-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Sciences
2012; 2(4): 29-32
doi: 10.5923/j.health.20120204.02
Physical therapy management of Anterior Canal Benign Paroxysmal Positional Vertigo by the Deep Head Hanging Maneuver
Amer A. Al Saif 1, Samira Alsenany 2
1Department of Physical Therapy, Faculty of Applied Medical Science, King Abdulaziz University, Jeddah, Saudi Arabia
2Faculty of Applied Medical science, King Abdulaziz University, Jeddah, Saudi Arabia
Correspondence to: Amer A. Al Saif , Department of Physical Therapy, Faculty of Applied Medical Science, King Abdulaziz University, Jeddah, Saudi Arabia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
One important factor that can cause of dizziness is benign paroxysmal positional vertigo (BPPV); this increases in prevalence with age. The aim of this clinical study was to determine whether the Deep Head Hanging maneuver is an efficacious treatment maneuver for anterior canalithiasis. Twenty-eight adult participants were recruited. Their ages ranged from 41–63 years. Thrteen participants were male, and fifteen were female. Participants were judged to be “clear” of the anterior canalithiasis when there was no nystagmus or subjective vertigo elicited by diagnostic positioning at the follow-up appointment. Results indicate that 82.1 % of the twenty-eight participants were clear of anterior canalithiasis after one treatment session, with another 14.2 % clear after a second treatment session. The remaining 3.5 % required a third treatment session. In Conclusion, the Deep Head Hanging maneuver was demonstrated to be a useful treatment in patients presenting with possible anterior canalithiasis sessions.
Keywords: Dizziness, Canalithiasis, Benign Paroxysmal Positional Vertigo , Deep Head Hanging maneuver, Vertigo
1. Introduction
- One important factor that can cause of dizziness is benign paroxysmal positional vertigo (BPPV); this increases in prevalence with age. Significantly, a study that compared patients with BPPV referred initially to a Falls and Syncope Unit (FSS group) found that FSS patients were more likely to have more than one type of dizziness (16% vs. 0%, p = 0.001), more likely to have cerebrovascular or cardiovascular co-morbidity (13% vs. 4%, p = 0.0152) and were taking significantly more medication (3.2 vs. 1.7; p = 0) and that these issues could be a curable cause for dizziness and so of falls in older people1).Similarly, another study to differentiate between dizziness and balance disorders used a cross-sectional design to verify the occurrence of unrecognized benign paroxysmal positional vertigo (BPPV) and associated lifestyle issues in a public, inner-city geriatric population. The study noted that dizziness was common in 61% of patients, whereas balance disorders were found in 77% of patients. In addition, nine percent were found to have unrecognized BPPV. Multivariate analysis demonstrated that the presence of a spinning sensation and the absence of a lightheadedness sensation predicted the presence of unrecognized BPPV. Patients with unrecognized BPPV were more likely to have reduced activities of daily living scores, to have had continual falls in the previous three months, and to have depression. These data indicate that unrecognized BPPV is common among older people and is related to causes of death 2). Significantly, many older people with dizziness complain of two diverse types of dizzy symptoms3). The most common is a gait disorder, but they may also have symptoms stemming from the cardiovascular and peripheral vestibular systems. Furthermore, some causes of dizziness represent a danger to life. Similarly, another study found that occurrence of BPPV increases with age. Older people suffering from dizziness may be transferred to a different special unit . Usually, the diagnosis of posterior canal BPPV is expected when typical signs (nystagmus) and symptoms (vertigo and nausea) are aggravated by positional tests such as the Dix-Hallpike test1).Benign paroxysmal positional vertigo (BPPV) is the most common otologic cause of dizziness4,5). It is caused by abnormal mechanical stimulation of one or more of the three semicircular canals (SCC) of the inner ear. Within the labyrinth of the inner ear lie collections of calcium crystals known as otoconia2). For a variety of reasons, in patients with BPPV, the otoconia are dislodged from their usual position within the utricle and travel through the endolymphatic fluid into one of (SCC)5) .The presence of the otoconia in one of the three semicircular canals causes the involved semicircular canal to become sensitive to changes in orientation of the head in the plane of the canal. It has been reported that 80-95% of all BPPV cases are the result of otoconia being trapped in the posterior SCC (PSC) and 10-12%in the horizontal SCC (HSC)4,5). There is much more debate concerning the anterior SCC (ASC) and reports vary from 2-21% of cases6) . Symptoms of BPPV include brief attacks of dizziness or vertigo associated with nystagmus, blurred vision, lightheadedness, loss of balance and nausea that are triggered by angular position changes such as bending forward, sitting up, and rolling over in bed2) . The symptoms can last for days, weeks, or months, or be recurrent over many years. In around half of BPPV cases, no cause can be found (idiopathic BPPV). However, in older people, the most common cause is degeneration of the gelatinous matrix within the utricle supporting theotoconia2,7). The diagnosis of BPPV is relatively straightforward due to the characteristic history and positional vertigo, that can be induced using the Hallpike-Dix maneuver2). The addition of using infrared goggles with the Hallpike-Dix maneuver improves the accuracy of the test. During the Hallpike-Dix maneuver, the patient long-sits on an examination table with their head rotated approximately 45 degrees to one side. The clinician then assists the patient into a supine position with their head and neck extended slightly below the level of the table while maintaining the rotated head position2,8,9) . The symptoms typically begin a few seconds after assuming this position. This is due to the gravitational impact of the test position which moves the otoconia within the SCCs. This increases the internal pull on the endolymphatic fluid of the SCC, producing a more vigorous bending of the cilia within the ampulla of the SCC2) . The end result of the Hallpike-Dix test, in the presence of BPPV, is vertical-torsional jerk nystagmus of typically short duration, suggesting a specific type of BPPV called canalithiasis. In this research study, we have operationally defined BPPV as the canalithiasis form. The clinician can determine the SCC involved by analyzing the eye movements provoked and the latency of nystagmus2). ASC BPPV is characterized by paroxysmal down-beating nystagmus lasting less than 60 seconds10,11). The most common clinical intervention for canalithiasis of the ASC is the canalith-repositioning maneuver (CRM). However, recent literature suggests using the (DH maneuver), as illustrated by Yacovino et al, as the primary treatment for ASC BPPV13). The DH maneuver is performed on an examination table in a similar manner to the CRM. Because the ASC has a different trajectory from the PSC, maneuvers targeting ASC BPPV differ geometrically from those described by Epley for PSC BPPV10). The idea of the DH maneuver is to invert the ASC to allow debris to fall to the "top" of the ASC, and then, upon returning the patient to the sitting position, allow it to migrate into the common crus and then the utricle10). The purpose of the current investigation was to determine whether the DH maneuver is an efficacious treatment maneuver for ASC-BPPV.
2. Methods
 | Figure 1. Deep Head Hanging Maneuver (Positions 1-4) |
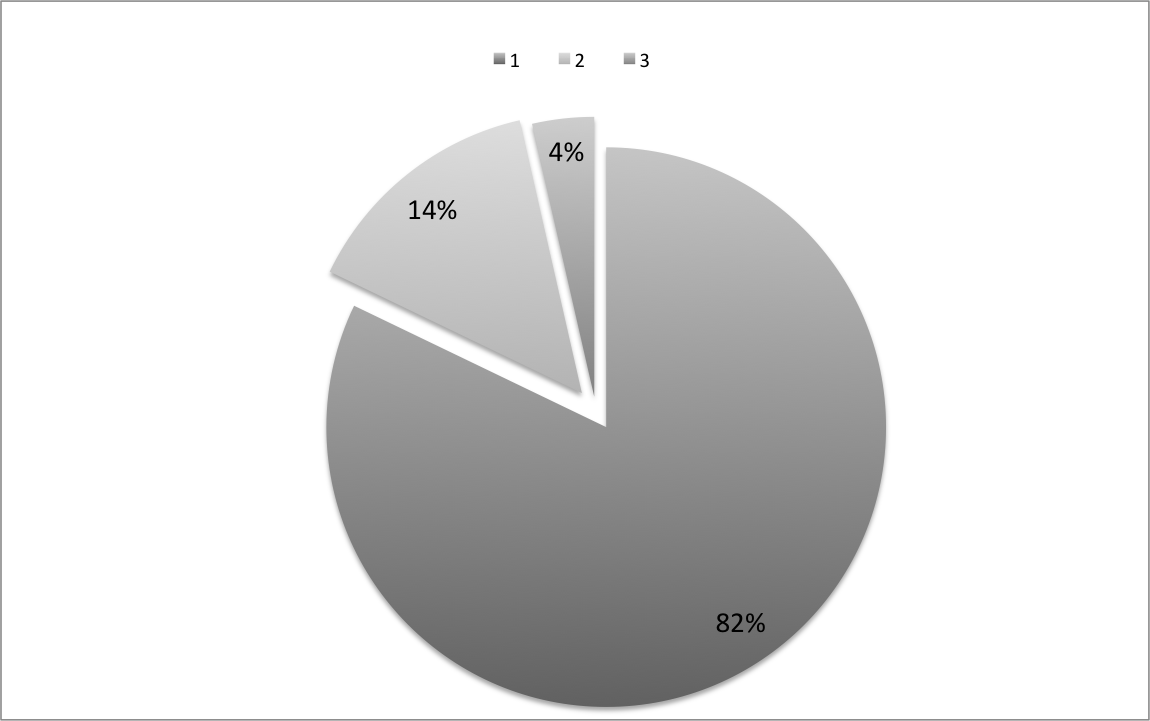 | Figure 2. Percentage of patients cleared of AC BPPC over the number of treatment sessions |
- All twenty-eight adult participants were recruited from patients seen at King Abdulaziz University Hospital. Informed consent was acquired prior to the beginning of the study. Age ranged from 41–63 years with an average age of 55 years. Thirteen participants were male, and fifteen were female. AC BPPV was confirmed in all participants with Video-Nystagmography recording (VNG) after it was determined that there was no central-mediated problem. Participants were treated with the DH maneuver as illustrated by Yacovino et al16). This consisted of four steps with intervals of at least thirty seconds (Figure 1). In Yacovino et al.’s method the the patient was first assisted from a sitting position into a supine position with their head extended backwards by 30°. This position is maintained while their head is flexed forward 45°. Finally, the patient is returned to the sitting position. In position 1, the otoconia lie near the ASC ampulla .In position 2 (head-hanging position), both ASC’s are inverted with their ampullas superior and their non-ampullary endings medial and inferior. Otoconia migrate due to their weight towards the apex of the ASC. In position 3 (chin to chest), gravity facilitates further migration towards the common crus. Finally, in position 4, the patient sits up with head tucked in. This last step allows otoconia to move through the common crus and into the utricle. The author, who is experienced in the treatment of ASC-BPPV using the DH maneuver, conducted all treatment sessions. All participants received one DH maneuver treatment per appointment and returned for follow-up evaluation at one-week intervals. Participants were judged to be “clear” of the ASC-BPPV when there was no nystagmus or subjective vertigo elicited by diagnostic positioning at the follow-up appointment.
3. Results
- Participants included in the study were telephoned one month following initial clearance by the DH maneuver and all reported 100% resolution of all symptoms.. As shown in Figure 2, 82.1 % of the twenty-eight participants were clear of AC-BPPV after one DH treatment session, with another 14.2 % clear after a second treatment session. The remaining 3.5 % required a third treatment session. All participants were cleared within three treatment sessions.
4. Discussion and Conclusions
- The mechanism driving BPPV is otoconia pathologically located in one of the three SCCs of the inner ear. Because otoconia have mass, angular position changes affect the involved SCC as the otoconia move within the endolymphatic fluid2). This movement results in an increased neural firing rate of the involved inner ear and a sensory mismatch between the systems responsible for position -sense and balance2,15). The symptomatic consequences include nausea and vertigo lasting from seconds to minutes1,2). Medical management aimed at resolving BPPV includes the CRM and/or liberatory maneuvers depending upon the specific BPPV type1,2). The purpose of the current investigation was to determine whether the DH maneuver wasis an efficacious treatment maneuver for AC-BPPV. Results from the current study indicate that the DH maneuver is successful in clearing AC-BPPV. The purpose of the DH was to remove physically the otoconia from the SCC and relocate them back into the utricle using gravity and a systematic progression of head position changes4, 10. Approximately 96% of patients were clear within one or two treatments. one study reported that all cases showed excellent therapeutic response to the DH maneuver16). Another study reported that vertigo and nystagmus in 29 patients fully resolved using this maneuver, 96.7% of patients became symptom free17). Based on these findings and our results, and DH maneuver could be one of the most effective treatment methods for ASC BPPV. This compares well with data reported in previous studies of treatment maneuvers for AC-BPPV using the DH maneuver as the primary treatment for ASC BPPV. The DH maneuver has the advantage that the clinician does not need to know the affected side13). The ASC is much nearer to the sagittal plane than the PSC, so keeping the head in a neutral non-rotated position is more beneficial in mobilizing the particles in the ASC compared to rotatory movements13). There are two major limitations in this study: the lack of a control group and the difficulty in recruiting patients with ASC-BPPV because it is a rare condition. Based upon the results of the current study, the DH maneuver was demonstrated to be a useful treatment in patients presenting with possible ASC BPPV. Moreover, the results from the current study indicate that approximately 96% of the participants were clear after one or two DH maneuvers.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML