-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Frontiers in Science
p-ISSN: 2166-6083 e-ISSN: 2166-6113
2021; 11(1): 1-17
doi:10.5923/j.fs.20211101.01
Received: Jan. 28, 2021; Accepted: Feb. 24, 2021; Published: Mar. 6, 2021

A Dynamic Scientific Model for Recovery of Coronavirus Disease
Md. Rahimullah Miah1, AAM Shazzadur Rahman2, Alamgir Adil Samdany3, Shahriar Hussain Chowdhury4
1Department of Health Information Technology, Northeast Medical Pvt. Limited, Sylhet, Bangladesh
2Department of Medicine, Northeast Medical College, Sylhet, Bangladesh
3Department of Orthopedics, Northeast Medical College, Sylhet, Bangladesh
4Department of Dermatology, Northeast Medical College, Sylhet, Bangladesh
Correspondence to: Md. Rahimullah Miah, Department of Health Information Technology, Northeast Medical Pvt. Limited, Sylhet, Bangladesh.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Coronavirus is the most pressing scientific puzzle in the 21st century. This is a pandemic spreading globally through exploration of various wireless sensor networks. Yet Medical authorities are facing the obnoxious ever-increasing causes of coronavirus as a very global turning issue. Aims: The study aims to outline the scientific model for recovery of coronavirus disease with comprehensive follow-up and services. Methods: A dynamic scientific model was established in connection with recovery of coronavirus disease. This model identified the COVID-19 patients who need boosted follow up to recover with dynamic community cares. Sensor data were collected from the patient's profile, diagnosis and complication records at light and dark environments. Results: The study demonstrates total 150 patients suffered from coronavirus disease and stayed at home isolation within optical GPS locations. In a light environment, all patients recover from coronavirus disease due to wireless sensor network isolation, changing their GPS locations instantly with tightly closed eyes and wearing anti-radiation sunglasses, and also clothe with black uniforms in the whole body. The obese patients required long time to recover in dark environment in comparison with others. Replication: The findings replicate the coronavirus disease recovery for dynamic health security that the physicians provide on the priority of strategy, mental health service, innovations, potentiality and personalism. Conclusion: Scientific healthcare sensor knowledge is indispensable for recovery of coronavirus disease. The study reveals the implementation of sensor network approach to patients with coronavirus disease recognizing those with augmenting physical, technological and mental healthcare requirements. The study suggests future research trajectories of a new alternative sensor network isolation model to promote global public health security.
Keywords: Coronavirus, Sensor network, Obese, Environment, Model, Security
Cite this paper: Md. Rahimullah Miah, AAM Shazzadur Rahman, Alamgir Adil Samdany, Shahriar Hussain Chowdhury, A Dynamic Scientific Model for Recovery of Coronavirus Disease, Frontiers in Science, Vol. 11 No. 1, 2021, pp. 1-17. doi: 10.5923/j.fs.20211101.01.
Article Outline
1. Introduction
- Coronavirus disease is nothing but misapplication of wireless sensor networks surrounding optical geographic location. This is a non-communicable sensor disease spreading worldwide through misusing of fluctuated and processed wireless sensor networks [15]. Until now Medical authorities are facing the undesirable escalation of corona virus towards human beings as a very global comprehensive issue. Coronavirus disease is a pandemic global problem, which is the grittiest scientific puzzle in the history of the world [81]. Coronavirus is tarnished [1,2,3,4,5] in the universe as an effect with unknown sources. The virus infected several people at Wuhan Province in China on December 29, 2019 [6]. Then the number of people infected with the virus increased day by day and spread all over the world, and above 2 million deaths from the COVID-19 [7,85]. This new virus and disease were unknown before the outbreak began at Wuhan last year but till to date total confirmed total cases 92022539, total deaths 1970394 (3%) and recovered 65865510 (97%) [8]. The whole world is worried, anxious and scared in all spheres including social, economic and communication due to unwanted conditions of coronavirus [9]. The World Health Organization provides information and guidance online on the spread of the virus, as well as regular virtual conferences, meetings, press briefings and exchange of information [7]. COVID-19 or Coronavirus disease 2019 is affecting in 219 countries and territories around the world [8], [10] due to the presence of interconnected markets, complex emergencies, religious mass gatherings, variation in emergency healthcare systems performance within and between geographic landscape, seascape and skyscape [11,12,13].Wireless Sensor Network is an integrated infrastructure comprised of sensing, detecting, tracking, observing and reacting the individuals within geographic positioning systems (GPS) locations [14], which is deployed the indoors and outdoors in large sensor fields using object’s light and radio signal [13,15,16,17,18,19,20,21,22,23]. Active eyes act as a receptor in a light environment. Current and customary medical systems cannot meet the requirements of patient needs in a timely fashion due to cutting-edge sensor healthcare systems [24]. This technology is actually valuable in some healthcare applications, which can be inserted into the human body for treatment services [25,26,27]. The cutting-edge sensor technology misuses in different services including healthcare activities, which have triggered a collective capacity of scarcities and securities. Wearable health-monitoring provides a revolutionary sensor technology, which serves as an alternative to traditional diagnosis, putting healthcare data on a path that is more remote, portable, and timely [28,29,30,31]. Physicians and health researchers use these healthcare data to evaluate body conditions with a sensor technology like internet of everything, artificial intelligence, deep-learning algorithm [32,33,34]. Moreover, sensor cameras along with sensor technology has a great advantage on non-communicable diseases to identify the classical symptoms [14]. Wireless sensor networks are a huge endeavor of digital health technology, including technology dependence, which has led to frustration due to lack of proper security. Smartphones can do a lot of lucrative things with at least 12 functions with digital health sensor systems [35,36]. Cyber hackers misuse the radio frequency through smartphones, telematics and high frequency sensor devices for spreading this corona remote sensing VIRUS among animals and human beings, mostly coronavirus [15]. The present world is being one-sidedly mistreated sensor networks one after another from cyber hackers [15]. The heartbreaking phenomena of this frustration are the foremost consequence of today’s COVID-19 outbreaks in human beings [37].The aim of the study is to build a new scientific model with multiple innovative approaches to solve the core challenges in global health security to recover coronavirus disease in order to provide the justifiable policy options by the use of sensor technology.
2. Scientific Model Design
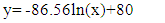
- This research method was conducted as PhD research work from October 2014 to May 2018 at the Universiti Malaysia Sarawak (UNIMAS), Malaysia. The materials and methods were connected with different parameters to enhance data collection, ISNAH Experiment [38]. According to ISNAH, the case study was conducted in different coronavirus disease recovery components, which are shown in Figure 1.
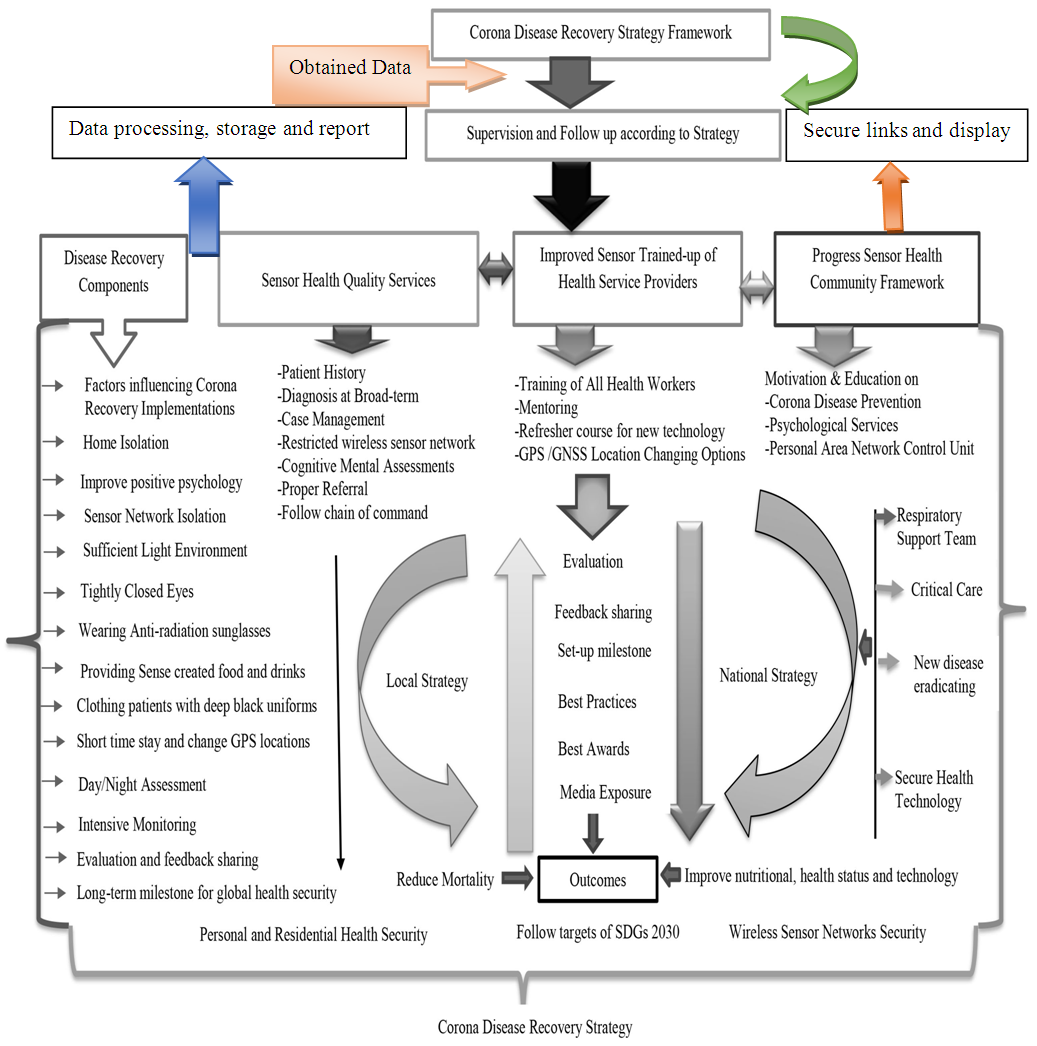 | Figure 1. Coronavirus Recovery Strategy Framework [111] |
3. Scientific Model Applications and Outcomes
- The study is a case study among 150 COVID patients. All patients were followed the ISNAH guidelines for recovery from coronavirus disease, which was stated in the recent published book “Cyber Dazzal: Barriers to Sound Health” [URL: https://www.rokomari.com/book/202988/cyber-dazzal---sushaysther-ontoray] and published article at volume 10, number 1 on title “Impact Sensor Technology Enhancing Coronavirus disease” at the American Journal of Biomedical Engineering in the year of 2020 in the URL (Uniform Resource Locator): http://article.sapub.org/10.5923.j.ajbe.20201001.03.html and volume 9, number 2 on the title “Impact of Sensor Networks towards Individuals Augmenting Causes of Diabetes” at the International Journal of Diabetes Research in the URL: http://article.sapub.org/10.5923.j.diabetes.20200902.02.html.All patients are recovered within the stipulated time and no deaths in coronavirus disease. The age gradations are randomly selected within 20-80 years old. The respondents are males and females, which is shown in Figure 2. The COVID patients were about 73% male and 27% females. The study provided them health tips and followed up regularly on their health status for three months. The experts monitor all patients intensively. The health experts inspired them for 80% of psychological awareness in sound health guidelines stated in the mentioned book and article. After three months, all respondents are sound health and free from sensor diseases in a light environment including coronavirus disease, heart attack, cancer, stroke, paralysis, numbness, back pain, chronic kidney disease, acute respiratory distress syndrome and diabetes [112]. etc. [Appendix-C]. But the overweight and obese patients took more time for disease recovery than normal and underweight patients.
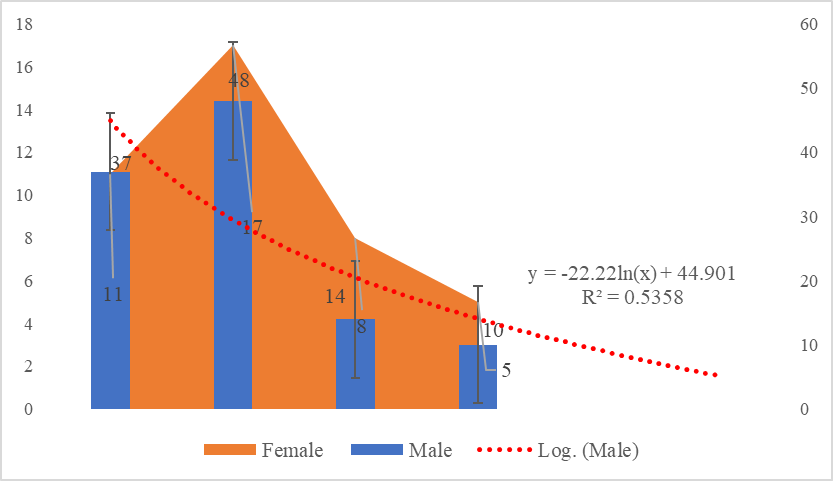 | Figure 2. Model Applications and Outcomes among male and female COVID patients |
 (a)
(a)
 (b)Where, y is the Model Outcomes among male and female patients and x is the Applications in affected patients in coronavirus disease at sufficient light environment. Equation (a) has an adjustment with equation (b) R2 (coefficient of multiple determinant of 0.5358 with standard error of estimate on observed value. The value of R2 is nearby 1, which indicated model outcomes between male and female patients. So, the stated equation is accepted on the priority of applicable parameters including real time, tightly closed eyes, soundless environment, controlled personal sensor networks and changing GPS locations towards patients.
(b)Where, y is the Model Outcomes among male and female patients and x is the Applications in affected patients in coronavirus disease at sufficient light environment. Equation (a) has an adjustment with equation (b) R2 (coefficient of multiple determinant of 0.5358 with standard error of estimate on observed value. The value of R2 is nearby 1, which indicated model outcomes between male and female patients. So, the stated equation is accepted on the priority of applicable parameters including real time, tightly closed eyes, soundless environment, controlled personal sensor networks and changing GPS locations towards patients. 3.1. COVID Recovery in Home Isolation
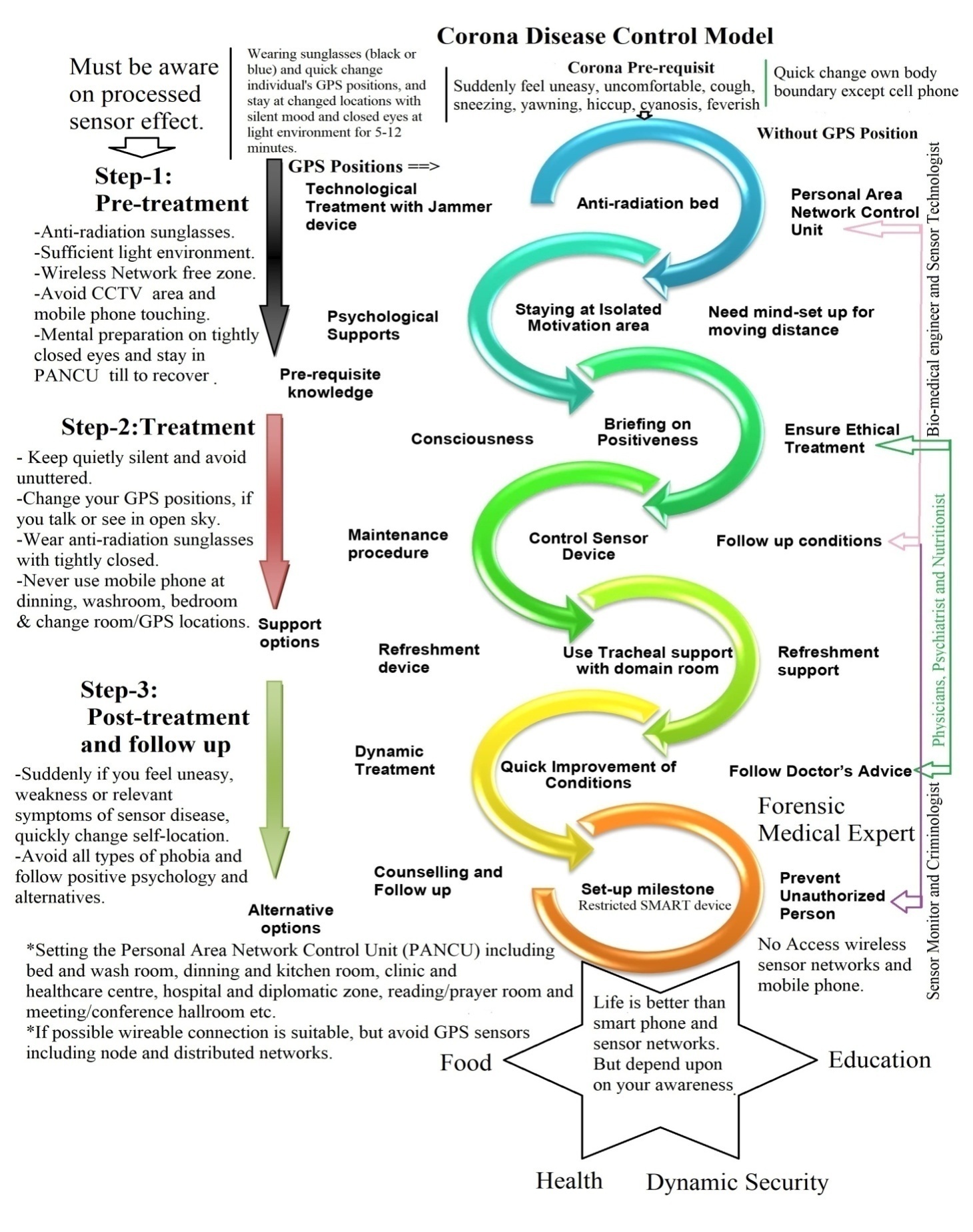
- The case study shows the COVID patients were recovered at home isolation with isolated wireless sensor networks, tightly closed eyes, wearing anti-radiation sunglasses and clothing black cloths due to reducing the processed sensor nodes from individual’s body organ at light environment and also clothed the patients with black uniforms through the whole body. Because, these components are reduced processed wireless sensor networks and created activeness in tightly closed eyes with GPS locations including longitude, latitude and ellipsoid height. The electron movement and blood transmission were easily improved than earlier conditions due to disconnect of wireless sensor networks. The age distribution among males and females’ patients varied in diversity, which as shown in Figure 3. Male patients followed the recovery instructions, sometimes they created gaps in intensive monitoring and remarkable follow up than female patients accordingly.
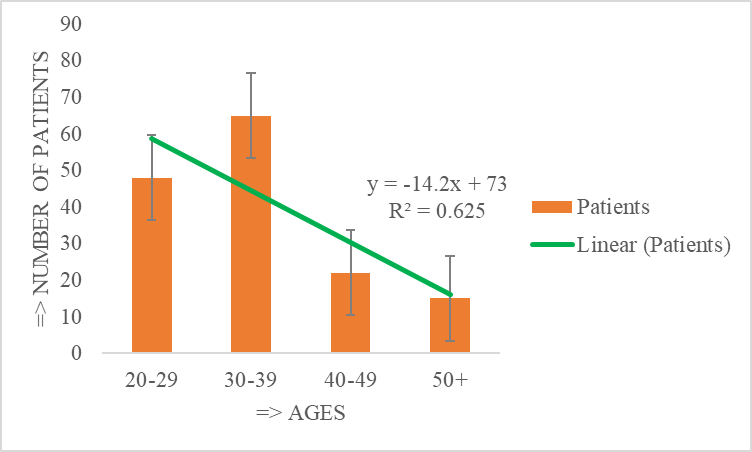 | Figure 3. COVID-19 Patients with age gradation |
 (i)
(i)
 (ii)Where, y is the recovery time on censored patient and x is the affected patient in coronavirus disease with overweight and obese, normal and underweight conditions of BMI at light environment. Equation (1) has an adjusted R2 (coefficient of multiple determinant of 1 with standard error of estimate on observed mean. The value of R2 is equivalent to 1, which indicated sensor time was recovered in patient’s mind satisfaction. So, the stated equation is accepted. The developed equation was then employed to stimulate human’s corona recovery consciousness regarding restricted wireless sensor networks with high frequencies towards underweight, normal and overweight in BMI status. If the value of R2 is negative, then the approaches between observed sensor time and simulated values recovered the coronavirus disease within stipulated times. For this reason, the stated linear equation is rejected. The existing sensor affected time will be accepted, if the value of “GPS distance” increases. The ISNAH approach will be accepted, if the value of overweight patients must be reached on >26 BMI and above.
(ii)Where, y is the recovery time on censored patient and x is the affected patient in coronavirus disease with overweight and obese, normal and underweight conditions of BMI at light environment. Equation (1) has an adjusted R2 (coefficient of multiple determinant of 1 with standard error of estimate on observed mean. The value of R2 is equivalent to 1, which indicated sensor time was recovered in patient’s mind satisfaction. So, the stated equation is accepted. The developed equation was then employed to stimulate human’s corona recovery consciousness regarding restricted wireless sensor networks with high frequencies towards underweight, normal and overweight in BMI status. If the value of R2 is negative, then the approaches between observed sensor time and simulated values recovered the coronavirus disease within stipulated times. For this reason, the stated linear equation is rejected. The existing sensor affected time will be accepted, if the value of “GPS distance” increases. The ISNAH approach will be accepted, if the value of overweight patients must be reached on >26 BMI and above. 3.2. COVID Recovery Mental Health Services
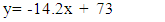
- From the study, COVID recovery services were applied 80% of psycho-technological and 20% of physical medicine, which was shown in Figure 4. The model works on COVID Recovery Administrative Isolated Wireless Sensor Networks for global public health and mental health services. The study illustrates all patients with coronavirus disease recover within 5-7 days to follow the disease recovery components. But the overweight and obese patients recover more than one week at light environment and 2-3 weeks at dark environment. The findings replicate the sensor disease recovery at local level in health security that the physicians provide worldwide.
 | Figure 4. The rate of COVID recovery in mental health services |
 (1)
(1)
 (2)Where, y is the rate of COVID recovery in mental health services and x is the affected patient in coronavirus disease with body mass indices at effective light conditions. Equation (1) has an adjustment with equation (2) R2 (coefficient of multiple determinant of 1 with standard error of estimate on observed value. The value of R2 is equivalent to 1, which indicated recovery rate was stated in psycho-technological and physical medicine. So, the stated equation is accepted on the priority of the patient's recovery. The developed equation was then employed to stimulate human’s corona recovery consciousness regarding the application of psycho-technological parameters and physical medicine with restricted wireless sensor networks.
(2)Where, y is the rate of COVID recovery in mental health services and x is the affected patient in coronavirus disease with body mass indices at effective light conditions. Equation (1) has an adjustment with equation (2) R2 (coefficient of multiple determinant of 1 with standard error of estimate on observed value. The value of R2 is equivalent to 1, which indicated recovery rate was stated in psycho-technological and physical medicine. So, the stated equation is accepted on the priority of the patient's recovery. The developed equation was then employed to stimulate human’s corona recovery consciousness regarding the application of psycho-technological parameters and physical medicine with restricted wireless sensor networks.4. Discussion
4.1. Model Reflection
- The findings reflect the importance in coronavirus disease management through treatment and recovery that the physicians provide, which recover due to restricted access wireless sensor networks, tightly closed eyes, change longitude/latitude and ellipsoid height instantly, wearing black uniform and sunglasses and stay in a light environment. In the dark environment, the obese people are more vulnerable than normal and underweight patient and they take more time to recover in light environment in all isolation period. Each sensory system has transformed tissue containing an array of fixated neurons to sense and transduce specific physical stimuli in optical sights [43]. Human eyes are the powerful natural close circuit camera, which focuses optical sight within GPS position. Through assimilating adaptive optics micro-stimulation with high-speed eye tracking, the retinal function can be explored at the level of the individual cone photoreceptor in active eyes [43]. The eye offers one exception to this situation, with the cornea and lens affording a view of the retina that is only obscured by imperfections in the optics. Recent advances in ocular imaging now make it possible to overcome these imperfections and image individual photoreceptors in the living retina [44]. The study assesses the scientific model for treatment and recovery from this coronavirus. Sensor data were collected from individual’s profile, diagnosis and sensor node records at laboratory experiments, where no death and all are recovered within 2-5 days in general. But overweight patients recovered in a longer time than in general. The case study was completed at four districts in Sylhet division of Bangladesh, viz. Sylhet, Sunamganj, Habiganj and Moulvibazar. There are some advantages of the dynamic scientific model, which are mentioned as follow:i. The scientific model can be applied to all patients in sensor diseases / CASID at local, national, regional and global levels [Appendix-C].ii. This model is appropriate in a wide variety of disease management and recovery.iii. It has low cost and ease to accommodate to all patients with sensor diseases / CASID.iv. It can be used in home isolation, small offices in connection with cognizance on non-communicable diseases.v. The model can be applied to health maintenance in organizations, single clinics, hospital-based care and private practice as well as large public health service centres/clinics.vi. The model can be applied to give recent developments in coronavirus disease related health education, nutrition, current treatment directions, future health security status.vii. The model can be applied to integrate the patient’s perspective, treatment preferences, and readiness to GPS location’s change within individual’s or integrated body boundary areas.viii. A useful dynamic model can be practiced anytime including prescriptive and predictive.ix. The model can advocate specific actions and options that can be taken to improve the sensor effectiveness and control, not just retrospectively explain events after they happen.x. It can address how a medical care system could use assessment information to tailor personalized interventions, based upon the uniqueness, situation, and desires of a novel sensor disease recovery.xi. The model is systematic, periodic, unique and free from all types of wireless sensor networks.xii. No need musk use during the implementation of this model towards animals and human beings.xiii. No restriction in handshake and social distance among each other’s body boundary area. xiv. The model is suitable in remote health services including rural and hilly area’s health systems.xv. No need to be a health expert but be aware of sensor effectiveness in real time and GPS locations.xvi. No restriction in physical distances for religious, cultural and meeting etc. activities.xvii. No need for physical distancing among each other during funeral activities of the body.xviii. In future, the model will be a lucrative and favorite for CASID research and health education management. xix. Finally, the model is not rigid and static, but can invite evaluation and be open to feedback, new data recovery, continual refinement and sharing to all.Overall, the scientific model reduces death from sensor disease in all countries of the world. Although, maximum deaths in some countries due to lack of dynamic sensor security, (a) The 389,621deaths from COVID-19 in USA, which is the highest in the world, (b) The 204,726 deaths in Brazil, which is the second ranking in the world, (c) The 151,564 deaths in India at third position in the world, and (d) The 135,682 deaths in Mexico at fourth ranking in the world [8]. General people can be aware from the study of this model, which is misused by cyber hackers. Cyber hackers scan the retina of the human eye with sensor technology to find out its current location and monitor every moment. The advantage of using decision support interlinks with wireless sensor network [47]. Recent progress in the use of biometric identifiers and simplified electronic medical record systems will mean that this is possible [48]. As a result, your location will be known immediately wherever you open your eyes at the country or international border and your activity will go to the sensor server along with the image. The sensor network has to adjust to your vision in the atmosphere. Cyber hackers spread the fake word in the media that he died after being attacked by Corona. Allah (The Creator) said in the Noble Quran as [87]: Evil (sins and disobedience of Allah, etc.) has appeared on land and sea because of what the hands of men have earned (by oppression and evil deeds, etc.), that Allah may make them taste a part of that which they have done, in order that they may return (by repenting to Allah, and begging His Pardon).
4.2. Treatment and Recovery
- COVID-19 is better cured in time and locations including diagnosis, treatment, prognosis, prediction and disease prevention. The research has shown that 80% of the disease needs to be treated through psychological and 20% through physical therapy and medicine. But the case study has performed 100% recovery from the application of scientific models at home and network isolations due to controlling recovery components. Controlling seven places for sustainable non-communicable disease management, this is to prevent the state-of-the-art of various aspects of wireless body area sensor network [54]. Moreover, the advice of a doctor experienced in medical sensors can be taken in this regard to advance the field of disease care [55]. If a person lives in a remote area where there is no regular registered doctor. Then he has to think of alternative arrangements. The sick person should wear sunglasses over his eyes, never sleep or stand in the dark, and drink regular lemon-ginger tea until he recovers. In addition, a teaspoon of lemon juice, a paracetamol (800 mg) and a glass of oral saline should be taken together. Regularly the person eats garlic, black cumin, neem leaf powder and honey together and changes his/her bed position from time to time for good health and is very careful in using a smartphone. Anti-radiation bed and mosquito net must be used in bedroom and facility-based care when it is needed [56]. The obese patients are risk in COVID-19 due to respiratory syndrome [88,89,90,91,92,93,94]. Designing of efficient biosensors for sensitive and selective measurement of specific biomarkers, is a significant step for the primary disease diagnosis, treatment, and management with emergency healthcare framework [45,46,53]. The whole world today is worried about the treatment of coronavirus disease (COVID-19). Because vaccines alone cannot cure corona completely. Moreover, the following coronavirus disease control model can enhance all for recovery from coronavirus disease, which is shown in Figure 5.
 | Figure 5. Dynamic Scientific Model for Recovery of Coronavirus disease |
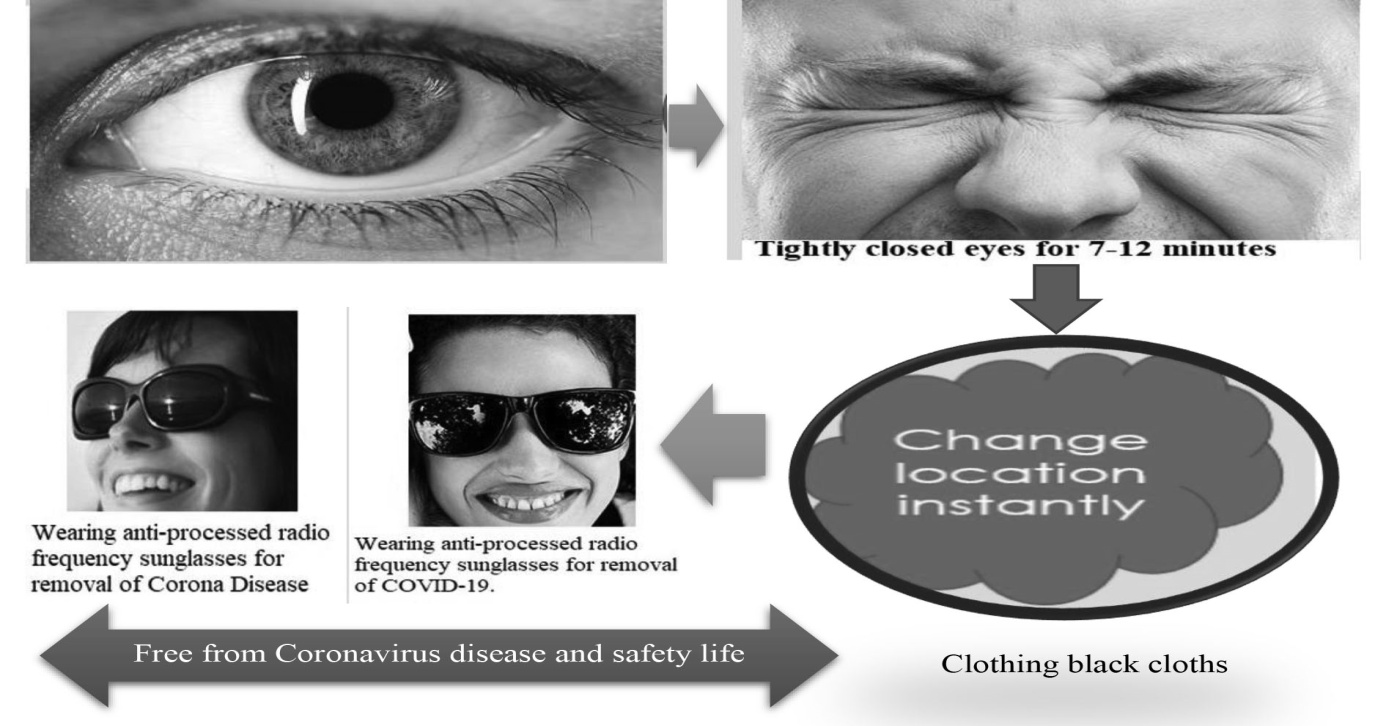 | Figure 6. Wearing anti-radiation sunglasses enhances free from CASID and safety life |
4.3. Performance in Management Model
- Corona virus is our learning with cutting-edge technology, which is continuing to advance on a dramatic impact on the science and engineering workforce [108]. This is the time to shift focus to efforts that support returning to manage and restarting operations according to requirement changes for the rationalized generations [104]. Global Coronavirus recovery (COVAX) is a global solution for COVID-19 treatment providing vaccines for controlling with effective testing and preventives measures [82]. Treatments give these tools to help patients to treat COVID-19 [83].Mask use is not recovered from coronavirus disease. Again, there is no relation between application of mask and corona recovery. But cyber hackers send messages to the main health administration for development of policy on mask applicability. Most health administrators have no idea on bouncing messages. As a result, they circulate policy to the security force. According to the rules and regulations, the security force monitors the general people. Public suffers from disease and punishment from cyber hackers and police respectively. Scientific healthcare knowledge is essential for treatment and recovery with medical sensor technological devices but such knowledge is poorly documented and relevant treatment supports are still below par. The study suggests future research trajectories of a new dynamic alternative model to promote global public health security concerning Sustainable Development Goals 2030, which was illustrated in Figure 7 on sensor disease management model.
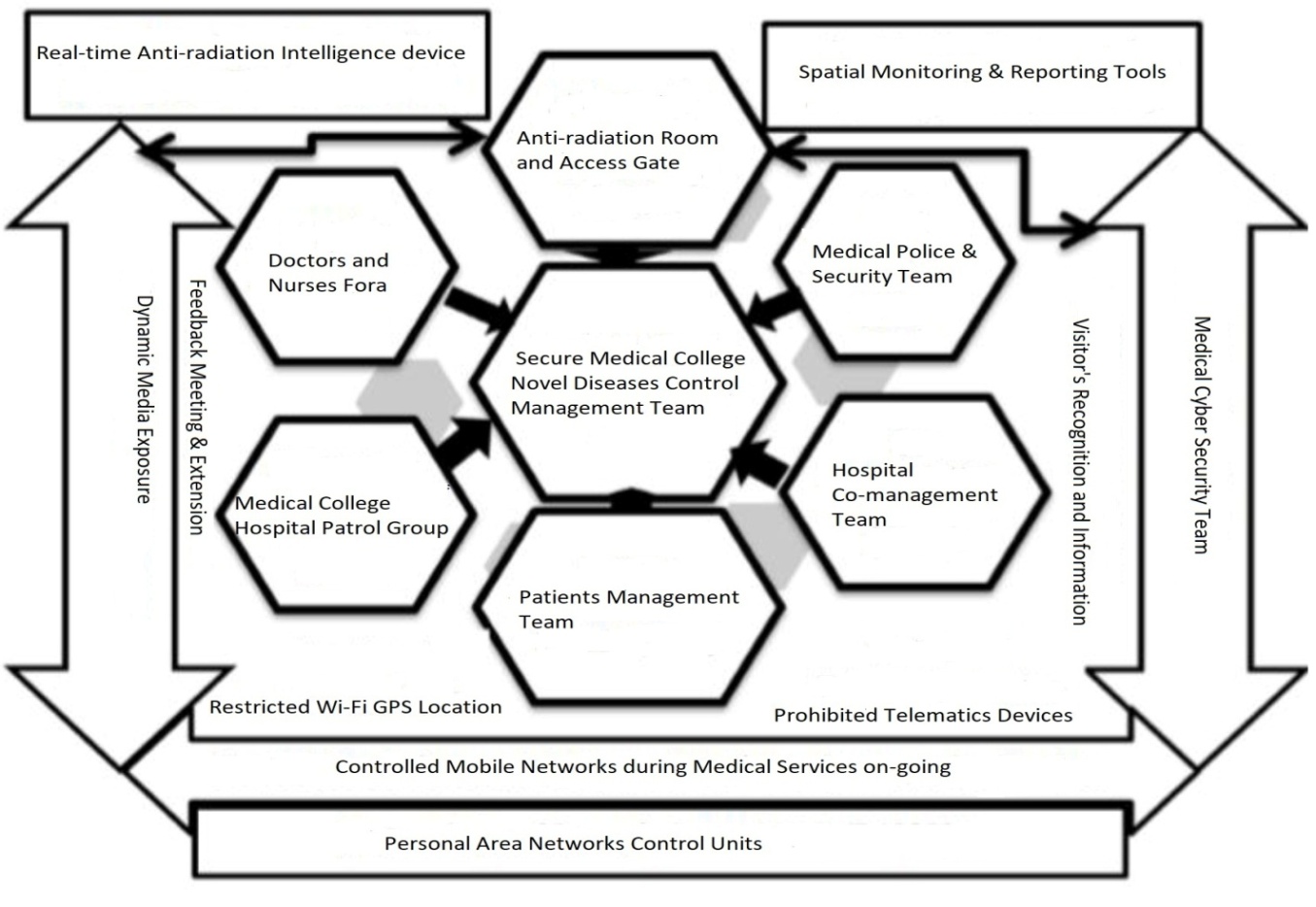 | Figure 7. Sensor Disease Management Model |
4.4. Innovations on Recovery
- COVID-19 recovery can innovate through technological science, medical science, crisis management interlinking with public and private sectors [105,109]. Innovation will have a significant tool to play in improving from the aftershock of coronavirus. There are some innovations to innovate from new scientific sensor model, such as:i. Quick sensor network affected towards man, animals, plants and objects within GPS body boundary areas.ii. Disseminate the distributed and node sensor networks to the whole network areas through individual or group wise.iii. Overweight and obese animals /human beings are more prone to be negatively affected by sensor telematic networks because of peripheral congested environment and splitting processed and fluctuated frequencies .iv. The radio frequencies of telematics ( above 500mHz to 999 mHz) were detected using Automated Radio Telemetry System and retina scanning within the optical sight distances. v. Exposure high RFID detects to die and damage the living and non-living objects less time in dark than light environment.vi. Treatment and recovery of the disease with setting PANCU and changing the object instantly from GPS locations.However, recovery from sensor disease, particularly COVID-19, the management rules can follow with anti-radiation parameters, such as black sunglasses, anti-radiation mosquito net and bed, which is shown in Figure 8.
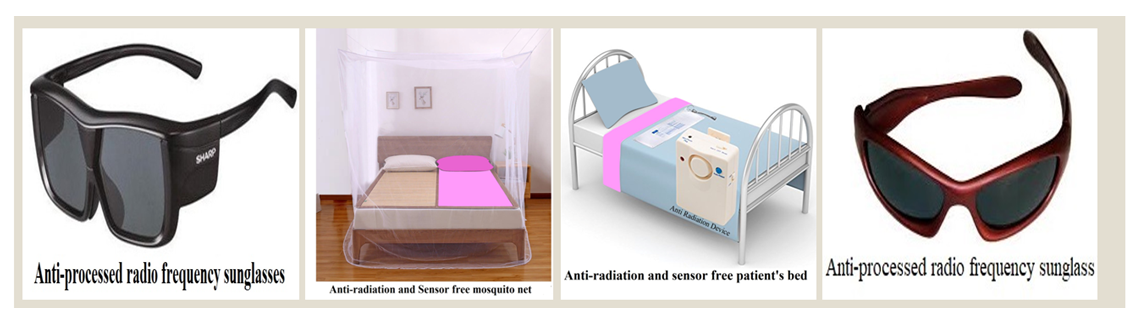 | Figure 8. Follow-up the anti-radiation processed radio frequency for secure life |
4.5. Potentiality for Future Directions
- The COVID-19 pandemic stances unique challenges in response and recovery trying to manage the shock in the face of existing societal threats like poverty, inequality, education and gender violence [106]. The Coronavirus has affected 71 million people in extreme poverty, 90% of students out of school and 30% gender violence [107]. From this scientific model, we achieve the following potentials to manage coronavirus disease, such as: ο It can enhance security systems for teachers, medical doctors, nurses, health officers, scientists, researchers, patients and other stakeholders, who have active open eyes or sensor devices.ο Experts have tried to implement ways of reducing this impact by encouraging pertinent institutions to go to a competitive market with dynamic treatment and recovery through alternative potentialities.ο Large potential on RFID technology uses including learning, research, servicing and access benefit sharing to achieve specific goals related to national health policy in connection with Sustainable Development Goals 2030.In the future, there is a lot of scope in wireless sensor networks in the world, which can be aware of the effect of it, as shown in Figure 9. People are at risk with wireless sensor networks, but human beings are attentive to manage their healthy life [95] for security. Health security capacity has become increasingly within the broader context of health systems [96]. Managing the global regime for controlling the international spread of infectious diseases is a central and historical responsibility of WHO [97]. State-of-the-art security frameworks have been extensively addressing security issues [98]. There is no consensus among analysts about the specific parameters of health security [99]. The world needs a stronger, more resilient framework for global health security [100]. Healthcare data has the highest potential for improving patient outcomes [101]. Global health security threats are increased through manmade [102]. COVID-19 outbreaks are the learnings that can avert the cost crises of social, political, economic and health systems [103]. The COVID-19 pandemic reflects in mental health services to staying at home and doing less in terms of social interactions and exercise with practical skills to help cope with stress [110].
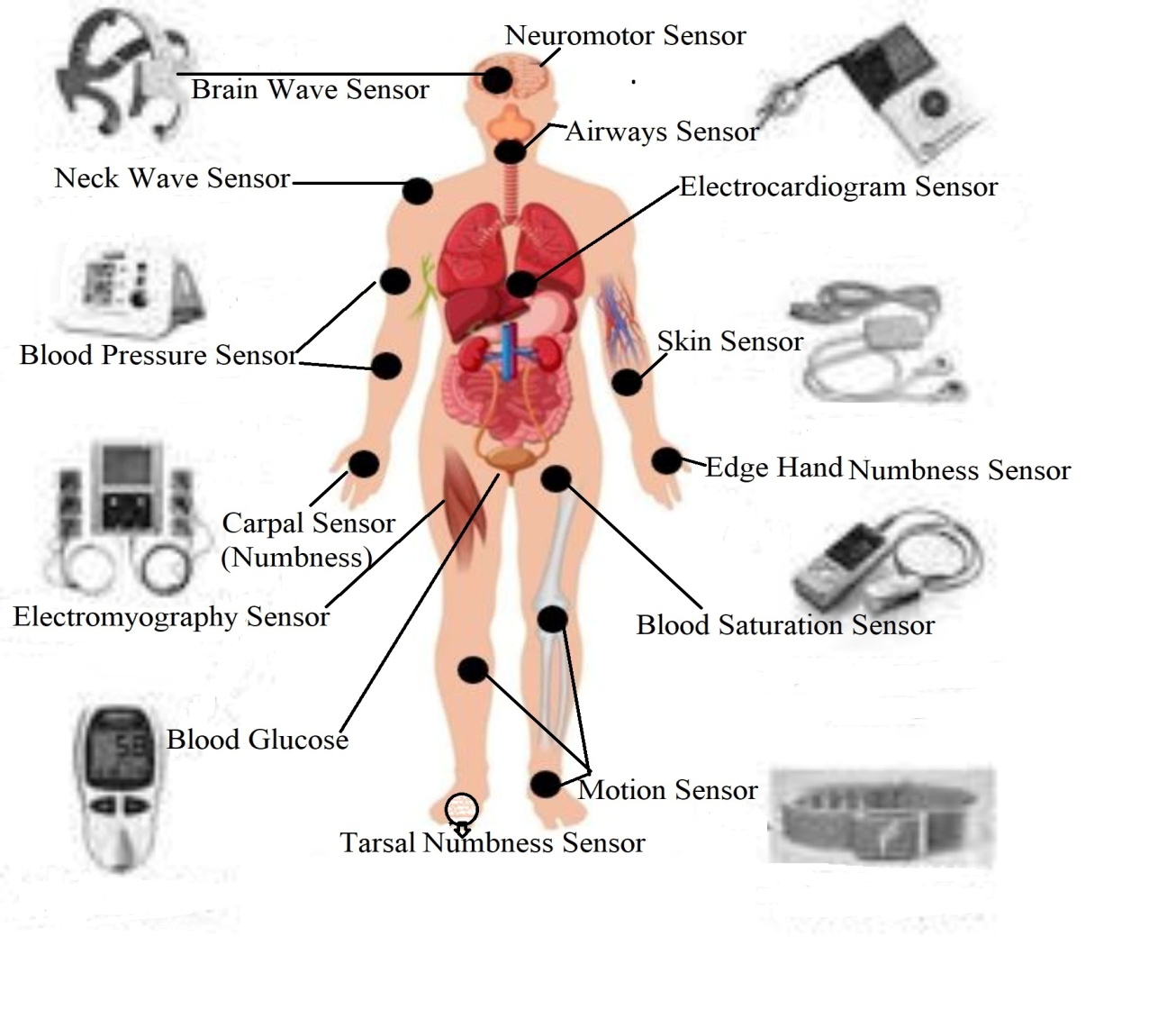 | Figure 9. Wireless Sensor Networks affect in the whole body producing different diseases |
4.6. Further Personalism Treatment
- Medical treatment is sensitive and integrated management in health services. Due to cutting-edge nano sensor technology the management of medication is not only for physicians but also recovery through the dynamic recovered actions of sensor experts. Further personalism of medical science can be shared with multidisciplinary sectors including sensor technology, advanced nutrition and herbal digitalization. So, doctor’s personalism is required to be flexible in treatment and recovery of CASID (Common Acute Sensor Infections and Disorders) [111]. The higher authority can allow them, who are interested in sensor health treatment by the physicians or sensor experts. For this purpose, the administration should restrict misapplication on sensor health activities including retina recognition, finger print, DNA sequencing and voice decoding etc.
4.7. Limitations in Implementation
- The major limitation is the stimulation of individual neurons is difficult when individuals sit within an array of similar receptors, with the array itself hidden inside a sensory organ [48]. False interface, bouncing message and voice are increasing through sensor technology due to lack of effective security [16]. Cyber hackers spread the fake information in the media that he died after being attacked by Coronavirus [16]. Despite the spread of information technology, it is very difficult to find the right antidote to cure coronavirus disease [56,57]. Many mobile phone users are not aware of the health security measures of sensor technology [58,59,60,61,62,63,64,65,66,67]. As a result, various non-communicable diseases including corona are increasing abnormally [15,61]. The research organization develops a set of recommendations for all countries to recover [54] corona with its challenges. The crowdsourcing data about providers, facilities, and health systems is likely to grow as more people with sensors are at risks [63]. Violence against healthcare technology providers has increased worldwide in the context of COVID-19 for challenging treatment with insecure technology [64,65,66]. Some people believe to reduce spread and deaths due to using facemasks, social distancing, and avoid handshaking [67]. But these are bouncing messages from cyber hackers sending to the higher authority, which are almost fake. Cyber hackers highlight scamming mails, voice calls and electronic news for media exposure as an infodemic with phobia formula accelerating negative psychology towards mass people [68,69,70,71,72,73,74,75,76,77,78,79,86] during the management of disease outbreaks as a global problem [81]. Moreover, COVID-19 treatment situation has not improved yet due to discriminatory nature of the existing health system [84]. The authority can ensure the effective physical and technological security in 15 locations including office room, wash room, bed room, dining place, meeting room, airport, bus stand etc.
5. Conclusions
- The study assessed the dynamic scientific model to recover coronavirus disease due to staying at home with isolated wireless sensor networks within GPS location including latitude, longitude and ellipsoid heights. Scientific healthcare sensor knowledge is indispensable for recovery of coronavirus disease. The study reveals the implementation of sensor network approach to patients with coronavirus disease recognizing those with augmenting physical, technological and mental healthcare requirements. Every State member of the United Nations should delete the retina scanning, DNA sequencing and fingerprint databases according to the National Sensor Health Policy and Sustainable Development Goals 2030. The study suggests future research trajectories of a new alternative sensor network isolation model to promote global public health security.
6. Declarations
6.1. Funding
- This research work ISNAH is a part of PhD Thesis, which was funded by the Zamalah Postgraduate Scholarship of UNIMAS, Malaysia and also sponsored by the Information and Communication Technology Division, Ministry of Posts, Telecommunication and Information Technology, Government of People’s Republic of Bangladesh. The funders had no role in the design of the research, in data collection, analyses or final interpretation of data, in the writings of the manuscript, or in the decision to publish the findings.
6.2. Data Availability
- The data being used to support the findings of this research work are available from the corresponding author upon request.
6.3. Competing Interests
- The authors declare no potential conflict of interests in this research work.
ACKNOWLEDGEMENTS
- The authors acknowledged the authority of Universiti of Malaysia Sarawak (UNIMAS), Malaysia for providing the Zamalah Postgraduate Scholarship for the completion of PhD degree. The authors are also grateful to the authority of the Information and Communication Technology Division, Ministry of Posts, Telecommunication and Information Technology, Government of People’s Republic of Bangladesh, for PhD Fellowship during the higher study in Malaysia. The authors acknowledged the authority of Northeast Medical College & Hospital (NEMCH) Pvt. Limited, Sylhet, Bangladesh for kind support.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML (Accessed Time on January 11, 2021 at 7:00 am).
(Accessed Time on January 11, 2021 at 7:00 am).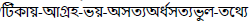 (Accessed time on January 16, 2021 at 8:00 am).
(Accessed time on January 16, 2021 at 8:00 am).