-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Food and Public Health
p-ISSN: 2162-9412 e-ISSN: 2162-8440
2019; 9(3): 94-101
doi:10.5923/j.fph.20190903.03

Factors Associated with Adherence to Iron-Folic Acid Supplementation among Pregnant Women Attending ANC Clinic North Shewa Health Institution, Ethiopia 2016
Asnakech Sisay1, Nitsubirhan Asres2, Mikyas Arega1
1Department of Midwifery, Institute of Medicine and Health Science, Debre Birhan University, Debre Birhan City, Ethiopia
2Department of Nursing, School of Nursing, Kotebe Metropolitan University, Addis Ababa City, Ethiopia
Correspondence to: Asnakech Sisay, Department of Midwifery, Institute of Medicine and Health Science, Debre Birhan University, Debre Birhan City, Ethiopia.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

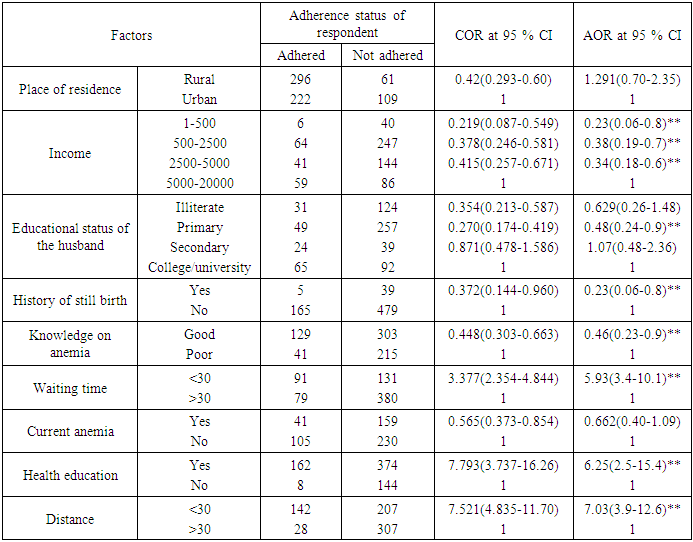
Background:- Anemia is a global public health problem affecting both developing and developed countries with major consequences for human health as well as social and economic development. It occurs at all stages of the life cycle, but is more prevalent in pregnant women and young children. Iron deficiency anemia (IDA) was considered to be among the most important contributing factors to the global burden of disease and folic acid deficiency is also the major contributing factor for congenital anomalies. Objective:-To assess the factors associated with adherence to iron-folic acid supplementation among pregnant women attending ANC clinic in selected governmental health institution, North shewa, Ethiopia 2016. Methodology: - Institutional based cross sectional study design was employed. On this study 693 respondents was participated. Data was collected using interview pre-tested and semi structured questionnaire of Amharic version. The data was cleaned, coded and entered into EPi info versions 3.1 and transferred to SPSS version 21 windows for analyses. Both Bivariate and multivariate logistic regression analysis was carried out to see significant association. Result: - It was intended to distribute 702 targeted sample questionnaires of this 693 were completed and returned with a response rate of (98.7%). Pregnant women who had less than 30 min waiting time were 5.93 times more likely to be adhered to IFAS than who take greater than 30 min in health facility (AOR=5.93, 95% CI: 3.4-10.1). Pregnant women who take health education were 6.25(2.5-15.4) times more likely to be adhered to IFAS than who didn’t take health education (AOR=6.25, 95% CI: 2.5-15.4). Conclusion: - This study show that only 25% of the pregnant women were adhered to iron folic acid supplementation. Recommendation: - Sensitization of pregnant women by health providers is very important to continue supplements of iron and folate throughout pregnancy. Provision of health education on anemia and importance of FANC are necessary.
Keywords: Maternal Anemia, Adherence, Iron/folate Supplement, Pregnant women
Cite this paper: Asnakech Sisay, Nitsubirhan Asres, Mikyas Arega, Factors Associated with Adherence to Iron-Folic Acid Supplementation among Pregnant Women Attending ANC Clinic North Shewa Health Institution, Ethiopia 2016, Food and Public Health, Vol. 9 No. 3, 2019, pp. 94-101. doi: 10.5923/j.fph.20190903.03.
Article Outline
1. Introduction
- Back groundAnemia is a global public health problem affecting both developing and developed countries with major consequences for human health as well as social and economic development. It occurs at all stages of the life cycle, but is more prevalent in pregnant women and young children. It is considered to be among the most important contributing factors to the global burden of disease [12].Low iron during pregnancy can cause fatigue, reduced work capacity, cardio vascular stress, lower resistance to infection, and iron deficiency which leads to premature delivery, low birth weight, infant mortality, placental previa, premature rapture of membrane, cardiac arrest, hemorrhage, and poor cognitive development [13].According to EDHS 2011 result in Ethiopia 17% of women at the age of 15-49 are anemic, with 13 percent having mild anemia, 3 percent having moderate anemia, and 1 percent having severe anemia. A higher proportion of pregnant women are anemic (22 percent) than women who are breastfeeding (19 percent) and women who are neither pregnant nor breastfeeding 15 percent [9].The other major problem related to folic deficiency is neural tube defects (NTDs), serious birth defects of the brain and spine, are a major, preventable public health burden. Globally, it is estimated that approximately 300,000 babies are born each year with it [15].According to the WHO and Ethiopia’s national guidelines for control and prevention of micronutrient deficiencies, all pregnant women should receive and consume a standard dose of 60mg iron + 400 μg folic acid daily for 6 months starting from the first month of pregnancy or at the time of their first antenatal visit. Currently, iron-folic acid supplementation (IFA) is the main strategy for anemia control and prevention in Ethiopia [16]. But overall national data suggests that from all pregnant women supplemented with IFA tablets only 0.4% consumed > 90 tablets during their pregnancy time [17]. This indicates that identification of the factors associated with adherence to IFA supplement is an important step to improve the IFA tablets use among pregnant women.
2. Methodology
- Study designA cross-sectional descriptive institutional based study was conducted to assess the adherence rate and factors affecting to iron/folate supplements among pregnant women at selected public health instituation, in North shwea Ethiopia 2016.Study periodThe duration of the project was conducted from November to January, 2016.Source populationAll pregnant women attending ANC At selected public hospital, in north shewa Ethiopia 2016.Sample size and sampling techniqueThe sample size was determined by using 37.2% of the adherence rate of pregnant women in North Western Zone of Tigray, Ethiopia (1). And using the following assumption: 37.2% of mothers had adherence with 5% marginal error and 95%CI and a non response rate of 10%. Based on this assumption, the actual sample size for the study was determined using the formula for single population proportion.Since the average total study population in the study area is about 2804 pregnant mothers who have attended ANC in the selected governmental health instituation which is below 10,000. So reduction formula was employed as follows= Margin of error tolerated is 5%.Since multi-stage sampling technique will be used by considering the design Effect 2 the total sample size became 702.Data quality assuranceA copy of the questionnaire was submitted to the expert to examine whether the number and type of items in the questionnaire measured the concept or construct of interest.The data collection tool was translated in to local language [Amharic]. The second version of the tool was retranslated in to the English to evaluate its consistency and before the actual data collection the questionnaires was pre-tested on the same source population in 04 health center which is not selected for the study with 5% of the total sample size. Based on the findings of the pre –test some modification and developments of the tool was done. Training was given for data collectors and coordinator. Data collectors was instructed to check the Completeness of each questionnaire whether each and every question was completely answered and also the coordinator was rechecked the completeness of the questionnaire immediately after Submission.Data analysis proceduresThe questionnaires were checked for completeness by the principal investigator. Unfilled and Partially filled questionnaire was excluded. The remaining was coded, cleaned and entered in to EPI data version 3.1 statistical software package. Then the data was transfer & analyzed by statistical package for social sciences software package (SPSS) version 21.The descriptive analysis such as frequency distribution and percentages was used. Odd ratio with 95% confidence interval was used to ascertain the association between dependent and independent variable as appropriate. Bivariate and multivariate analysis was used to identify independent predictor of adherence of iron folic acid. Confidence interval of (95%) was used to see precision of the study and level of significance was taken at α =<0.05. Data presentationThe data was presented by using frequency, table, text, by measurement of central tendency and graphs.Ethical considerationEthical clearance was obtained from IRB (institution review board) of Debre Birhan University (DBU), college of health science, institute of health science and medicine. Then formal letter of cooperation was written to north shewa health Bureau, and for each health instituation from north shewa health Bureau. Each study participant was adequately inform about the purpose, method, anticipated benefit of the study and their full right to discontinued or refused to participate in the study by their data collector and asked if they are willing to participate or not. Written Informed consent was obtained from student who was participate in the study. Not asking the name of the participant to keep Confidentiality and cultural norms was respected properly.
3. Result
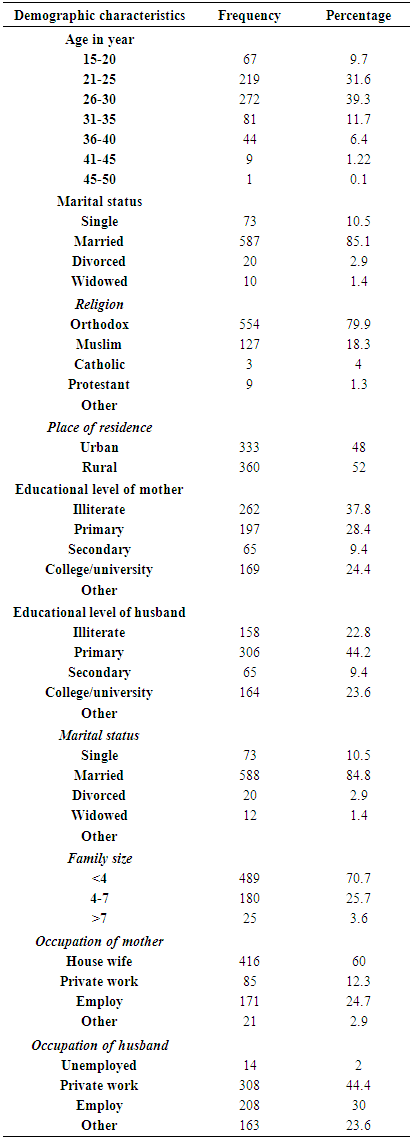
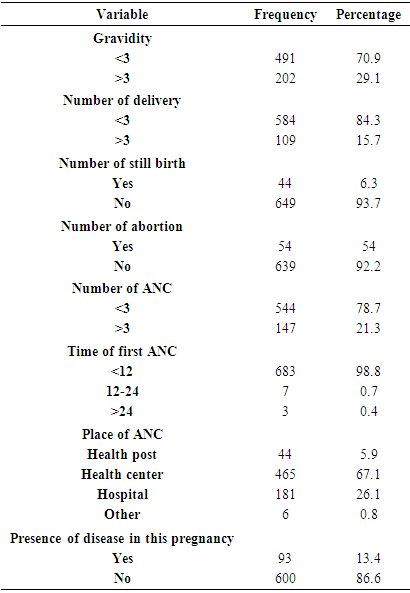
- Socio-demographic characteristics of the respondents It was proposed to distribute 702 targeted sample questionnaires from this 693 were completed and returned with a response rate of (98.7%). The mean age of the respondents was 26.3 (±5.1) years. Around 35.6% of respondent were in age group of 21-25 years and about 6.9% were in age group of 36-40 years. Majority of the women interviewed were married (85.1%). About (37.8%) of the respondents were unable to read and write, (28.9%) can read and write, (13%) had primary school level and (9.3%) had secondary school level, the percentage of pregnant women who had college and university level were (24.3%). Regarding occupation majority of the respondent were house wives (60%). Concerning residence 360 (51.9%) were in rural and 333 (48.1%) were in urban. By religion majority of respondent were Orthodox which constitute 554 (79.9%) and the remaining small proportion Muslim and Protestant were 127 (18.3%) and 9 (1.2%) respectively. Majority 590(85.1%) were married (Table 1).
|
|
|
|
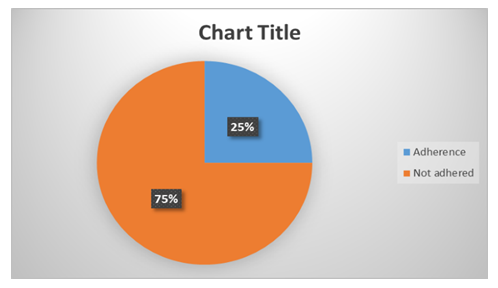 | Figure 1. Prevalence of adherence of iron folic acid |
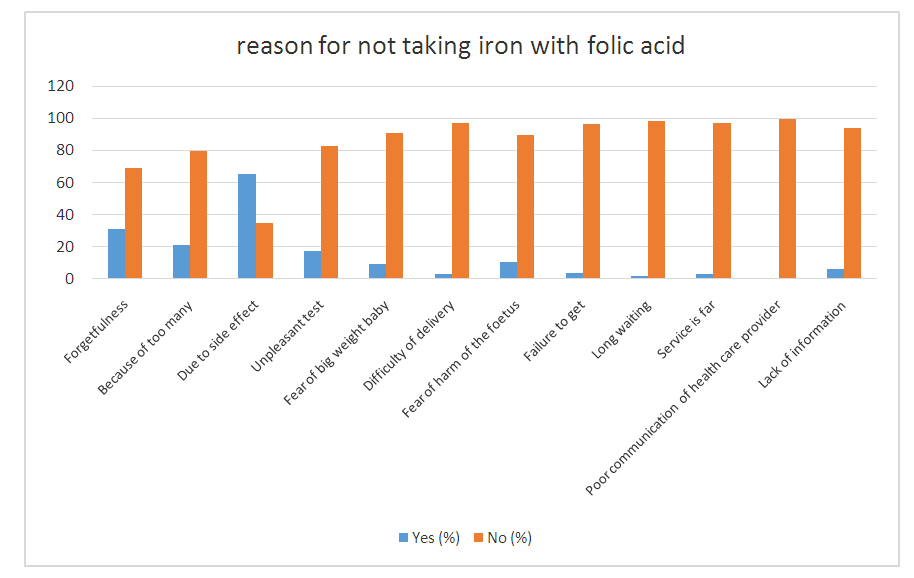 | Figure 2. Reason for not taking iron with folic acid |
|
4. Discussion
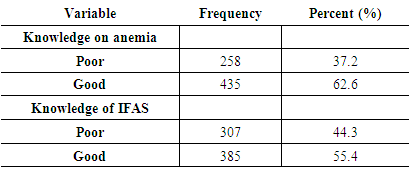
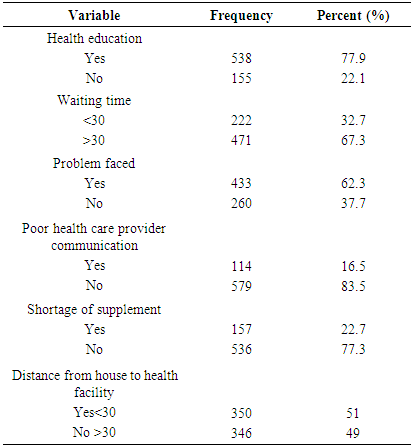
- Iron/folic acid deficiency is the major contributing factor for both maternal and neonatal morbidity and mortality. Pregnant women are among the most vulnerable group of iron deficiency anemia. But overall national report suggests that majority of pregnant women not take the drug as recommended. This indicates identification of the factor associated with adherence of iron folic acid supplementation is the important point to identify the problem and to take an intervention because Iron and folic acid supplementation is among the most feasible way to prevent anemia folic acid deficiency.The study also show that only 25% of the pregnant women had adhered to Iron and folate supplement. This figure is lower than the study conducted in debre markos town which is 55.5%, Tigray, North Ethiopia (37.2), Misha district, south Ethiopia (39.2), but other study that conducted in Eritrean refugee camp is only 7% the possible reason may be related with different in geographic location, life style, inaccessibility of health care service and there may be related with poor information regarding iron folic acid supplementation.Educational status of partner was important socio demographic factor which showed significant association with adherence to iron folic acid supplementation. Pregnant women who were having educated husband more likely to be adhered to iron with folic acid supplementation compared with those husband who were can not read and write. This finding also supported by other study done…the possible reason is educated husband have good knowledge about anemia and iron folic acid supplementation and give emphasis for adherence to iron folic acid supplementation.Adherence was better seen in those pregnant women who were less waiting time in the health facility 5.93 times more likely to be adhered to iron folic acid supplementation and those who were wait long time. This also consistent with the study done in goba the reason may be pregnant women who had short waiting time probably had better concern for their Pregnancy and good communication with health care provider.Knowledge of anemia is one of the grate factor to adherence of iron folic acid supplementation. In this study was women who had poor knowledge of iron folic acid supplementation were 0.46 times less likely adhered than who had good knowledge of iron and folic acid supplementation. The finding also supported by the study done in eight district in Ethiopia, study done in markose town and goba town. The possible reason is that those pregnant women who had good knowledge iron and folic acid supplementation were aware of the tablet importance, frequency of taking and side effect of the drug.There were different reason for adherence and non-adhered of pregnant women to iron and folic acid supplementation. Among the reason that make the pregnant women to be not adhered to iron and folic acid supplementation distance between home and health facility, forgetfulness, poor communication with health care provider, fear of side effect and long waiting time in the health facility, were the major reason. This also supported by another study in Kenya and debre markose. The possible reason for this it may be related with poor communication with health care provider and poor counseling during medical advice
5. Conclusions
- This study reviled that only one fourth of the pregnant women were adhered to iron folic acid supplementation. Educational status of the husband, waiting time, distance from health facility and health education were significantly associated with pregnant women adhered to iron folic acid supplementation. On the other hand half of the respondent had good knowledge on anemia and iron folic acid supplementation.
List of Abbreviations
Declaration
- Ethical ConsiderationsEthical clearance obtained from IRB (institutional review board) of formal letter of cooperation and written to selected organizations. Informed consent was obtain from each study participants after adequately providing information about the purpose, method, anticipated benefit of the study. Confidentiality was maintained by anonymous coding.
ACKNOWLEDGEMENTS
- Our gratitude goes to the Debre Birhan university college of medicine and health science department of midwifery for the approval of the ethical clearance. The authors would like to thank data collectors and supervisors for their commitment and the study participants for their valuable information. Funding – Debre Birhan University College of medicine and health science department of midwifery Availability of data and materials- the raw data would not be provided so as to protect client anonymity.
Availability of Data and Material
- All data supporting the findings are contained in the manuscript. Anyway, datasets are available from the corresponding author on reasonable request.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML