-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Food and Public Health
p-ISSN: 2162-9412 e-ISSN: 2162-8440
2019; 9(2): 53-59
doi:10.5923/j.fph.20190902.03

Prevalence of Underweight and Associated Factors among Children Aged Six to Fifty-Nine Months in the Pastoral Community of Korahay Zone, Somali Regional State, Ethiopia 2016. Across-Sectional Study
Sisay Shine, Wondwosen Asegidew
Public Health Department, Institute of Medicine and Health Science, Debre Berhan University, Debre Berhan, Ethiopia
Correspondence to: Sisay Shine, Public Health Department, Institute of Medicine and Health Science, Debre Berhan University, Debre Berhan, Ethiopia.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Ethiopia is among the nations with highest under-five mortality rate in the world and at least 57% of children mortality attributed by malnutrition. The objective of this study was to assess the prevalence and associated factors of underweight among 6-59 months year’s old children in the pastoral community of Korahay Zone, Ethiopia. Methods: A community-based cross-sectional study was used among 624 children paired with their mothers. Multi-stage sampling technique was used to select the study participants. Data was collected by using a structured questionnaire and anthropometric measurements. Odds ratios with 95% confidence intervals were used to assess the level of significance. Results: The study indicated that prevalence of underweight among children 6-59 months’ years old was 48.7%. Children being male (AOR: 2.0; 95%CI 1.3, 3.0), not attending antenatal care by the mother (AOR: 6.2; 95%CI 1.4, 28.1), preceding birth interval of children less than 24 months (AOR: 2.1; 95%CI 1.3, 3.2) and breast milk feeding for children less than 12 months (AOR: 2.0; 95%CI 1.3, 3.1) were significant predictors of underweight. Conclusions: This study indicated that half of the children from 6-59 months' years old were underweight. Not attending antenatal care visits by the mother and children who feed breast milk for 12 months and less were more underweight than their counterparts. Maternal education on the advantages of breastfeeding, birth interval and antenatal care visit to improve the nutritional status of children.
Keywords: Underweight, Socio-demographic, Healthcare, Environmental, Dietary, Children, Ethiopia
Cite this paper: Sisay Shine, Wondwosen Asegidew, Prevalence of Underweight and Associated Factors among Children Aged Six to Fifty-Nine Months in the Pastoral Community of Korahay Zone, Somali Regional State, Ethiopia 2016. Across-Sectional Study, Food and Public Health, Vol. 9 No. 2, 2019, pp. 53-59. doi: 10.5923/j.fph.20190902.03.
Article Outline
1. Introduction
- Underweight is referred to as being low weight-for-age (WAZ), less than minus two standard deviations (SD) of the new World Health Organization (WHO) Growth Standard. It is an indicator of both acute and chronic malnutrition problems and a broader measure of malnutrition among children aged 6-59 months [2]. Globally, about 16% (115 million) of children under-five years were underweight. The highest levels of underweight prevalence are found in South Asia, where almost half (46%) of under-five children are underweight, followed by Sub-Saharan Africa with more than one-quarter (28%) of under-five children are underweight. It is the causes for 2.2 million deaths out of these one million in African countries and 800,000 in the South-East Asia Region [3–5]. Ethiopia is among the nations with the highest under-five mortality rate in the world and at least 57% of under-five children mortality attributed by malnutrition [6]. Studies done in different part of Ethiopia reported that high prevalence of underweight among under-five children [7–10]. Past studies also showed that child sex [7–9, 11], child age [12], mother educational status [12, 13], father educational status [7], household monthly income [6, 14], antenatal care visit by the mother [13, 15], household water source [16], duration of breastfeeding [17], birth order of the children [16] and child colostrum’s feeding status [15] were factors associated with underweight. Majorities of those studies conducted in Ethiopia focused on urban dwellers, agrarian and agro-pastoral communities. No previous study attempts to address the magnitude and associated factors of underweight among the pastoral community in which the most underserved area in terms of access to essential health services and characterized by high level of child malnutrition, food insecurity and vulnerable livelihoods. Therefore, the objective of this study was to assess the magnitude and factors associated with underweight and came up with the possible recommendations for program planners who engage in the improvement of maternal and child health care services.
2. Methods
- Study design and setting: A community-based cross-sectional study was carried out from May 1-20, 2016 in Korahay Zone, Somali regional state, East Ethiopia. Korahay zone is one of six administrative zones within Somali Regional State. This is 428 km from Jig-Jiga town. The zones have six Woredas in which most population are predominantly pastoralist. According to the 2007 census the zone has 167,031 population [18]. Study participants The source population of this study included all 6–59 months years old children paired with their mothers who lived in the Zones. The study populations were all 6–59 months years old children paired with their mothers who lived in the selected Woredas. Sample size and sampling procedure Sample size was computed using a single population proportion formula with the following assumptions; 95% confidence level, 5% margin of error, reported prevalence of underweight among under five children in Shinile zone 24.5% [17], 10% non-response rate and design effect of two. The final required sample size was 624. Multi-stage sampling technique was used to select the study participants. First stage, three Woredas was selected from a total of six Woredas by lottery method. Second stage, three Kebeles was selected via lottery method from each selected Woredas. Then, the census was conducted in each selected Kebeles to know the eligible households. Final stage, households were selected by using systematic random sampling technique and took a child-mother pair from each selected household until the required sample size was fulfilled.MeasurementsThe dependent variable for the study was underweight. The independent variables considered in the study were grouped in to three: Socio-demographic factors (child sex, child age, mother educational status, father educational status, occupation status of mother, father occupational status and household monthly income); healthcare and environmental factors (number of ANC visits by the mother, PNC visits of the mother, maternal age at pregnancy, diarrheal status of children, place of delivery, birth order of children, preceding birth interval of children, source of drinking water, availability of functional toilet facility); and dietary factors (time for initiation of breastfeeding, first milk feeding, duration of breastfeeding, complimentary food starting, cup feeding, spoon feeding). Anthropometric data were collected through measurements of age and weight. Child age was collected from the mother and confirmed by using the birth certificate or vaccination cards and also used a "local events calendar". Weight was measured by an electronic digital weight scale with light clothing and no shoes. Calibration was done before weighing every child by setting it to zero. In case of children aged below two years, the scale was allowed weighing of very young children through an automatic mother-child adjustment that was eliminated the mother’s weight while she standing on the scale with her baby. WHO Anthro version 3.2.2 software was used to convert the anthropometric measures; Children whose weight-for-age Z-score is below minus two standard deviations (-2 SD) from the median of the WHO reference population are considered to be underweight [2].Operational definition Woreda: it is an administrative locality which contains more than twenty kebeles. Kebele: it is an administrative locality which contains more than one hundred households.Data processing and analysis Data was cleaned for completeness and consistencies, coded and entered into Epi info version 3.5.3 and exported to SPSS version 20 for analysis. The results were organized, summarized and presented using appropriate descriptive measures such as text, tables, frequencies and percentage. Associations between the outcome and independent variables were assessed by using odds ratios with 95% confidence intervals. Bivariate logistic regression was used to screen variables that had a significant association with the outcome variable with p-value ≤ 0.2. These variables were entered into multivariable logistic regression to assess the independent predictors for underweight. Variables which were significant at the p-value less than 0.05 and adjusted odds ratios with 95% CIs were considered to be the associated factors of childhood underweight.Data quality control measures The data collection tool was first prepared in English and translated to the Somali language and back-translated to English check for consistency. The pre-test was done on 5% of the respondents prior to the actual data collection period. Training was given for both data collectors and the supervisor on the data collection tools and techniques of interviewing. Daily supervision was done by the supervisors and principal investigators.
3. Results
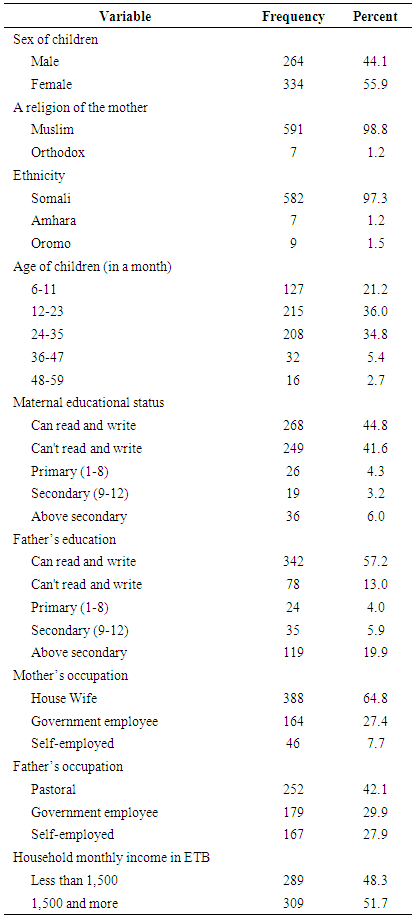
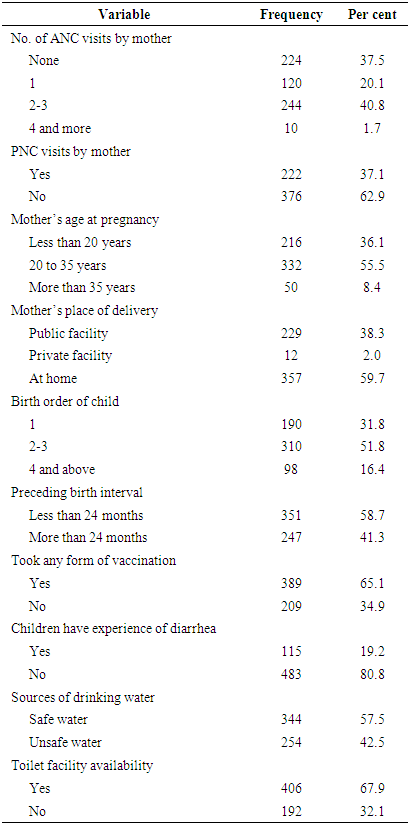
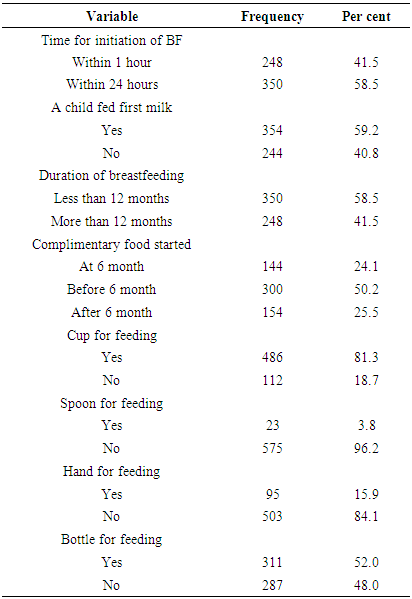
- Socio-demographic characteristics: A total of 598 children between 6-59 months year old with their mothers were participated in the study that made the response rate of 95.8%. Out of the total respondents, 334 (55.9%) were females. The majority of participants 215 (36.0%) were between 12-23 months year old, followed by 24-35 months year old which accounted 34.8%. Five hundred ninety-one (98.8%) were Muslim followers in religion and 582 (97.3%) were Somali in ethnic group (Table 1).
|
|
|
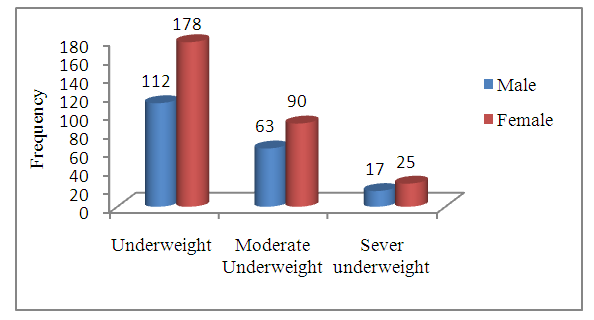 | Figure 1. Underweight with sex between 6-59 months year old in the pastoral community of Korahay Zone, Ethiopia, 2016 |
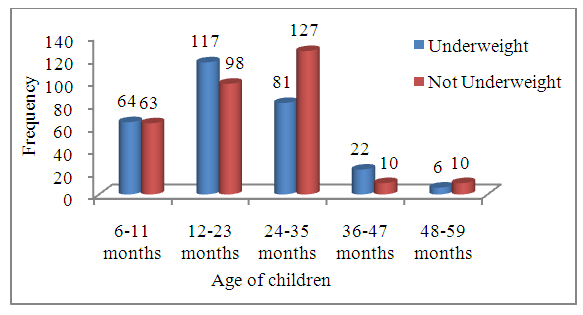 | Figure 2. Underweight with age categories 6-59 months year old in the pastoral community of Korahay Zone, Ethiopia, 2016 |
|
4. Discussion
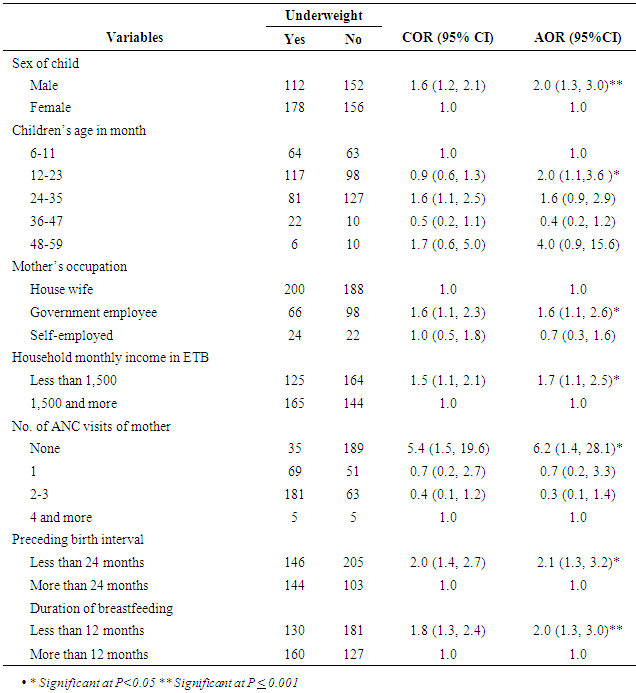
- The prevalence of underweight in the study area was high 48.5% according to the WHO classification standard. This was congruent with previous study reports in different parts of Ethiopia like Dola Ado (47.7%) [8] and west Gojam (49.2%) [13]. However, the findings of this study were higher than the report in south India (22.7%) [19], Iran (9.66%) [20], Rwanda (11.0%) [21], Kenya 18.1% [22] and in the different part of Ethiopia [1, 10]. This might be due to the fact that mothers in food insecure and inaccessible health service areas were at a high risk of getting underweight babies. On the other hand, the prevalence of underweight was lower than the reports in Mangalore (63.16%) [23], Pakistan (54.3%) [24] and India (52.9%) [25]. This might be the difference in the study population.The result of this study showed that underweight was more prevalent on male children (AOR: 2.0; 95% CI 1.3, 3.0) than female children. This was consistent with the reports in South Africa [26], Rwanda [21] and in the different part of Ethiopia [7, 8, 11]. In contrast, a study conducted in India [25], Nepal [27] and Ethiopia [10] showed that females were more underweight than males. These discrepancies in finding could be attributed to differences in cultures or traditional norms and gender issues on preferential treatment among opposite sex, parents’ educational status and nutritional factors among communities.Children age 12-23 months were about 1.95 times more likely to be affected by underweight than children age 6-11months (AOR: 2.0;95% CI 1.1, 3.6). It was consistent with previous study done in Mangalore [23] and Ethiopia [1, 6]. Children at this age category start walking on their own and they try to eat what they got in the field, thus increasing their exposure to infections and susceptibility to illness. This tendency, coupled with inappropriate or inadequate feeding practices may contribute to faltering nutritional status.The current study revealed that household monthly income was a strong predictor of underweight. It was consistent with the study conducted in India [28] and Ethiopia [6, 14]. This is not surprising as the household which has low monthly income can’t access different kinds of nutritious food and amounts of food available for consumption.In the study area mothers who did not visit ANC were 6.21 times more likely to have the underweight child than those who had four and above ANC visits. Other studies conducted in Ethiopia, showed that mothers who did not attend ANC visit were more likely to have the underweight child than their counterpart [13, 15]. This study has been addressed only certain issues related to the underweight status of under-five children and determining covariates because of some limitation: Since the study employ cross-sectional study it is difficult to establish a cause-effect relationship. Important variables like Body Mass Index (BMI) of mother and size of children during birth were not assessed these might have an impact on the result of the study. Qualitative data were not included to explore some associated factors and triangulate the finding of the quantitative data through qualitative data.
5. Conclusions
- Prevalence of underweight among children age 6-59 months in the study area was found to be high. Sex of children (being male), the age of children (between of 12-23 months years old), government employee mothers, low household monthly income, preceding birth interval within 24 months, breastfeeding less than 12 months and mother not attend antenatal care follows up were predictors of childhood underweight. Educating mothers on the advantage of breastfeeding, birth interval and antenatal care visits can promote the nutritional status of children.
List of Abbreviations
- ANC - Antenatal Care, AOR– Adjusted Odd Ratio, PNC - Postnatal Care, SD - Standard Deviation, SPSS - Statistical Package for Social Science, WAZ-Weight-for-Age Z-score, WHO - World Health Organization.
Declarations
- Ethical approval and consent to participateThis study was carried out after getting ethical clearance letter from Jig-Jiga University research ethics review committee. Data collection was carried out after receiving an ethical clearance letter from the regional health bureau and administration office. Informed consent was obtained from each study subject after an explanation of why they take part in research. They were also informed participation is volunteer based. Confidentiality has been ensured from all the data collectors, supervisors and investigators side using code numbers than names and keeping questionnaires locked.
ACKNOWLEDGEMENTS
- We would like to thank the Regional Health Bureau and Zonal Health Office head for their collaboration during conducting this research. Our gratitude also goes to our data collectors and study participants for their willingness to participate in the study. At last but not least, we would like to forward my special thank and sincere appreciations to our friends who gave advice and comment throughout the whole research project activities.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML