-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2011; 1(1): 16-22
doi: 10.5923/j.health.20110101.03
Using Informal Conversation in the Clinical Setting as a Measure of Communication Potential for Adults with Aphasia
Kim C. McCullough
Department of Speech Language Pathology, University of Central Arkansas, Conway, 72035, United States of America
Correspondence to: Kim C. McCullough , Department of Speech Language Pathology, University of Central Arkansas, Conway, 72035, United States of America.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
The purpose of this study was to investigate the clinical usefulness of informal conversation as a tool for determining ability to communicate potential regardless of modality (verbal or nonverbal). Four individuals with aphasia (two non-fluent and two fluent) and four non-impaired individuals participated in this study. Selected segments of conversational discourse were analyzed for communication act usage during a 20-30 minute dyadic interaction with the investigator. Results revealed no significant differences between the total number of communication acts used by the participants. However, the participants with aphasia used a higher number of nonverbal and a combination of both verbal and nonverbal acts when compared to the non-impaired participants. Implications for clinical application are discussed.
Keywords: Aphasia, Communication, Conversation, Verbal, Non-Verbal
Cite this paper: Kim C. McCullough , "Using Informal Conversation in the Clinical Setting as a Measure of Communication Potential for Adults with Aphasia", Journal of Health Science, Vol. 1 No. 1, 2011, pp. 16-22. doi: 10.5923/j.health.20110101.03.
Article Outline
1. Introduction
- Given that communication is required for most daily activities, the impact of aphasia on functions of everyday life can be significant. Concepts of aphasia have been influenced by the World Health Organization’s International Classification of Functioning, Disability, and Health (ICF). The ICF model provides clinicians with a framework for conceptualizing the development of treatment goals, not only for impairment and activity limitations but also for participation in life situations and social roles. The American Speech-Language-Hearing Association (ASHA) has recommended the use of the ICF model as outlined in the Scope of Practice in Speech-Language Pathology (ASHA, 2001) and Preferred Practice Patterns for the Profession of Speech-Language Pathology (ASHA, 2004). ASHA encourages clinicians to address impairments, activity limitations, and participation restrictions in their assessment and treatment of communication disorders. Additionally, ASHA recommends that clinicians recognize the environmental and personal factors that may have an influence on communication.The ICF defines communication for societal participation as “holding a conversation: starting and sustaining an interchange of thoughts and ideas, carried out by means of spoken, written, sign or other forms of language, with one ormore people one knows or who are strangers in formal or casual settings” (WHO, 2001, p. 135). The strategic use of informal conversation is a readily available tool that clinicians can use as a way to develop treatment goals that will facilitate a person’s potential for societal participation.The present investigation used the concept of “communication acts” as a means for estimating communication potential. This investigation was designed to explore how individuals with aphasia circumvent their verbal deficits by using nonverbal strategies when expressing a communicative intent.The results of previous investigations relating to usage of communication acts during conversation and aphasia suggest that communication acts may not necessarily be resistant to the breakdown that is seen in other aspects of the language of individuals with aphasia, as indicated by Holland (1982). Instead, it appears that some individuals with aphasia may exhibit a normal range of communication acts in comparison to non-impaired participants (Glosser et. al, 1988; Guilford & O'Connor, 1982; Holland, 1982; Prinz, 1980), whereas others may display a restricted range of communication acts (Gurland, Chwat, & Wollner, 1982; Prutting & Kirchner, 1987; Wilcox & Davis, 1977). One limitation of the above studies is that they fail to consistently report the extent to which individuals rely on nonverbal variables to communicate their message. Because nonverbal features (Damico et. al, 2008) are an inherent component of communicative interactions, inclusion of this data would provide a more accurate characterization of the ability of individuals with aphasia to effectively communicate intent.The purpose of this study was to compare the use of communication acts by individuals with aphasia and non-impaired individuals. An attempt was made to answer the following questions: 1) Is there an apparent difference in the number of communication acts used by individuals with aphasia and non-impaired individuals during informal conversation?; 2) Is there an apparent difference in the number of verbal and nonverbal communication acts used by individuals with aphasia and non-impaired individuals during informal conversation?; and 3) Is there an apparent difference in the distribution of usage across different types of communication acts that are expressed by individuals with aphasia and non-impaired individuals during informal conversation?
2. Method
2.1. Participants
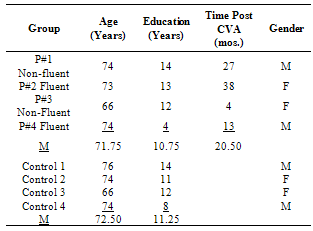
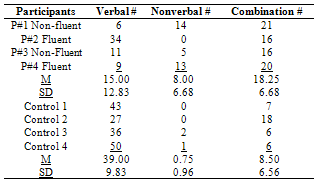
- Four individuals with aphasia (two fluent and two non-fluent) and four non-impaired controls participated in this study. All participants were recruited through local nursing homes. The participants with aphasia were all pre-morbidly right-handed, native English speakers with a mean age of 71.25 years and a mean education level of 11.25 years. Participants were at least two months post-onset to insure medical stability. According to each participant's history, there was no evidence of neurologic disorder; psychiatric disorder; or speech, language, and hearing problems previous to the stroke.The non-impaired participants were all pre-morbidly right-handed, native English speakers with a mean age of 72.5 years and a mean education level of 10.75 years. According to each participant's history, there was no evidence of neurologic disorder; psychiatric disorder; or speech, language, and hearing problems. The non-impaired participants were matched in age, gender, and education with the participants with aphasia. Two females and two males were recruited for each participant group. Table 1 summarizes information obtained for each participant.
|
2.2. Preliminary Testing
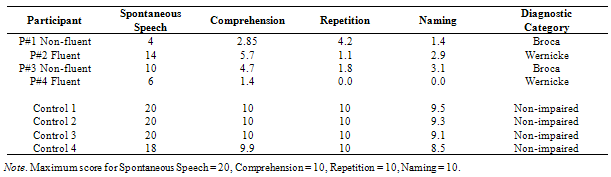
- The Western Aphasia Battery (WAB) (Kertesz, 1982) was administered to all participants. As expected, the non-imp- aired participants presented with language skills that were judged to be within normal limits. Individual scores from the WAB are presented in Table 2. All participants participated in a hearing screening and hearing was judged to be adequate for conversation.
2.3. Experimental Task
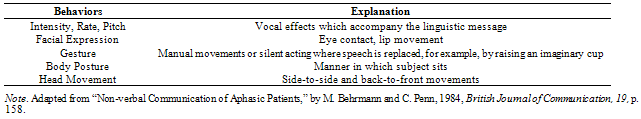
- The primary objective of the experimental task was to elicit a spontaneous communication sample that was representative of each participant’s ability to communicate regardless of modality. Therefore, it was necessary to embed this portion in such a way that the participants were not self-conscious or poised for the communication sample. Previous literature suggests that this is possible by first administering formal assessments and then suggesting that a "break" from testing be taken (Ripich, Vertes, Whitehouse, Fulton, & Ekelman, 1991).Each experimental session lasted approximately two hours and took place in a clinic treatment room with the participant and investigator seated across the table from one another. After the administration of the WAB and the hearing screening, each participant was told that it was time for a coffee break from testing. Coffee and a light snack were then offered to the participant. At this point, the investigator engaged the participant in a 20-30 minute informal conversation. Work history and illness were targeted for topics of conversation because they have been found to yield the most complex language (Glosser et al., 1988). Alternative conversational topics included information relating to recent activities and interests, recent life changes, education and family. The investigator attempted to keep the topics and the form of the conversations similar for all participants. However, the content of the conversations depended largely on the participant. All interactions were videotape recorded. The participant’s communication acts within fifty investigator communication acts after an initial two minute period of talking were used for analysis. The mode of communication was also analyzed. This included verbal, nonverbal, and combinations of verbal and nonverbal modes.
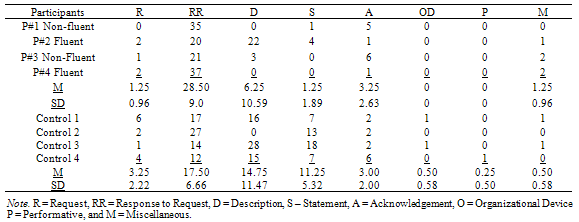
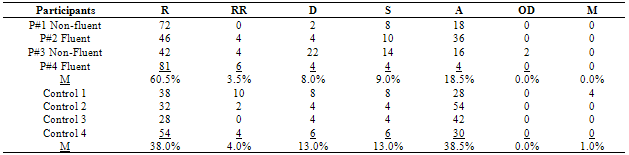
2.4. Data Analysis
- The choice for system of analysis was determined based on the communication categories used in previous research with adults (Doyle, Thompson, Oleyar, & Wambaugh, 1994; Gurland et al., 1982; Ripich et al., 1991; Wambaugh et al., 1991; Wilcox & Davis, 1977). Dore's (1978) Conversational Act Categories was chosen for the system of analysis because it included many of the same categories used in the above mentioned adult studies. The following communicative act categories were analyzed during the conversation (Dore, 1978): requests, responses to requests, descriptions, statements, acknowledgments, organizational devices, performatives, and miscellaneous.
|
|
2.5. Reliability
- For the purposes of intra-judge reliability of transcription, the primary investigator selected at random one language sample from each group of participants. The videos were viewed and discrepancies in transcription from the original transcripts were noted. The percent agreement for intra-reliability of the two randomly selected transcripts was 98%.For the purposes of inter-judge reliability of transcription, two language samples were selected at random from each group. A trained reviewer viewed the videotapes of the four samples and generated an independent transcription for each sample. The reviewer was then given the original transcriptions generated by the principal investigator and instructed to indicate any discrepancies between the transcriptions. The percent agreement for the four randomly selected transcripts was 89%. Points of disagreement were then identified and discussed, and agreement was reached on all points.For the purposes of intra-judge reliability of coding of communication acts, the primary investigator re-coded ten percent of a randomly selected portion of the communication acts for each of the eight participants. The percent agreement for this procedure was 97%.For the purposes of inter-judge reliability of coding, twenty-five percent of the communication acts from each of the eight original transcripts were randomly selected for re-coding by the trained reviewer. Point-to-point agreement was 98%. All points of disagreements were identified, the transcripts and videotapes were again viewed by the primary investigator and trained reviewer and, after discussion, agreement was reached on all points.
2.6. Results
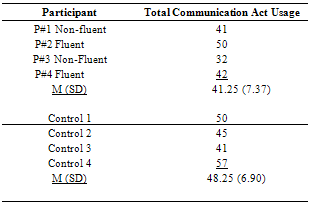
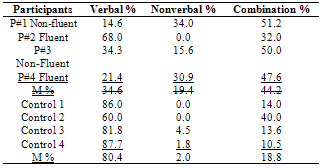
- Because of the small sample size parametric statistical analyses were not performed; however, individual and group means were analyzed to determine trends in communication act usage. As stated previously, the number of communication acts for each participant was tabulated. The mode of each communication act was classified as verbal, nonverbal or a combination of both and each communication act was coded using Dore's (1978) categories.
|
|
|
2.7. Discussion
- Clinicians are challenged with the task of identifying preserved language areas and using these areas as starting points for initiating treatment. If specific functions are to be targeted for treatment, consideration should be given to how frequently these functions are normally used in conversation. It is for this reason that identification of patterns of performance among individuals with aphasia is important. The present study sought to determine the number, mode of expression, and variety of communication acts used by participants with aphasia when compared to non-impaired participants during informal conversation. Visual inspection of the data revealed no apparent differences in the number of communication acts produced by the participants with aphasia when compared to the control participants. This finding lends support to research findings (Prutting & Kirchner, 1987) that individuals with aphasia are sensitive to the social and interactive rules of conversation.It was hypothesized that the participants with aphasia might use nonverbal strategies or a combination of verbal and nonverbal strategies to more effectively communicate a message. Results relating to mode of communication revealed an overall trend for the participants with aphasia to use more nonverbal strategies to communicate intent than the control participants. However, individual variability among the participants with aphasia was observed.
|
|
3. Conclusions
- Results of this research were that individuals with aphasia produce the same overall number of communication acts, although the variety of communication acts was restricted when compared to non-impaired individuals. Furthermore, consideration of nonverbal behaviors used by individuals with aphasia during communication did not influence the findings as expected. It is of interest to note that the scores of the participants with aphasia on the WAB did not necessarily predict which participants would communicate most effectively during the informal conversation. Further research is needed to explore whether the standardized functional communication measures that are available might be a better predictor of the communication act usage of individuals with aphasia. It is anticipated that further investigation into the pragmatic abilities of individuals with aphasia will lead to information which may enhance the design of assessment and therapy that target full-life participation for this population.Although the number of participants with aphasia included in this study was small, it appears that communication act usage may be related to severity of aphasic impairment and in particular, severity of verbal impairment. Further research is needed to explore performance profiles in both individuals with aphasia and non-impaired individuals. Although specific information obtained from this study does not contribute directly to the development of appropriate treatment strategies for individuals with aphasia, these findings suggest that there may be distinctions among some individuals with aphasia which deserve attention, and which may ultimately enhance the design of clinical treatment for specific patients, given further exploration.The idea of using a less impaired or relatively unaffected modality to strengthen an affected one is not a new one in the aphasia literature. It seems that the best way to implement this notion is to start providing opportunities in treatment sessions to produce a variety of communication acts. This does not mean to suggest that every treatment session should provide opportunities to communicate all possible intentions, for this is neither possible nor realistic. But rather, treatment should be structured so that the patient is allowed to intend more than a response to a clinician’s request.To understand how or whether clinical deficits affect communicative participation, analysis of larger segments of performance is necessary. These results suggest that the pragmatic aspects of language are closely linked to judgments of a perceived level of social competence. Our effectiveness as clinicians is judged, in part, by the impact our remediation efforts have on an individual's ability to function as a productive member of society (Kagan & Simmons-Mackie, 2007). In cases where only limited advancement in the structural aspects of language can be predicted, remediation of the pragmatic aspects of communication may contribute most to a level of social acceptability and participation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML