-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2014; 4(1): 7-10
doi:10.5923/j.health.20140401.02
Pattern of Drug Utilization in the Treatment of Chronic Suppurative Otitis Media in a Tertiary Health Institution in Kaduna, Nigeria
Abubakar K.1, Abdulkadir R.2, Abubakar M. R.1, Ugwah-Oguejiofor J. C.1, Abubakar S. B.3
1Department of Pharmacology and toxicology, Faculty of Pharmaceutical Sciences, Usmanu Danfodiyo University Sokoto, Nigeria
2Pharmacy Department National Ear Care Centre Kaduna, Nigeria
3Department of Haematology and Pathology, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria
Correspondence to: Abubakar K., Department of Pharmacology and toxicology, Faculty of Pharmaceutical Sciences, Usmanu Danfodiyo University Sokoto, Nigeria.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
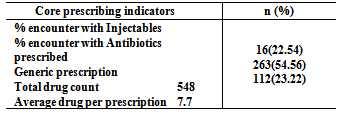
Objective:A prospective study was undertaken to find out the baseline data on the prescribing pattern of drugs in the treatment of chronic suppurative otitis media.Materials and methods: Prescriptions for chronic suppurative otitis media were collected from the outpatient department of National ear care centre, Kaduna Nigeria, over a period of six months and were analyzed by employing the WHO/INRUD methods of determining core prescribing indicators. Result: Children were the most diagnosed with CSOM 60.6%, the major diagnostic symptom was otorrhea 85.2%. Antibiotics were the most prescribed drugs 48% and antihistamines prescription was also significant 21.5%.The quinolone antibiotics were the most prescribed group of drugs, percentage encounter with injection was 22.54%, prescription with generic name 23.22% and total number of medicine per prescription was 7.1.Oral dosage forms were the most prescribed drugs in this study (78.4%).Conclusions:The present work is the maiden drug utilization studies for the treatment of CSOM in the outpatient department of this hospital. Most of the indicators for rational prescription were being observed by the prescribers. There is still need for improvement in the area of prescribing with brand names and polypharmacy.
Keywords: Drug utilization, CSOM, Antibiotics and polypharmacy
Cite this paper: Abubakar K., Abdulkadir R., Abubakar M. R., Ugwah-Oguejiofor J. C., Abubakar S. B., Pattern of Drug Utilization in the Treatment of Chronic Suppurative Otitis Media in a Tertiary Health Institution in Kaduna, Nigeria, Journal of Health Science, Vol. 4 No. 1, 2014, pp. 7-10. doi: 10.5923/j.health.20140401.02.
Article Outline
1. Background
- Ear nose and throat (ENT) infections are common clinical problems occurring in the general population and are a cause of serious morbidity and debility. These infections affects the normal daily functioning of both adults and children and are the frequent cause of absenteeism from work and school among school aged children[1]. As with other infections of the upper respiratory tract (URT), ear infections such as chronic suppurative otitis media are of great concern especially in developing countries, such as retarded language development and progress in school among children[2, 3]. Otitis-media (which means an inflammation and infection of the middle ear) is now known to be the most common childhood infection which leads annually to the death of over 50,000 children under 5 years[4]. The prevalence rate of ENT diseases is particularly high in developing countries; diseases such as Otitis media had a reported prevalence of 65%[5]. The WHO estimated that URT infections generated a 94.6% disability adjusted life years and were responsible for 6.9% of the global number of deaths in 2002[6]. Otitis media infection occurs less common in adults compared to children, it is one of the most common reasons parents take their children to the hospital. According to a report[7, 8] acute otitis media are the most common childhood infection and the most common indication for antibiotic use in children. In the USA acute otitis media is responsible for up to 20 million physician visit per year representing an average of 2.9 physician office visits per child[9].One of the ENT diseases resistant to current antibiotics is chronic suppurative otitis media (CSOM)[10].Chronic suppurative otitis media is an infection of the middle ear lasting for more than two weeks, mostly (CSOM) holds perforation of the tympanic membrane and discharging [11] for at least two weeks. Many factors predisposes individuals to CSOM, they include genetic, infectious, hygienic and environmental factors[12]. Other less common causes includes low socio-economic status, allergy and overcrowding[12]. The major complication of CSOM is hearing impairment which may be preceded by purulent otitis often with perforation and further complications including recurrent acute otitis media, persistence of middle ear effusion which requires the insertion of drainage tube, mastoiditis, meningitis, brain abscess and sepsis[13]. Different group of drugs are employed in the management of ear infection; such drugs include analgesics, anti histamines, antiallergins and antibiotics. The drugs are administered in the form of tablets, capsules, syrups and instillations. Antibiotics appear to be the most frequently used class of drugs owing to the etiology of the disease condition. The prescription and use of antibiotics in URT infections as with other infections is facing a lot of challenges which include over use and misuse which leads to development of resistance[14]. Variability in the prescription of antibiotics do occur and this can be attributed to the infecting organism and antimicrobial susceptibility that differs from country to country, other factors may include physician preference, local policy, costs and lack of local guidelines[15].The present study explored the pattern of prescription of drugs used for the treatment of chronic suppurative otitis media in a Tertiary Ear Care centre in Kaduna Nigeria. The study is aimed at critically analyzing the prescriptions issued from the outpatient department of the hospital. It is the desire of the study to find out areas that needs adjustment and improvement in the overall interest of the patient and the healthcare system.
2. Materials and Methods
2.1. Setting
- The study was carried out in the out- patient department of the National Ear Care Centre Kaduna, Nigeria between January and May 2011 (six months).
2.2. Study Design
- It was a cross sectional retrospective study and was based on the prescriptions coming to the pharmacy from the outpatient clinic of the Hospital.
2.3. Study Population
- The present study was conducted on 121 prescriptions which were obtained from the prescription records of the pharmacy Department of the Hospital. Seventy one Prescriptions were found to satisfy the inclusion criteria for the study. The sample prescriptions were investigated using a checklist for the following items: Legibility of handwriting, date of prescription, patient’s name in full, patient’s address, patient’s age, patient’s sex, doctor’s name, doctor’s signature in ink, dosage form, type and number of drugs prescribed and the number of drugs per prescription. Other Information obtained from the patient case files were the presenting symptoms and the diagnosis. The study population included all patients whose prescription was filled at the pharmacy those patients that did not obtain their drugs from the pharmacy were not included.
2.4. Parameters for Evaluation
- The WHO/INRUD methods of describing core prescribing indicators were employed. The average number of medicines per prescription was calculated by dividing the total number of drugs by the number of encounters. Percentage encounter with generic name, percentage encounter with antibiotics and percentage encounter with injections were determined by dividing the number of occurrence by the total number of event, respectively and multiplying by 100. Other parameters evaluated includes gender distribution, average age range of patients, types of infections, most commonly used agents of a particular class, comparison of antibacterial prescribed in monotherapy versus fixed dose combination therapy and mode of administration.
3. Results
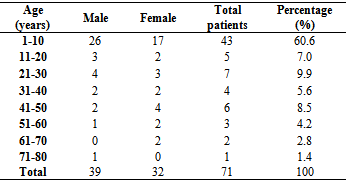
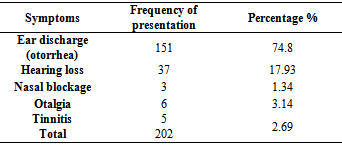
- During the study period (Jan- May, 2011) a total of 71 prescriptions were evaluated. Out of the total number of patients, 41 patients were males and 30 females. Among total patients 46 were children (1-12years) and 25 adults (>13 years). During the study it was observed that the highest number of patients was in the age group (1-10 years) and the geriatric group was the least [Table 1]. The major presenting complain was ear discharge 76.5%, followed by hearing loss and otorrhea 8.8% [Table 2].
|
|
|
|
4. Discussion
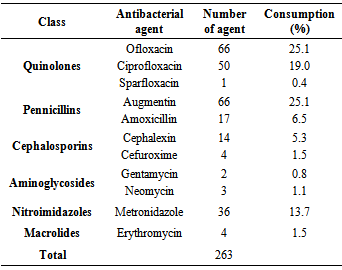
- This study comprises essentially of an audit of various prescriptions issued for the treatment of chronic suppurative otitis media carried out over a period of six months (January- may 2011). Data collected from 71 prescriptions were analysed, and the findings compared with similar studies published. The study targeted chronic suppurative otitis media alone, therefore, prescriptions for acute otitis media and other ENT diseases were excluded.Demographic data showed that 60.6% of the patients were children between the ages of (1-10 years). These finding are consistent with 34-46 % reported in previous studies[17, 18]. Anatomical and immunological considerations could be the reason why children are more susceptible to this infection; the Eustachian tube in children is shorter and more horizontal than adults and is made up of more flacid cartillage which can impair its opening[19]. Another point for consideration is the immature nature of children’s immunity[20]. The study also showed that the percentage of males suffering from CSOM was more than females. Similar findings were reported by[21, 22].Ear discharge (otorrhea) was the most common diagnostic symptom in 85.3%, followed by hearing loss 8.8%. Nasal discharge, cough and swelling were the least observed diagnostic symptoms 1.5% respectively. Similar result of 50% presentation of otorrhea was reported by[23] in a study of the prevalence of chronic suppurative otitis media and hearing impairment in Basrah city, the result disagreed with the result of[24] who reported that otorrhea was commonly found in otitis externa. Hearing loss was present in 8.8% of the patients, this was significantly lower than a presentation of 55.5% as reported by[23]. The specificity of the researched disease condition (CSOM) accounts for the low value of the other diagnostic symptoms in (table 2).Antibiotics were the most prescribed drugs in this study (48%), followed by antihistamines 21.5% and multivitamins 15%. Another class are the miscellaneous groups (9.1%), such as ear drops, oils such as eucalyptus oil, nasal drops and nasal spray. Analgesic and steroids were the least prescribed. Previous study of the prescription pattern of CSOM also indicated a prevalent prescription of antibiotics such as[25] and[26].Most commonly prescribed class of antibiotics were the quinolones (44.5%), closely followed by the Pennicillins (25.1%) and the Nitroimidazoles 13.7%.The cephalosporins frequency was 6.8%, followed by the Aminoglycosides 1.9% and the least prescribed was the macrolides 1.5%. Most studies favour the use of the Pennicillins and cephalosporins over the quinolones[25, 26]. The preference for quinolones was observed in some past studies as was the case with this study, this could be due to the fact that the drugs have oral antipseudomonal activity and lack ototoxicity side effect[27]. The oral and topical quinolones have been used effectively in children and such use will avert the inconveniences of the parentheral antibiotics[28,29,30].Most of the drugs in the study were prescribed using brand names (data not displayed) and the average number of medicine per prescription was 7.6, the range being (1-11) [16]. Orally administered drugs were the most frequent dosage forms in this study (78.4%), this could be due to convenience especially in children.
5. Conclusions
- The prescription behaviour of physician in the hospital under review is encouraging. The report is in line with results obtained from similar studies; however there is a need to improve on the use of generic names instead of brand names and the need to use less number of drugs per patient.
ACKNOWLEDGEMENTS
- The authors wish to express their appreciation to the management of the National ear care centre Kaduna, Nigeria for providing the enabled environment that made this research successful.
References
| [1] | Witsell DL, Dolor RJ, Bolte JM, Stinnet SS. Exploring health-related quality of life in patients with diseases of the ear, nose and throat: A multicenter observation study. Otolaryngology – Head and neck Surgery. 2001; 125-134 |
| [2] | WHO Conquering suffering, Enriching humanity. World Health Organization report, WHO, Geneva; 1997. |
| [3] | Newton EV, Macharia I, Mugwe P, Ototo B, Kan SW. Evaluation of the use of a questionnaire to detect hearing loss in Kenyan pre-school children. International Journal of Paediatric Otorhinolaryngology. 2001; 57:229–234. |
| [4] | Rovers MM, de Kok IMCM, Schilder AGM. Risk factors for otitis media: An international perspective. International Journal of Paediatric Otorhinolaryngology. 2006; 70:1251–1256 |
| [5] | WHO/PDH Prevention of hearing impairment from chronic Otitis media. Report of WHO/CIBA Foundation workshop, Geneva; 1996. 19–21, November, 1996. |
| [6] | Geneva, Switzerland: World Health Organization; 2004. Burden of illness and management options. |
| [7] | Froom J, Culpepper L, Grob P, et al. Diagnosis and antibiotic treatment of acute otitis media: report from International Primary Care Network. Br. Med J. 1990; 300:582–6. |
| [8] | Bergus GR, Levy BT, Levy SM, Slager SL, Kiritsy MC. Antibiotic use during the first 200 days of life. Arch Fam Med. 1996; 5:523–6. |
| [9] | Thompson D, Oster G, McGarry LJ, Klein JO. Management of otitis media among children in a large health insurance plan. Pediatr Infect Dis J. 1999; 18:239–44 . |
| [10] | Megale SRMCL, Scanavini ABA, Andrade EC, Fernades MIM, Anselmo-Lima WT. Gastroesophageal reflux disease: Its importance in ear, nose, and throat practise. International journal of Paediatric Otorhinolaryngology. 2006; 70:81–88. |
| [11] | Seid A et al. Bacterial otitis media in all age group of patients seen at Dessie referral hospital, North East Ethiopia. Egypt J Ear Nose Throat Allied Sci.2013; 02.005 |
| [12] | Lasisi AO, Olayemi O, Irabor AE. Early onset otitis media: risk factors and effects on the outcome of chronic suppurative otitis media. Eur Arch Otorhinolaryngol. 2008; 265:765–768. |
| [13] | Winn W, Allen S, Janda W, et al. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology. 6th ed. Philadelphia USA: Lippincott’s Williams and Wilkins; 2006, p. 439–440 and 211–302. |
| [14] | Przemyslaw K. Patient compliance with antibiotic treatment for respiratory tract infections. J Antimicrob Chemother. 2002; 49:897–903 |
| [15] | Needham A, Brown M, Freeborn S. Introduction and audit of general practice antibiotic formulary. J R Coll Gen Pract. 1988; 38:166–7. |
| [16] | Abubakar K, Muhammad A.A, Jimoh A.O, Abubakar S.B. Prescription Pattern of Antipsychotic Drugs-A Case study of a Neuro-psychiatric Hospital in North-Western Nigeria. European Journal of Scientific Research ISSN: 1450-216X / 1450-202X Vol. 95 No 3 January, 2013, pp.332-337. |
| [17] | Jha AK, Singh JB, Dutta D. Microorganisms present in discharging otitis media in a group of patients in Kathmandu. Nepal Med Coll J. 2007;9(3):196–198. |
| [18] | Mansoor T, Musani MA, Khalid G, Kamal M. Pseudomonas aeruginosa in chronic suppurative otitis media: sensitivity spectrum against various antibiotics in Karachi. J Ayub Med Coll Abbottabad. 2009; 21(2):120–123. |
| [19] | Vanderven E.L, Schilder AG, VanHeerbeek N, Verhoeff M, Zielhuis GA, Rovers MM. Predictors of chronic suppurative otitis media in children. Arch Otolaryngol. Head Neck Surg. 2006; 132 (10):1115-1118. |
| [20] | Grote JJ, Vallely PJ. Otitis media. In: Newton VE, Valley PJ, eds. Infection and Hearing Impairment. England: John Wiley & Sons Ltd; 2006:71–181. |
| [21] | Shankar PR, Upadhyay DK, Subish P, Dubey AK, Mishra P. Prescribing patterns among paediatric inpatients in a teaching hospital in western Nepal. Singapore Med J. 2006; 47:261-5. |
| [22] | Pradhan S, Jauhari AC. A study of antibiotics used in adult respiratory disorders in Kathmandu and Bhaktapur. Nepal Med Coll J. 2007; 9:120–4. |
| [23] | Ahmed M.Alabbasi,Ihsan E. Alsaimary,Jassim M. Najim. Prev alence and patterns of chronic suppurative otitis media and hearing impairment in Basrah city, journal of Medicine and Medical Sciences 2010 Vol 1 (4) pp. 129-133 |
| [24] | Bardanis J, Batzakkis D, Mamatas S.Types and causes of otorrhea. Auris Nasus larynx.2003; 30:253-257 |
| [25] | M.R. Ain,N.Shahzad,M.Aqil, M.S. Alam, R.Khanam. Drug utilization pattern of antibacterials used in ear,nose and throat outpatients and inpatient departments of a university hospital at New Delhi, India. J Pharm Bioallied Sci.2010; 2(1) 8-12. |
| [26] | Rehan H.S. Pattern of drug utilization in acute tonsilitis I a teaching hospital in Nepal. Indian Journal of Otolaryngology and head and Neck surgery; 2003: Vol 55 No 3 pp 176-179. |
| [27] | Claes J,Govaerts PJ,Van de Heyning PJ, Peeters S. Lack of ciprofloxacin ototoxicity after repeated ototopical application. Antimicrobial agents chemother 1991;1014-6 |
| [28] | Force R.W, Hart M.C, Plumme S,A, Powell D.A,Nahata M.C.Topical ciprofloxacin for otorrhea after tympanostomy tube placement. Arch. Otolaryngol Head Neck Surg. 1995;121:880-4 |
| [29] | Lang R, Goshen S.Raas-Rothschild A,Raz A, Ophir D, Wolach B et al.Oral ciprofloxacin in the management of chronic suppurative otitis media without choleasteatoma in children: Preliminary experiences in 21 children. Paediatr. Infect Dis J 1992; 11:1925-9. |
| [30] | Wintermeyer SM, Hart MC, Nahata MC.Efficacy of ototopical ciprofloxacin in paeditric patients with otorrhea. Otolaryngol Head Neck Surg 1997; 116: 450-3. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML