-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Food and Public Health
p-ISSN: 2162-9412 e-ISSN: 2162-8440
2021; 11(1): 24-34
doi:10.5923/j.fph.20211101.03
Received: May 21, 2021; Accepted: Jun. 5, 2021; Published: Jun. 26, 2021

Infant and Young Child Feeding Practices in Urban Areas in the Haut Sassandra Region (Côte d’Ivoire): Description and Nutritional Consequences
Dago A. Gnahé, Abba P. Obouayeba, Massé Diomandé, Koffi P. V. Niaba, Avit G. M. Beugré
Agrovalorisation Laboratory, Department of Biochemistry-Microbiology, Agroforestry Training and Research Unit, Université Jean Lorougnon Guédé, Daloa, Côte d’Ivoire
Correspondence to: Abba P. Obouayeba, Agrovalorisation Laboratory, Department of Biochemistry-Microbiology, Agroforestry Training and Research Unit, Université Jean Lorougnon Guédé, Daloa, Côte d’Ivoire.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The malnutrition of children remains a health problem in Côte d'Ivoire. In this context, a nutritional survey by questionnaire and anthropometric measures was carried out in the urban area in the Upper Sassandra region to nearly 419 children with an age of between 0 and 36 months in the city of Daloa. Describe the feeding of the infant and the young child through a nutritional survey and evaluate the nutritional status of children through anthropometries were the goals pursued in this study. The results show the average prevalence of chronic growth or malnutrition (7.32%). The skinny that reflects acute malnutrition affects only 16.92 percent of the children and is specific to the poor. As a result, some results obtained in the Court of Inquiry revealed that an exclusive breastfeeding of the birth to 6 months, and then a suitable supplement diet, are major factors in the nutritional status of Infants.
Keywords: Infants, Young child, Breastfeeding, Complementary feeding
Cite this paper: Dago A. Gnahé, Abba P. Obouayeba, Massé Diomandé, Koffi P. V. Niaba, Avit G. M. Beugré, Infant and Young Child Feeding Practices in Urban Areas in the Haut Sassandra Region (Côte d’Ivoire): Description and Nutritional Consequences, Food and Public Health, Vol. 11 No. 1, 2021, pp. 24-34. doi: 10.5923/j.fph.20211101.03.
Article Outline
1. Introduction
- According to the WHO, among children under 5, 52 million are wasted, 17 million are severely wasted and 133 million are stunted, while 41 million are overweight or obese in Africa. Stunting or chronic malnutrition has spread in Côte d'Ivoire, among children under 5 years old. The prevalence of stunting is considered serious at the national level compared to an acceptability rate of 20%. From 34% [1] in 2006 according to NCHS standards, it rose to 29.8% [1] in 2012 according to WHO standards. Despite a downward trend in all regions, rates remain at the critical threshold of 40 % in the far north and west. At the level of children, this growth retardation is due to maternal undernutrition and an unsuitable feeding practice.It is well recognized that the period between birth and the age of 2 years is a critical period for the promotion of optimal growth, health and development of the child [2]. Globally, 60% of infant and young child deaths occur due to inappropriate infant feeding practices and infectious diseases, two-thirds of which are attributable to inadequate breastfeeding practices [3]. Infants and young children are particularly very fragile and vulnerable during their feeding. Indeed, feeding practices are very important and should not be neglected because it is at these times that the child can contract infectious diseases. Infant and young child feeding practices relate to a series of behaviors that the mother develops. These practices include the method and duration of breastfeeding, the choice of different types of complementary foods, the ages of introduction or cessation of various practices and the quantities served. These practices are of fundamental importance for the survival and harmonious development of children [4]. In several countries, nutritional problems in infants and young children are strongly linked to complementary feeding practices. In Côte d’Ivoire, 20.5% of the population in 2014 did not meet the minimum level of calorie intake and the diet remained undiversified in all age groups. The average calorie intake per capita is 2534 kcal / person / day compared to 2806 kcal / person / day recommended by WHO. The diet is generally not very diverse. In 2012, only 7% of children and infants received a diet of minimum quality both in terms of diversity and frequency of meals. This implies that IC supply practices are unsuitable [5].However, it is clear that malnutrition was responsible for 60% of the 10.9 million annual deaths of children under five [6]. Well over two-thirds of these deaths often associated with inappropriate feeding practices. Also, no more than 35% of infants worldwide benefit from exclusive breastfeeding during the first four months. Complementary feeding often starts too early or too late, and foods are often nutritionally inadequate. In addition, malnourished children who survive are more often ill and suffer the consequences of disrupted development all their lives. Another source of serious concern is the growing incidence of overweight and obesity in children [6]. Improper feeding practices are among the most serious barriers preventing this age group from achieving and maintaining satisfactory health. As a result, many infants and young children suffer from malnutrition [7]. Faced with all these problems; awareness raising on exclusive breastfeeding of infants up to the age of 5 months is desired in order to eradicate this malnutrition. However, it is advisable to combine breastfeeding with complementary foods for children from 6 months of age [8]. However, this practice can cause nutritional problems. The general objective of our work is to describe the feeding of infants and young children in urban areas in the Haut-Sassandra region, and to identify the nutritional consequences. More specifically we will: describe the feeding practices of infants and young children through a nutritional survey and establish their nutritional status by means of anthropometry.
2. Materials and Methods
- Target population (Child 0-36 months)This study took place from July 8 to September 8, 2020 at the PMI (Protection Maternel et Infantile) in Daloa and focused on the anthropometric parameters of infants (0 to 12 months) and young children (12 to 36 months).Technical materialThe technical material used to carry out this study consists of: A survey sheet containing a multiple choice questionnaire a notebook for recording additional information not appearing on the survey sheet; writing boards (Bic and pencils) and eraser; a plastic tape measure to take the child's head circumference; a tape measure to take the child's MUAC.The different instruments used to conduct this study are:
 | Figure 1. Photograph showing an instrument for measuring the cranial perimeter (tape measure) |
 | Figure 2. Photograph showing an MUAC measuring instrument |
|
|
3. Results
3.1. Results of the Nutritional Survey
3.1.1. Characteristic of the Studied Population
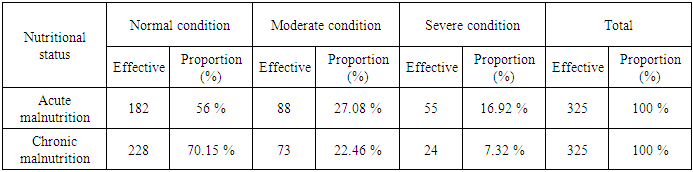
- The population of children surveyed was made up of 179 girls, or 42.72% against 240 boys, or 57.27% (Figure 3). During the survey, of the parents surveyed 21.72% were single versus 24.58% married and 15.99% widowed (Figure 4). Also with the age groups obtained, the age group [0-5] months included 50% of children with 19% of girls and 31% of boys; [6-11] months was composed of 21.24% children with 11% girls and 10% boys and the age group [12-36] months included 28.16% children with 13% of girls and 16% boys (Figure 5) and (Figure 6).
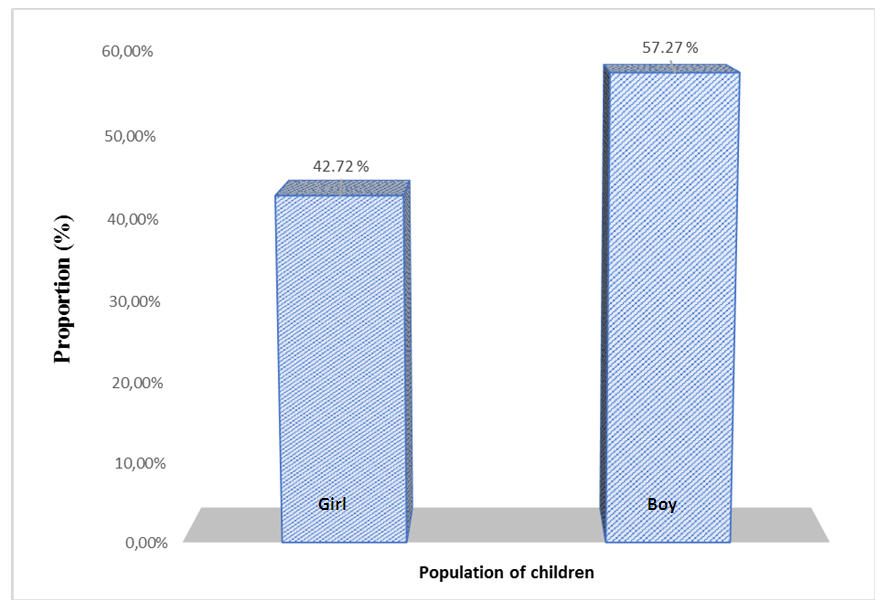 | Figure 3. Distribution of children by sex |
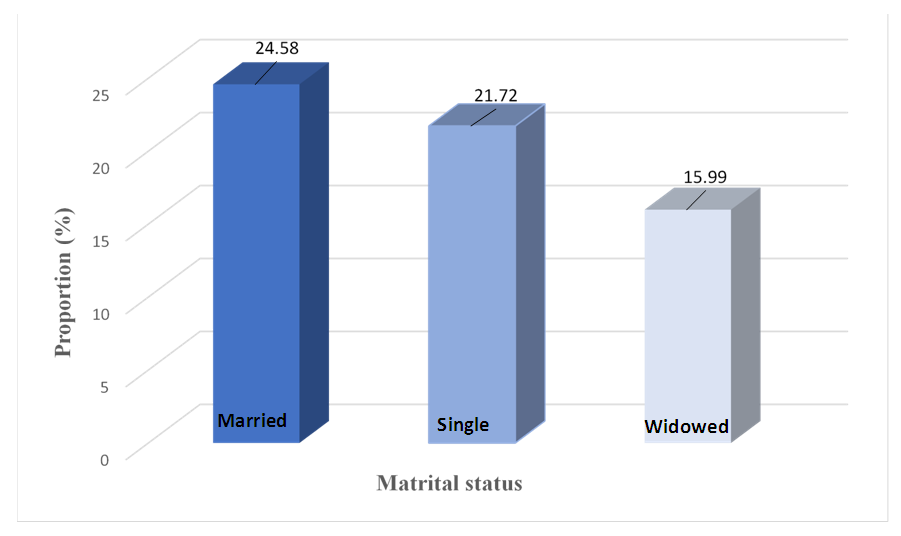 | Figure 4. Breakdown of parents surveyed according to their marital status |
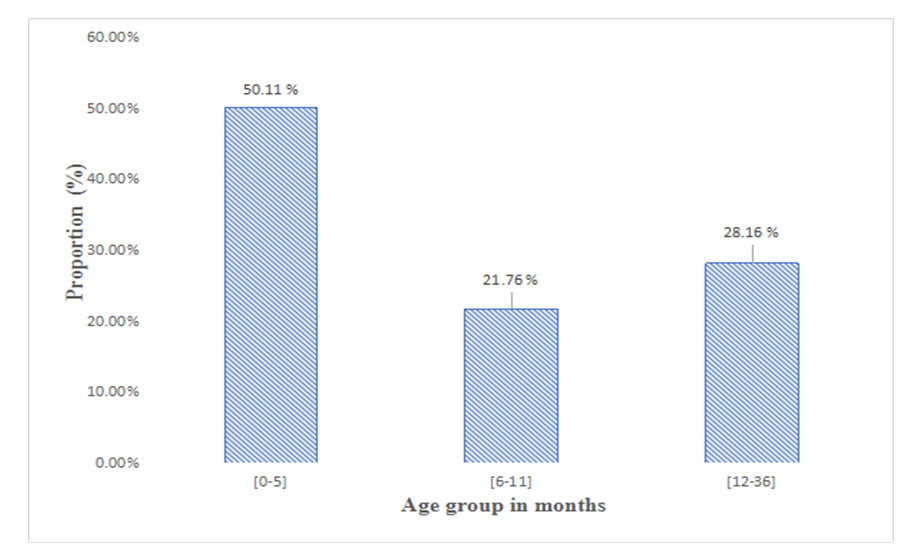 | Figure 5. Distribution of children by age group |
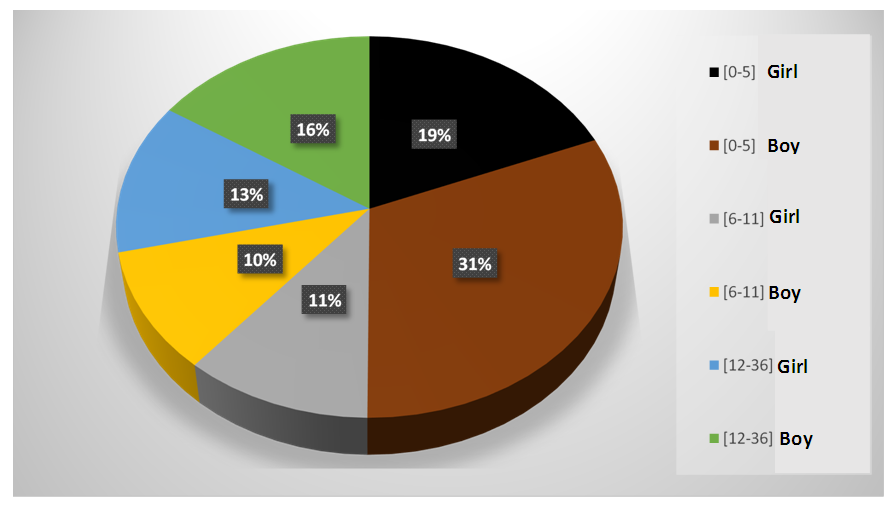 | Figure 6. Distribution of children by sex according to their age group |
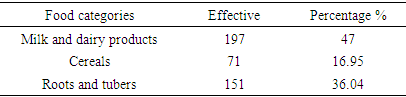
3.1.2. Categories of Foods Consumed by Children
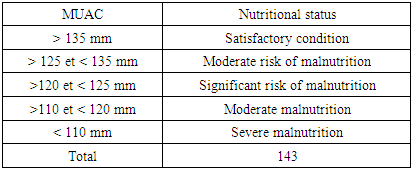
- The study showed that 47% of children consume milk and dairy products; 16.95% consume cereals and 36.04% of children consume roots and tubers (Table 3).
|
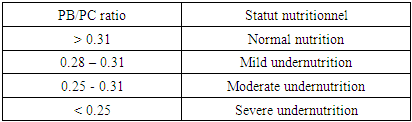
3.1.3. Types of Foods Eaten by Children
- The study showed that 19.09% of children consume breast milk; 8.35% consume drugstore milk; 13.13% consume rice; 0.47% consume cassava; 4.05% eat the sweet potato; 31.03% consume sweet potato; 10.02% consume others; 7.16% consume maize and 6.68% for millet (Table 4).
|
3.1.4. Diet of Children According to Their Age
- The survey showed that in the age group [0-5] months, 80% of children consume the predominant breast against 18% for the exclusive breast, 2% for the porridge alone and 10% for the complementary food (AC) other than porridge. In the age group [6-11] months 45% of the children took the predominant breast compared to 5% for the exclusive breast, 30% for the porridge alone and 20% for the non-porridge CA. In the age group [12-36] months 5% of the infants took the predominantly breast versus 70% not breastfed, 20% consumed CA other than porridge and 5% took the porridge alone (Figure 7).
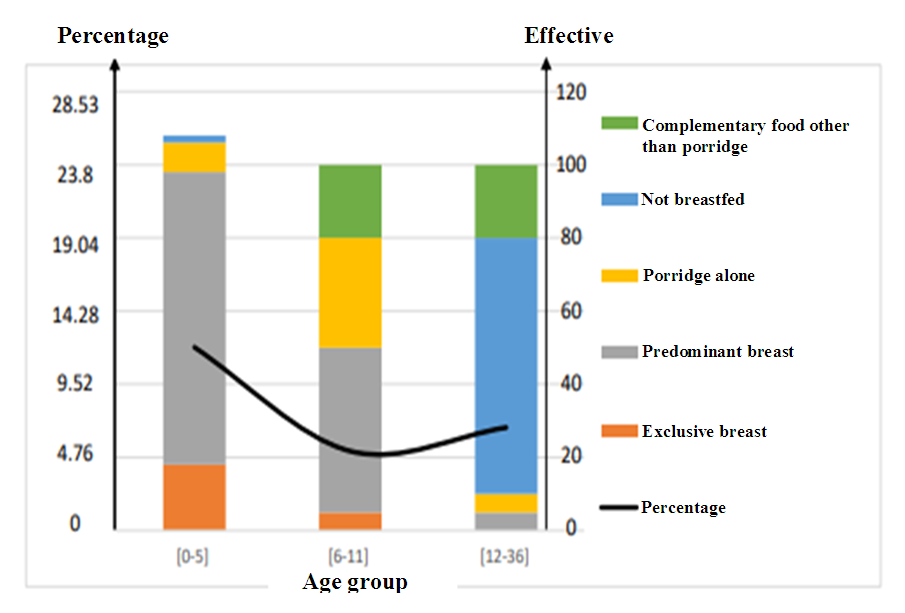 | Figure 7. Feeding method of children according to their age [0-36] months |
3.1.5. Types of Complementary Foods Consumed by Children
- The study showed that 13.84% of children consumed pharmacy milk (cow's milk) against 46.30% who consumed porridge, also 24.34% who consumed mash and 15.5% of other foods (Figure 8).
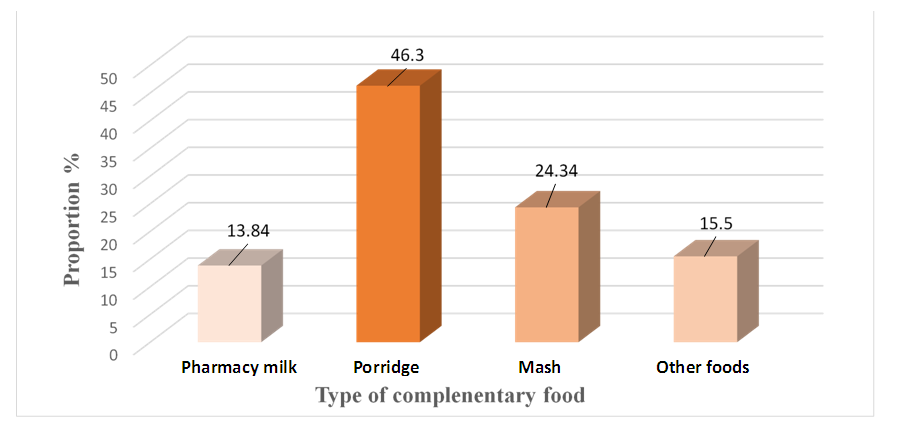 | Figure 8. Supplementary foods consumed by children |
3.1.6. Age of Food Diversification
- The study showed that 55.34% of mothers think that the specific age for food diversification is less than 6 months against 32.22% who think that 6 months is the perfect age and 12.41% think the opposite (Figure 9).
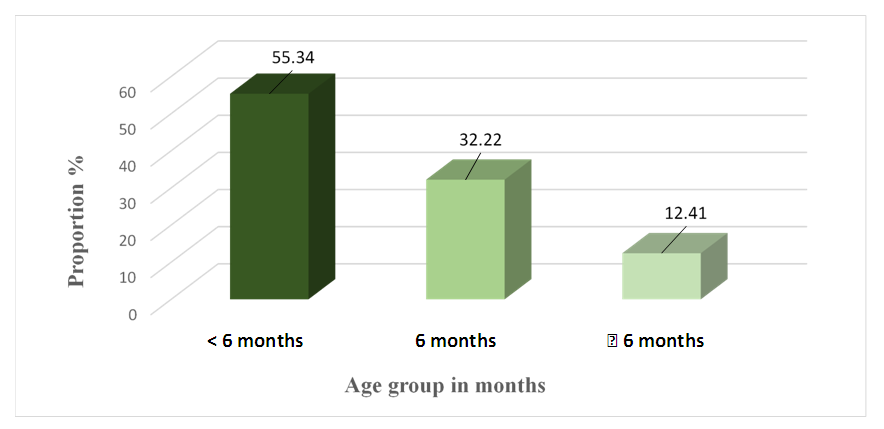 | Figure 9. Age of introduction of supplement foods |
3.2. Results of the Anthropometric Survey
3.2.1. Evolution of the Anthropometric Parameters of the Children Surveyed
- The survey showed that anthropometric parameters like MUAC and CP change in the same way in children from 0 to 36 months. In fact, MUAC and CP in children [0-6] months old is practically the same as MUAC and PC in children [7-12] months up to 36 months (Figure 10).
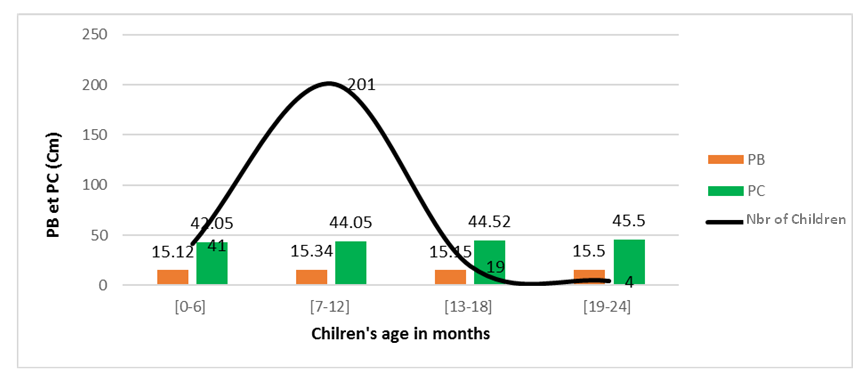 | Figure 10. Evolution of MUAC and CP in children according to their age |
3.2.2. Evolution of the Anthropometric Indices of the Children Surveyed According to Their Age
- The study conducted showed that PB/A, PC/A change with the age of the child (Figure 11).
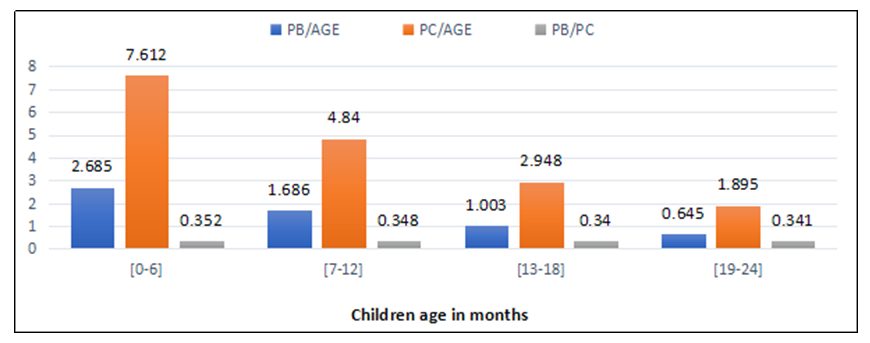 | Figure 11. Evolution of BP/A, PC/A depending on the age of the children |
3.2.2.1. Evolution of the MUAC/CP of the Children Surveyed
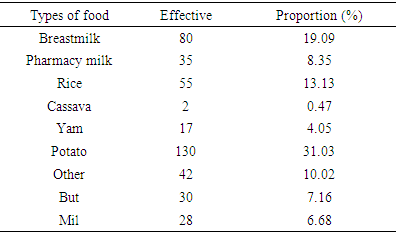
- The survey showed that the MUAC/CP of children 0-6 months was 0.35% compared to 0.34% for children 7-24 months (Figure 12).
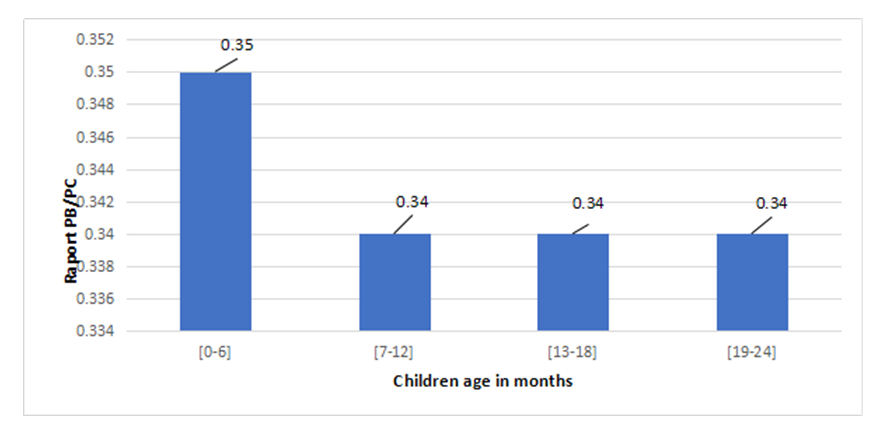 | Figure 12. Percentage of PB/CP of children surveyed |
3.2.2.2. Assessment of the Nutritional Status of the Children Surveyed
- This study revealed that acute malnutrition affects 44% of children aged 0 to 36 months living in the Haut Sassandra region with 16.92% being in severe condition. Indeed, 29.78% of children from 0 to 36 months suffer from chronic malnutrition with 7.38% being in a severe state (Table 5).
|
4. Discussion
- This study was carried out to describe the diet of children from 0 to 36 months in urban areas in the Haut Sassandra region, by identifying the nutritional problems associated with it in order to fight against malnutrition.The study showed that the number of boys was higher than that of girls with a sex ratio of 1.34. On the other hand, a study carried out in 2016 on the nutritional situation of the country indicated that the number of boys was higher than that of girls with a sex ratio greater than 1. In addition, boys would be more affected than girls, with respectively lower rates. prevalence of stunting of 33% and 27% [13]. Regarding the marital status of the parents questioned during the survey, the study showed that the mothers at greater risk who do not comply with the recommendations on feeding practices for infants and young children are single mothers, widows and those who have a low level of education. These mothers generally have financial problems that prevent them from adequately meeting the needs of their children but also have little information on good feeding practices for their children. This analysis joins that of Health Canada, [14] on the principles and recommendations for infant feeding from birth to six months. On the other hand, women who respect the recommendations of good dietary practices are those who are married, who are of a high intellectual level [15] and a stable socio-economic situation [16]. Indeed, the diet of the children surveyed was based on three (3) main food categories and among these foods, milk and dairy product were the most consumed by children with a percentage of 47%, followed by roots and tubers (36.04%) and cereals were consumed with a percentage of 16.95% of the children surveyed. The results of a survey carried out in 2004 showed that meals generally consist of a very simple base (cereals, tubers or plantains) accompanied by a sauce [17]. Regarding the types of food consumed by children, potatoes, breast milk and rice were the most consumed with a respective rate of 31.03%; 19.09 % and 13.13% because it is these types of foods that are more available in urban areas, so they are appreciated by children. This was refuted by a study which had shown that across the country, the cereals consumed are mainly maize (consumed by 71% of children in urban areas and 79% of children in rural areas), rice, sorghum. and millet [18]. With regard to the feeding method of the children surveyed, we note with satisfaction that breastfeeding in general is in the first month with a percentage of 50.11% and which continues until the age of 1 or even 2 years. The average duration of breastfeeding in our sample is greater than that observed nationally [19]. However, it is not known whether this long duration is a positive element, as some people have observed in Burkina Faso, where prolonged breastfeeding was associated with better nutritional status [20], or whether it is This is a phenomenon of reverse causality, breastfeeding being prolonged by mothers, children are malnourished [21]. Before the age of 6 months, exclusive breastfeeding is weakly practiced in Daloa. This rate is nevertheless higher than that observed in Sub-Saharan Africa in general [22]. It is also 4 times higher than that recorded nationally. In all of the children surveyed, complementary foods are often introduced after the recommended age and later than in other parts of Africa in general [22]. Porridge is not always offered to children and, in view of their composition, they can be judged of poor nutritional quality. It is well recognized that more often in developing countries, porridges lack protein, fat, micronutrient sources and are low in energy densities compared to recommendations [23]. With such a density it would be necessary for a young boy of 6 months to consume 4 porridges per day to supplement the energy contributions of the mother's milk [24].The description of the feeding practices of children from 0 to 36 months in the Haut Sassandra region revealed that 46.30% of children consume porridge as a complementary food to breast milk against 24.34% who consume mash. The others used at 15.5% and 13.84%. Of these supplement foods, porridge was the most common food consumed by children, the survey noted. Several foods were introduced into their diet before the age of 6 months: water, porridge and fruit juices [25-26]. It is true that porridge is the most consumed food, but its frequency of daily consumption is low because most of the children surveyed did not consume it more than 2 to 3 times a day, but this frequency of daily consumption cannot therefore be covering the nutritional needs of young children. These results are in agreement with those of [27] and [28] who found that local porridge is used at 64%, with a low frequency of daily consumption. This practice is due to mothers who lack information on good complementary feeding practices. Regarding the age of introduction of supplement foods 55.34% of mothers report that supplement foods can be introduced before six months. This knowledge is not in line with WHO recommendations that complementary foods should not be introduced into the diet of young children until 6 months of age [29]. This high proportion of mothers with inadequate knowledge about the age of introduction of complementary foods could be explained by a lack of nutrition education. It clearly appears that such a situation cannot help the proper management of complementary feeding.Regarding the anthropometric survey, the nutritional status of the children surveyed was assessed through anthropometric parameters (MUAC and head circumference). The study showed that the MUAC of most of the children surveyed (325) of the different age groups [0-24] months had a stable state of health (satisfactory nutritional status), since the measurement of their MUAC was greater than 135 mm or 13.5 cm which meets the standard. As for the cranial perimeter, the different age groups met the standards [29]. Indeed, the measurement of the cranial perimeter of children between 0 and 2 years old oscillated between 43 and 48 cm, which is recommended for children of this age group and which shows that their state of health is satisfactory. Indeed, the assessment of the nutritional status of children from 0 to 2 years old shows that the majority of children had a normal nutritional status since the MUAC to cranial perimeter (MUAC/PC) ratio was in the majority of cases greater than 0.31 cm [30]. Also The measurement of MUAC on age (MUAC / A) was consistent with the standard prescribed by [30], the standard having shown that children in normal nutritional status were those whose MUAC was equal to or greater 115mm or 11.5cm. Measurement of head circumference for age (PC/A) showed that the children did not suffer from microcephaly or macrocephaly because the head circumference observed in these children was between prescribed (2 > Normal < 98) in according to [30]. The anthropometric parameters studied clearly showed that only a small part of these children had problems of acute malnutrition and severe chronic malnutrition. Severe chronic malnutrition. Malnutrition therefore exists, but in low prevalence and spreads especially in poor socio-economic and marital conditions. This analysis is joined to that carried out by [31] on the assessment of the nutritional status of children in the town of Sati, which showed using anthropometric parameters that the prevalence of malnutrition in the town of Safi was weak but grew up with the poor living conditions of the families.
5. Conclusions
- The general objective of this study is to provide a description of infant and young child feeding in urban areas in the Haut Sassandra region and to identify the problems that are potentially associated with it. Through a nutritional survey, we showed that children's feeding practices were more based on the consumption of predominant and exclusive breast milk. Food diversification took place gradually from 6 months and was marked by the presence of complementary food such as porridge (46.3%); puree (24.34%); cow's milk (13.84%) and others (OPV, fruits and vegetables, fruit juice). Also, the study of anthropometric parameters showed that the majority of children observed had a good nutritional status even if the malnutrition was mainly due to the poor socio-economic and marital status of the parents. In short, it emerges from this work that feeding practices are functions of age groups and that the nutritional status of infants and young children is influenced by the different feeding practices of children which are themselves functions of socio-economic and educational conditions. and marital status of the parents. It is therefore up to children's institutions such as the PMI to conduct awareness campaigns to encourage parents to adopt good dietary practices for their children, but above all to explain to them the risks associated with bad practice.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML