-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2014; 4(3): 72-78
doi:10.5923/j.health.20140403.04
Utilisation of Modern Contraceptive among Women of Childbearing Age in Resource Constraint Setting: Evidence from 2008 National Demographic and Health Survey in Nigeria
Franklin C. Igbodekwe1, Olanrewaju Oladimeji2, 3, Kelechi E. Oladimeji1, 4, Ikeola A. Adeoye1, Onoja M Akpa1, Lovett Lawson2
1Department of Epidemiology and Medical Statistics, Faculty of Public Health, College of Medicine, University of Ibadan, Oyo State, 200211, Nigeria
2Tuberculosis Research Unit, Zankli Medical Centre, Abuja, 900108, Nigeria
3Liverpool School of Tropical Medicine, Pembroke Place, Liverpool L3 5QA, United Kingdom
4Research Unit, Institute of Human Virology Nigeria, Abuja, 900211 Nigeria
Correspondence to: Franklin C. Igbodekwe, Department of Epidemiology and Medical Statistics, Faculty of Public Health, College of Medicine, University of Ibadan, Oyo State, 200211, Nigeria.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
BackgroundNigerian women are known to have high fertility rates and a low utilization of modern contraceptives. Understanding the factors affecting the use of contraceptives using a nationally representative data is crucial to tackling the low prevalence of contraceptive use in Nigeria.Methods: Secondary dataset of 33,385 women aged 15-49 years, who participated in the 2008 National Demographic and Health Survey was analysed. We calculated contraceptive prevalence rates for various population sub-groups, and examined the association between socio-demographic characteristics and current modern contraceptive use, using multiple logistic regressions.Results: Mean age of the respondents was 31.1±8.8 years. Current contraceptive prevalence rate was 13.2%, while that of modern methods was 9.4%. The significant factors associated with the utilization of contraceptives were urban residence (OR=1.22, 95%CI=1.11-1.35), being a working class woman (OR=1.22, 95%CI=1.11-1.35), being educated (OR=1.22, 95%CI=1.11-1.35), parity (OR=1.22, 95%CI=1.11-1.35), being wealthy (OR=2.62, 95%CI=2.14-3.21). Importantly, the likelihood utilization varied across the gradient of wealth. Women in richest (OR=2.62, 95%CI=2.14-3.21), richer (OR=2.44, 95%CI=2 .02-2.94), and middle (OR=1.78, 95%CI=1.48-2.14) wealth quintiles were more likely to use modern method compared to women in the poorest category.Conclusions: Prevalence rates were very low across virtually all segments of the population. Concerted efforts are required to increase use of modern methods of contraception.
Keywords: Contraceptive use, Women, Childbearing age, Nigeria
Cite this paper: Franklin C. Igbodekwe, Olanrewaju Oladimeji, Kelechi E. Oladimeji, Ikeola A. Adeoye, Onoja M Akpa, Lovett Lawson, Utilisation of Modern Contraceptive among Women of Childbearing Age in Resource Constraint Setting: Evidence from 2008 National Demographic and Health Survey in Nigeria, Journal of Health Science, Vol. 4 No. 3, 2014, pp. 72-78. doi: 10.5923/j.health.20140403.04.
Article Outline
1. Introduction
- Nigeria has remained the most populous country in the Africa with a total population of about 160 million at the 2006 census. The current total fertility rate is estimated to be 5.7 per woman. Low utilization of modern contraceptive is one of the key determinants of high fertility in Nigeria [1-3]. Modern contraceptives which include hormonal and non-hormonal methods are preferred above the traditional methods like periodic abstinence and coitus interuptus because they are more efficacious and are associated with lower failure rates. The correlates of low contraceptive use include high rates of unwanted pregnancies, abortions, maternal and perinatal morbidity and mortality. The utilization of modern contraceptives is an important component of maternal, new-born, and child health services [1]. It plays a significant role in fertility reduction by facilitating both the spacing and limiting of pregnancies in women of reproductive age [2]. Importantly, limiting pregnancy in women of reproductive age is vital to the reduction of the risk of maternal and prenatal complications from early childbearing, thereby resulting in decrease in infant, child and maternal mortality [2, 3]. Evidence shows that the high level of awareness and knowledge of contraceptive methods in Nigeria. For example about 70% of the women know of at least a method of contraception [4]. However, modern contraceptives in Nigeria therefore the contraceptive prevalence rate has remained low [5, 6]. Ample evidence from the literature shows that low contraceptive prevalence rates is associated with high maternal mortality ratios [7, 8], and Nigeria records one of the highest ratio, with maternal mortality ratio of 545 deaths per 100,000 live births [4]. Several factors play an important role in the use of contraceptives among women of childbearing age [9, 10]. The identification of these factors is crucial to the planning and implementation of suitable family planning programmes [2, 9-12]. While studies on factors affecting the use of contraception among women have been reported for selected areas in Nigeria [11, 12], in-depth analysis of factors affecting the use of modern contraception among women of childbearing age in a national survey has been scarcely reported in Nigeria. The purpose of this study is to determine the prevalence of contraceptive use in Nigeria, and to examine the factors that affect contraceptive use in a nationally representative survey.
2. Methods
2.1. Study Design
- The study design was a retrospective cross-sectional study. The data were extracted from the National Demographic and Health Survey (NDHS) of 2008 conducted by Inner city fund (ICF) Macro Calverton, Maryland, U.S.A. in conjunction with National Population Commission (NPC), Nigeria. During the survey, a multi-stage probability sampling was adopted to select 33,385 women age 15-49 [4].
2.2. Study Area
- Nigeria is made up of 36 states and Federal capital territory (FCT), Abuja. It is the most populous country in Africa, with a population of more than 162 million people [13]. The country is made up of diverse ethnic and cultural groups, with a low literacy level.
2.3. Sampling Method
- The sample for the 2008 NDHS was designed to provide population and health indicators across the country. The Population and Housing Census of the Federal Republic of Nigeria in 2006, and was provided by the National Population Commission (NPC). During the 2006 population census, each locality was subdivided into convenient areas known as enumeration areas (EAs), in addition to the administrative units of the Federal Republic of Nigeria namely; states, local government areas (LGA), and localities. The primary sampling unit (PSU), referred to as a cluster for the 2008 NDHS, is defined on the basis of EAs from the 2006 EA census frame [4]. The 2008 NDHS sample was selected using a stratified two-stage cluster design consisting of 888 clusters, 286 in the urban and 602 in the rural areas. A representative sample of 36,800 households was selected with a minimum target of 950 completed interviews per state. In each state, the number of households was distributed proportionately among its urban and rural areas. A complete listing of households and a mapping exercise were carried out for each cluster from April to May 2008, with the resulting lists of households serving as the sampling frame for the selection of households in the second stage. All private households were listed. The final survey sample came down to 886 instead of 888 clusters because of inaccessibility to the cluster due to flooding and inter-communal unrest during fieldwork [4].
2.4. Data Management
- The female dataset (NGIR51FL.SAV) – SPSS file format used in this study was obtained from ORC Macro. In the original questionnaire used for the survey, a question was asked from the respondents on any methods used for contraception. Current use of modern contraceptive method was used as a dependent variable, while the independent variables include age, marital status, occupation, place of residence, region (zone), level of education, religion, ethnicity, wealth index and parity.
2.5. Data Analysis
- Frequency tables were generated to describe and summarize variables of interest. Further analyses were performed using Chi-square and multiple logistic regression analysis to investigate association between the dependent and independent variables. The logistic regression model is of the form;
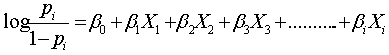 Where;
Where;  is the proportion of women of child bearing age in Nigeria who were currently using modern contraceptives.
is the proportion of women of child bearing age in Nigeria who were currently using modern contraceptives. are parameters to be estimated and
are parameters to be estimated and  are the independent variables.All statistical analyses were performed at 5% level of significance using the Statistical Package for Social Sciences (SPSS) version 15.
are the independent variables.All statistical analyses were performed at 5% level of significance using the Statistical Package for Social Sciences (SPSS) version 15.3. Results
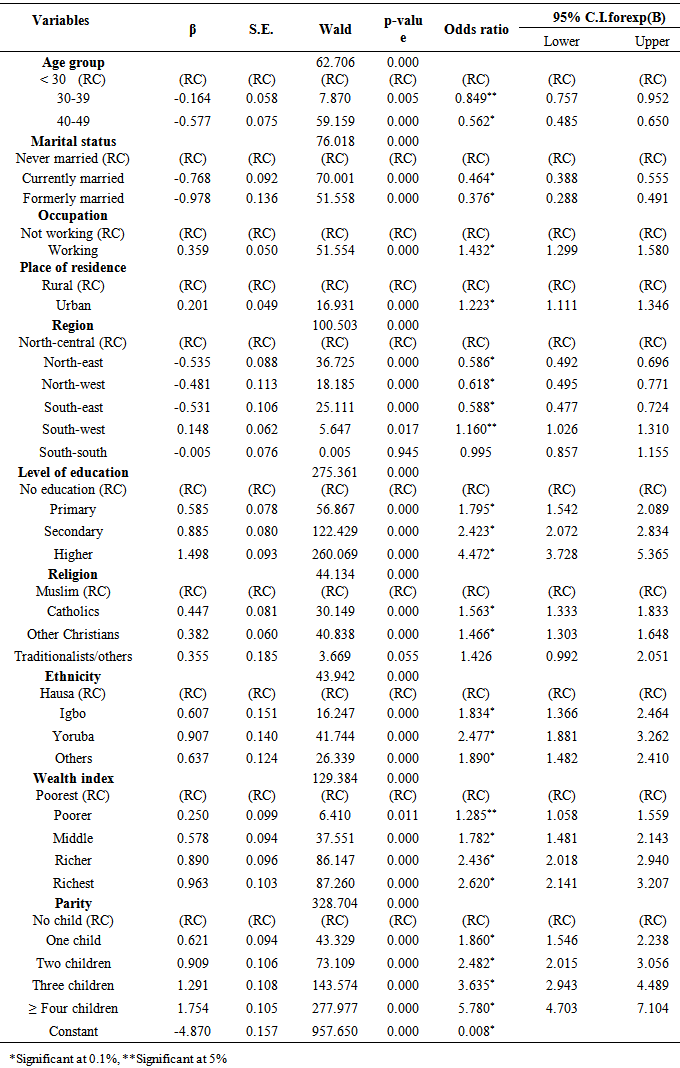
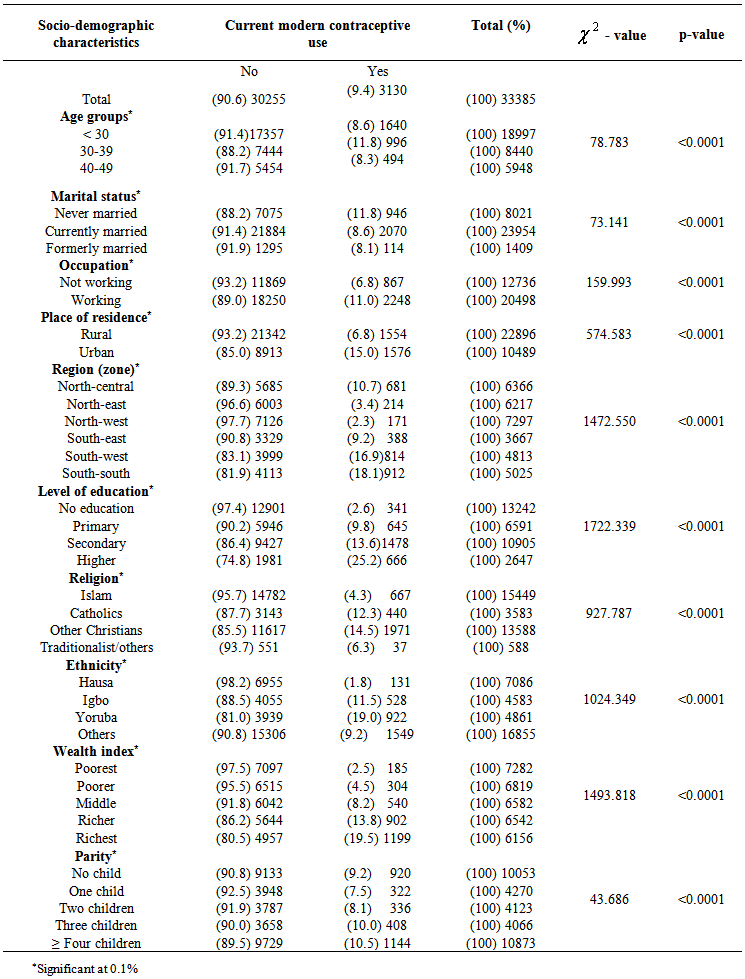
- Table 1 shows variation in the prevalence of current modern contraceptive use over various demographic characteristics of the women aged 15-49 years. The data shows that the prevalence of modern methods was 9.4%. Twelve percent of those who use modern contraceptives belonged to the age group 30-39 years, while the lowest prevalence was among the respondents between 40 and 49 years (p<0.1). (Table 1). Respondents that were never married were significantly likely to use modern contraceptive methods than those currently married or formerly married (p<0.01). Women with employment were more likely to use contraception compared to those unemployed (P<0.01) and are more likely to live in urban setting (p<0.01). (Table 1). Respondents in South-south and south-west regions were significantly likely to use modern contraceptive when compared to their contemporaries in the other zones (p<0.01). A larger number of the respondents who had tertiary education were more likely to use modern contraceptive method compared to those with lower grades of education (p<0.01). Christians were more likely to utilise modern contraceptive than Muslims and Traditionalists. When compared, other Christian denominations were more likely to use contraceptives than the catholic. Statistically, Yoruba respondents were more likely to use modern contraception than other ethnics group in the country (p<0.01), while the highest use was found among the richest wealth quintile (p<0.01). Multi-parity respondents were more likely to prevent more pregnancy by use of modern contraception (p<0.01).
 | Table 1. Socio-demographic characteristics of women of child bearing age with respect to use of modern contraceptive |
|
4. Discussion
- Our study assessed modern contraceptive use and its correlates among Nigerian women of childbearing age (15-49 years) using the 2008 NDHS data. Specifically, the study examined the prevalence of current contraceptive method used by Nigerian women, and the factors that might influence their use across the six geopolitical zones of the country. It also identified socioeconomic factors, as well as maternal factors that influenced modern contraceptive use among Nigerian women. The overall rates for current contraceptive use was 13.2%, while the rate for modern methods was 9.4%. These are slight improvements over previous nationally representative CPR estimates. Specifically, the CPR rates for modern contraceptives from NDHS data in 1990 and 1999 were 7.5% and 9% respectively. Although there was an increase in the utilization of modern contraceptive methods in 1999 compared to 1990, utilization of family planning seems to have stagnated since 1999. This implies that contraceptive use is still a critical public health agenda in Nigeria. Monjok et al (2010) in their review of contraceptive use in Nigeria and its implication for future policy decisions suggested that “connection has to be made between those involved with research and those involved with policy and governance. Particularly, research information must be shared to generate political priority with politicians and those who have power to take appropriate action.In addition, women residing in urban areas were significantly more likely to currently use modern contraceptive method compared to the women who live in rural areas. This is similar to studies by Bogale et al, Arbab et al., and Olalekan et al. [2, 14, 15], which showed a significant association between contraceptive use and place of residence, as women who live in urban areas had greater chance of being more educated, more access to health facilities, greater exposure to mass media messages more knowledge about modern contraceptive issues than their counterpart who dwell in the rural areas where unmet need for family planning has been shown to be high.There was a direct relationship between contraceptive use and levels of education of the women as we observed that women who had higher, secondary and primary education were all more likely to currently use modern contraceptive than their counterparts who had no form of education. Similar patterns have been shown in Nigeria [15, 16]. Generally, education is a major determinant of utilization of health services. This is achieved by improving health literacy and empowering individual to make informed choices about modern health facilities. In addition, contraceptive use has been shown to affect the timing for fertility among career women. For instance, late marriage due to time spent studying has been documented to facilitate more use of contraception among educated women than illiterates [15, 17].The data further shows that currently married women and formerly married women were significantly less likely to currently use modern contraceptive method than women who were never married [18]. Married women have high frequency of sexual exposure and are at higher risk are more at risk of pregnancy than unmarried women. Therefore have a greater need for contraceptive especially for spacing and limiting births [18]. However, the never-married women, including adolescents and young women, but sexually active are increasing using contraceptives to prevent sexually transmitted disease especially HIV/AIDS. Although, they have a great disadvantage in obtaining contraceptives largely due to stigma attached to being sexually active before marriage. Among women in need of contraceptive use of modern methods is thirty-one percentage points lower among never married women than among married women in Asia; this difference is ten percentage points in Latin America and the Caribbean. However, the situation is reversed in Sub-Saharan Africa, where the proportion of never-married, mostly adolescents and young women in need using modern contraceptives is nineteen percentage points higher than among their married counterparts [19].Furthermore, in this study, respondents from the southwest and South-southregions were significantly more likely to use contraception as compared to the respondents from the north central zone of the country, while those from the northeast, northwest and southeast were less likely to use contraceptive. This is related to the postulation that family planning is more acceptable in the southern states of Nigeria than in the northern states [19-22]. Previous studies have shown that Northern Nigeria is more resistant to family planning services. Therefore, this regional difference informs the need to adopt innovative strategies in the provision of family planning services. This means that in addition to facility based delivery of contraceptive commodities, community based delivery which includes the participation of non-governmental agencies in creating awareness, sensitization, health education and delivery of commodities need to be promoted.Catholic respondents, other Christians, Traditionalists and respondents from other denominations in this study were significantly more likely to currently use modern contraception compared to Muslim respondents. This finding corresponds to that in similar studies carried out in parts of northern Nigeria [20]. This is so because it has been shown that Muslims have lower level of education as compared to Christians, as such the later are more predisposed to information about the importance of utilisation of family planning services. It was also observed that women of Igbo and Yoruba ethnicity were significantly more likely to currently use modern contraceptive method as compared to Hausa respondents.Direct relationship between current modern contraceptive use and wealth index was observed in this study. The data showed that the respondents who belong to the middle wealth quintile were significantly more like to currently use modern contraceptive as compared to the women that belong to the poorest wealth quintile. This is similar to the findings of [18] because in Nigeria, contraceptive services are not free. This implies that the services cannot be paid for by the poorer population as a result of their financial inability, because a higher proportion of Nigerian population are very poor. A study by Creanga et al. compared two Demographic and Health Surveys (DHS) in 13 sub-Saharan African countries. They reported a decrease in wealth-related inequalities in the met need for contraception in some countries and an increase in others. In a similar manner, it was found that contraceptive use in general increased substantially in Ethiopia, Madagascar, Mozambique, Namibia and Zambia attributable to the increased uptake of short-term contraceptive methods while there was a marginal decline in Malawi, Senegal and Uganda. In addition, the increase in use of long-term contraceptive methods was almost negligible, and five countries (Cameroon, Kenya, Mozambique, Rwanda and Senegal) experienced a reversal trend in use [23]. Duff Gillespie et al. studying data from 41 developing countries found the poorest quintile had a total fertility rate of six (6), twice as high as that found in the wealthiest quintile. They suggest that reducing inequality in access to modern contraception will also reduce the inequality in fertility [24]. Hotchkiss and colleagues observed that the increased role of the private commercial sector in supplying modern contraceptives in Nigeria, Uganda, Bangladesh and Indonesia resulted in reduced inequality in modern contraceptive prevalence rates over time [25].
5. Conclusions
- In conclusion, prevalence rates were very low across almost all segments of the population. Therefore, we recommend concerted efforts to the policy makers to intensify awareness on utilisation of modern methods of contraception in Nigeria.
ACKNOWLEDGEMENTS
- The authors are grateful to Professor Olusola Ayeni who supervised this work and we thank Macro-International U.S.A and National Population Commission for allowing us to use their data (NDHS, 2008) for this study. We are also thankful for the support of the entire staff of the department of Epidemiology and Medical Statistics, University of Ibadan.
Ethics
- Ethical exemption was gotten from the University College Hospital institutional review board (IRB). However, an authorization to download the dataset was obtained from the Demographic and Health Surveys (DHS) on-line archive.
Funding
- No funding for the study
Conflict of Interests
- The authors declare that they have no conflicts of interest in relation to this article.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML