, smokers of 1-10 cigarettes daily, smokers of 11-20 cigarettes daily, or smokers of 21 or more cigarettes daily. Consumption of alcohol was assessed by asking how often drinking occurred during a week and was classified as never, once per week, 2-7 times per week, or more than 7 times per week. Participants were asked how often they engaged in physical activity in one week, and this was classified as less than 3 times per week, 3-5 times per week, or more than 5 times per week. Statistical Analysis: The Statistical Package for the social science (SPSS) package program (Release 20.0, SPSS inc. Chicago, Illinois, USA) and epi info (Release 6, CDC, Atlanta) were used for statistical analysis. Cross-tabulation analysis was performed using epi info 6 to select variables with p- values less than 0.05, and followed by trend analysis and stratification using the Mantel Haenszel test. The significant variables with p- values less than 0.05 were put in the multivariate logistic regression model for further investigation, which was performed using the SPSS program and with backward stepwise methods.
3. Result
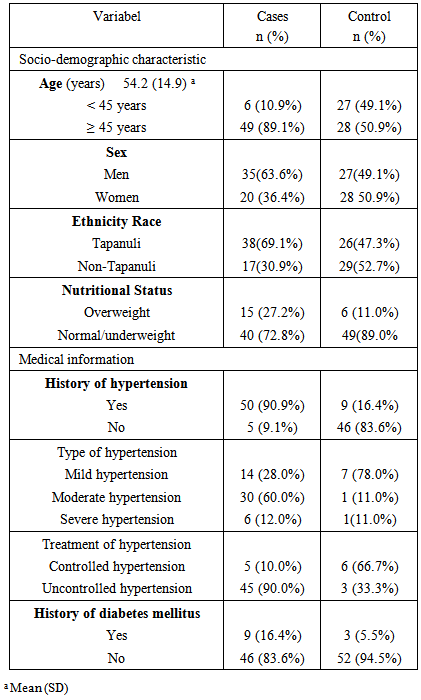
- The mean age of the study population was 54.2 ± 14.9 years (range: 20-91 years). Majority of cases (89.1%) were ≥ 45 year age group, 63.6% were men and 69.1% were residents of Tapanuli. Based on nutritional status, most of the case and control patients were normal or underweight (72.8% vs. 89.0%, respectively). The majority of cases (90.9%) had a history of hypertension with moderate hypertension (60%) and commonly uncontrolled hypertension (90%). Most of the patients in both the cases and control groups did not have history of diabetes mellitus. The details are listed in Table 1.
|
|
|
|
|
|
|
4. Discussion
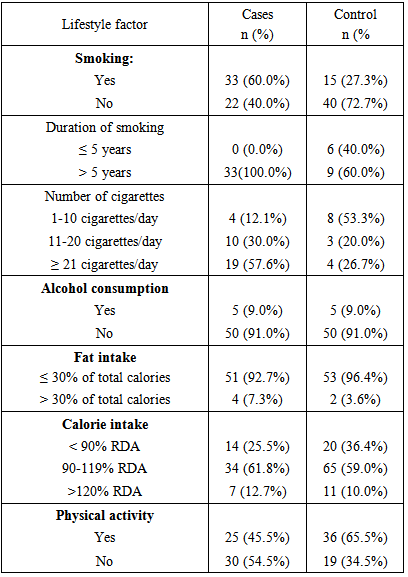
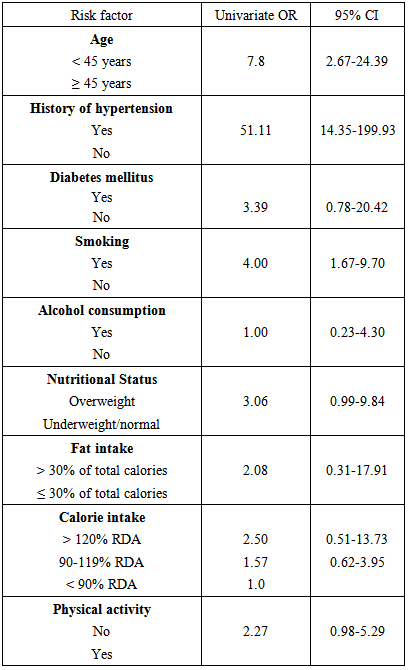
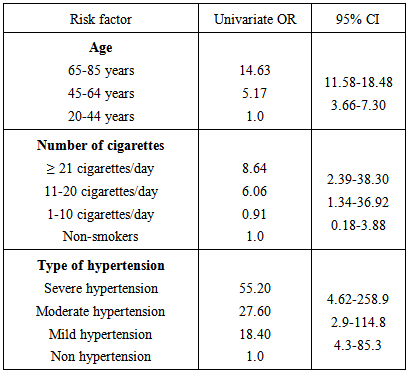
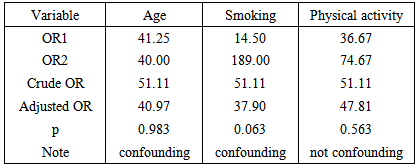
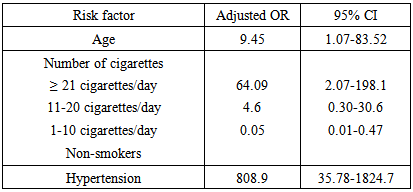
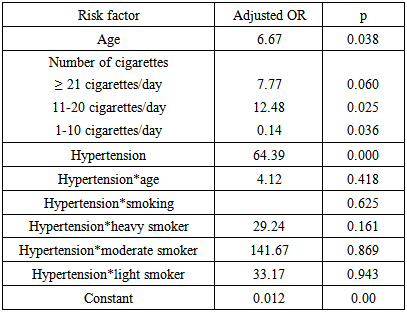
- This is a study that quantifies the contribution of different factors to the risk of stroke. It was found that age, cigarette smoking and history of hypertension are all independent of each other in their risk for stroke. Cigarette smoking and hypertension are modifiable risk factors. In the present study found that hypertension was the greatest risk factor for stroke. Hypertension is well known as the most important risk factor for stroke, both high systolic and diastolic blood pressure [12, 31]. In the cross-tabulation found patients with hypertension had a 51.11-fold increased risk of stroke compared to those without hypertension. In trend analysis there is a sequence risk of stroke according to severity of hypertension. Mild hypertension had a 18.40-fold risk of stroke, increased to 27.60-fold in the moderate hypertension and 55.20-fold in the severe hypertension compared to non hypertension. This findings is consistent with Turan study et al found that the higher blood pressure is associated with increase risk of ischemic stroke and stroke in the territory of the stenotic vessel [32]. In the multivariate analysis, after adjustment, it was found that hypertension plays a role in the occurrence of stroke. Patients with hypertension had an 808.9-fold increased risk of stroke compared to those without hypertension. The interaction analysis found no interaction between hypertension and age and smoking relative to the relationship between hypertension and stroke incidence. It mean that history of hypertension is independent variable relative to the incidence of stroke. We know that hypertension is a modifiable risk factor for stroke. Uncontrolled hypertension in Indonesia was found to be 95.9% and proved to be a dominant risk factor for stroke [33]. In the present study, 90% of stroke patients had history of hypertension with uncontrolled hypertension. Cairu Li study et al on 27,936 subjects in 45-73 years old in Sweden and follow up for 6 years found that more than 90 % of stroke occurred in those with uncontrolled blood pressure [34]. While as we know that adequate control of blood pressure is a cornerstone in stroke prevention and enormous public health importance. Thus control hypertension is important and could reduce the incidence of stroke.This study demonstrated an independent dose-response relationship between cigarette smoking and the risk of stroke. Among the various lifestyle factors in this study, smoking was an important risk factor for the incidence of stroke. In this study, the majority of cases (60.0%) reported smoking, with all reporting a duration of more than 5 years and partially reporting smoking ≥ 21 cigarettes/day. Our univariate analysis demonstrated an association between smoking cigarettes and occurrence of stroke. These results are consistent with the Framingham study, which found that smokers had a 1.6-fold risk of stroke compared to non-smokers [12]. Similarly, Jamrozik et al found that smokers had a 3.5-fold risk of stroke compared to non-smokers [21]. The trend analysis showed a sequence of stroke risk that was dependent on the number of cigarettes smoked per day. The smoking of ≥ 21 cigarettes/day resulted in an 8.64-fold increased risk of stroke, and the risk was 6.06-fold increased for those smoking 11-20 cigarettes/day, compared to non-smokers. This finding is consistent with Kelly et al, who found that in the Chinese adult population, there was a dose-response relationship between cigarette smoking and the risk of stroke. Smoking 10-19 cigarettes/day resulted in a 1.20-fold increased risk of stroke, which increased to 1.42-fold for smoking ≥ 20 cigarettes/day, compared to non-smokers [16]. Similarly, in the U.S. Physicians’ Health Study, Kurth and colleagues found smoking < 20 cigarettes/day resulted in a 1.6-fold increased risk of stroke, which increased to 2.25-fold for smoking ≥ 20 cigarettes/day [17]. In the stratification analysis, we found smoking to be a confounding factor in the relationship between hypertension and stroke. The multivariate analysis after adjustment found that smoking influenced the incidence of stroke and showed a tendency toward a higher risk of stroke based on the number of cigarettes smoked per day. The interaction analysis found no interaction between smoking and hypertension in the relationship between hypertension and stroke. Thus smoking is independent variable relative to the incidence of stroke. The smoking of ≥ 21 cigarettes/day resulted in a 64.09-fold increased risk of stroke compared to non-smokers. This finding indicates that the impact of smoking on the risk of stroke is important. Smoking is associated with the occurrence of stroke through the mechanisms of inhibiting the release of prostacyclin and causing platelet adhesion [11, 17, 21]. The chemical ingredients in cigarettes accelerate the process of atherosclerosis and can increase blood pressure. Programs supporting the prevention and cessation of smoking could be part of a strategy to reduce the incidence of stroke.In this study, lifestyle factors such as alcohol consumption, fat and calorie intake, and physical activity did not appear to play a role in the occurrence of stroke. This finding might be because most of the cases and controls had no alcohol consumption, had fat intake ≤ 30% of total calories, and had a caloric intake of 90-119% RDA. In addition, for physical activity, there was no significant difference in stroke occurrence between cases with and without physical activity. Our data revealed no association between these variables and the occurrence of stroke, suggesting that these variables are not significant. Age is an important risk factor for stroke, mostly in those aged > 45 years, and the risk increases with age [11]. The present study demonstrated that there was a sequence of stroke risk that increased with age. In the group aged 45-65 years, there was a 5.17-fold increased risk of stroke, which increased to 14.63-fold in the group aged 65-85 years, compared to the group aged less than 45 years. These results are consistent with the Framingham study, which found that the incidence of stroke increased with increasing age from 22% for ages 45-55 years to 83% for ages 65-74 years [12]. In Rochester, Minnesota, the incidence of stroke increased 10% for each year of age [11]. Stratifying by age found that age is a confounding variable and that there is no interaction between age and hypertension relative to the occurrence of stroke. This finding is supported by the multivariate analysis, which found that age influences the incidence of stroke. The interaction analysis revealed no interaction between age and hypertension in the occurrence of stroke.
5. Conclusions
- Our study revealed that hypertension and cigarette smoking are important modifiable risk factors for stroke. Hyperten-sion was the greatest risk factor for stroke and followed by cigarette smoking. There is a dose-response relationship between cigarette smoking and the risk of stroke. Targeted intervention mainly reduce blood pressure by control of blood pressure and regular treatment and cessation smoking through change in lifestyle could substantially reduce the morbidity and mortality of stroke in the community. Therefore, in reducing stroke morbidity and mortality in community promote anti smoking programs and control of blood pressure should be enhanced.
ACKNOWLEDGEMENTS
- We gratefully acknowledge Prof Darulkutni Nasution, Head of the Department of Neurology, for his facilitation of and advice on this study; everyone in the Neurology Department who was involved in this study; and all study participants.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML