-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Food and Public Health
p-ISSN: 2162-9412 e-ISSN: 2162-8440
2016; 6(6): 149-156
doi:10.5923/j.fph.20160606.01

Food Insecurity, Not Stress is Associated with Three Measures of Obesity in Low-Income, Mexican-American Women in South Texas
Jennifer J. Salinas1, William Shropshire2, Ana Nino3, Deborah Parra-Medina4
1Department of Family Medicine Texas Tech University Health Sciences Center at El Paso, El Paso, United States
2Department of Epidemiology, Human Genetics and Environmental Sciences, University of Texas Health Sciences Center School of Public Health, Houston, United States
3School of Medicine, University of Texas Southwestern, Dallas, United States
4Mexican American and Latina/o Studies, University of Texas at Austin, Austin, United States
Correspondence to: Jennifer J. Salinas, Department of Family Medicine Texas Tech University Health Sciences Center at El Paso, El Paso, United States.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: To determine the relationship between obesity, food insecurity and perceived stress in very low income Mexican American women. Design: Cross-sectional baseline data analysis of a randomized clinical trial. Setting: Texas-Mexico border region of South Texas. Subjects: Very Low Income Mexican American Women. Results: The relationship between obesity and food insecurity in a sample of very low income Hispanic women living in South Texas depends on the measure of obesity and the dimension of food insecurity. The only measure of food insecurity associated with all measures of obesity was often not having enough money to afford to eat balanced meals. Waist circumference was associated with the most dimensions of food insecurity, while BMI had the least associations. Finally, perceived stress was not significantly associated with BMI, waist circumference or percent body fat when adjusted for other covariates. Conclusions: We have found a strong and significant relationship between food insecurity related to having enough resources to eat a balanced diet and BMI, waist circumference, and percent body fat in low-income Mexican American women. While behavioural change is an important strategy for reducing obesity, consideration may need to be made as to how food access with high nutritional value, may be in and of itself a contributing factor in obesity in low income populations.
Keywords: Mexican Americans, Obesity, Food Insecurity, Perceived Stress
Cite this paper: Jennifer J. Salinas, William Shropshire, Ana Nino, Deborah Parra-Medina, Food Insecurity, Not Stress is Associated with Three Measures of Obesity in Low-Income, Mexican-American Women in South Texas, Food and Public Health, Vol. 6 No. 6, 2016, pp. 149-156. doi: 10.5923/j.fph.20160606.01.
Article Outline
1. Introduction
- The increasing prevalence of obesity over recent decades has led to an increased burden on our public health infrastructure [1]. There has been a 59% increase in age-adjusted prevalence of obesity for adults aged 20 years and older in the United States from 1988-1994 to 2011-2014. This is of paramount concern due to the well-established associations of obesity with a large number of health risks such as cardiovascular disease, coronary heart disease, type II diabetes, and all-cause mortality [3]. This increasing prevalence of obesity disproportionately affects minority populations, such as for Mexican-American adults where age-adjusted obesity prevalence is 46.4% compared to 34.6% of non-Hispanic whites [2]. There are many factors that may contribute to this disparity including higher rates of poverty and overall lower socioeconomic status in Mexican-American women. Food insecurity affects millions in the United States. It is estimated that 14% of American households are food insecure, while 22.4% of US Hispanic households4 go without food on a regular basis. Food insecurity is the result of not having sufficient economic resources to purchase foods to sustained adequate calorie or nutritional intake [5]. Women are particularly affected by food insecurity [5-11]. Women are often put in the precarious position of sacrificing their own food to ensure that their children do not go hungry [5]. Paradoxically women who are food insecure have a greater likelihood of being overweight relative to their food secure peers [8]. Food insecure women were also found to be on average 2 BMI units heavier than women in food secure households [9]. Although limited information is known about race/ethnic differences in the etiology of food insecurity, there is some evidence that obesity may be more closely related to food insecurity in Hispanics than in non-Hispanic whites [10, 12]. The mechanistic effect of food insecurity on obesity is not well understood, however, one recent hypothesis suggests that weight gain may be a physiological response for persons with low socioeconomic status [13]. For example, stress could be a mediating factor in the food insecurity and obesity relationship. Hispanics living in colonias, unincorporated residential areas often lacking basic infrastructure along the US-Mexico border, experience high levels of stress due to economic hardships, lack of access to healthcare, and high crime rates [14, 15]. In the literature, both chronic and perceived stress have been associated with increased obesity in Hispanic populations [16, 17]. The Genetics of Atherosclerotic Disease study found that Mexican women were more likely to experience chronic stress when compared to Mexican men and this was associated with increased visceral fat deposition [17]. Increased accumulation of visceral fat in women has been linked to increased risk of heart disease, diabetes, and overall mortality [18-20]. One potential mechanism for increased burden of obesity among the poor may be chronic stress and related physiological responses to social and environmental stressors associated with poverty [21, 22]. These environmental stressors may in part affect the dietary quality of persons with low income whom are food insecure [23]. This is further supported by the observation in animal models that stress may induce a greater urge to consume more calories beyond satiety24. It is therefore possible that food insecurity coupled with stress may exacerbate the risk for obesity in low income populations – potentially providing a pathway in which Mexican-Americans become susceptible to obesity.The primary objective of our study is to use three most commonly used measures of obesity to examine the relationship with food insecurity in our sample of 554 low-income Mexican-American women South Texas. Although the majority of studies examining the relationship between food insecurity and obesity in adults use BMI as the predominant measure of obesity [7-9, 25-28], there are notable limitations especially when considering genders of the same age across different ethnicities [29-31]. Since Hispanics have higher levels of adiposity, waist circumference and percent body fat can be useful obesity markers in addition to BMI [31, 32] and to our knowledge only three studies have used percent body fat to test the relationship with food insecurity [33-35]. Therefore, using multiple measures of obesity could provide a more accurate ac-count of how obesity may be associated with food insecurity. [36]. Furthermore, we are interested to see how perceived stress affects the food insecurity/obesity relationship within our unique study sample of low-income Hispanic women.
2. Methods
2.1. Sample
- The data used from this study came from the baseline collection of a large randomized clinical trial (RCT). The goal of the RCT – Enlace – was to evaluate a promotora (community health worker in a Hispanic community)-led physical activity (PA) intervention to increase moderate-to-vigorous physical activity (MVPA) among a particularly underserved segment of Latinas living in the Texas-Mexico border region. A total of 554 Mexican origin participants ages 18-64 years who did not meet recommended U.S. national PA guidelines were recruited into this study.
2.2. Measures
- All measures were collected in person by trained study staff at eight participating community resource centres. All questionnaires were administered in both Spanish and English depending up participants’ preferences.
2.2.1. Food Insecurity
- Participants were asked the six-item short form from the U.S. Household Food Security Survey Module from the United States Department of Agriculture. This module reduces respondent burden and is an acceptable substitute to the longer 18-item U.S. Household Food Security Survey Module 37. The Food Security Scale assesses hunger in the past 12 months and assigns food security categories. The questions asked are: 1) ‘The food that I bought just didn’t last, and I didn’t have money to get more. Was that often, sometimes, or never true for you in the last 12 months?’; (2) ‘I couldn’t afford to eat balanced meals. Was that often, sometimes, or never true for you in the last 12 months?’; (3) ‘In the last 12 months, did you ever cut the size of your meals or skip meals because there wasn’t enough money for food? Yes or No’; (4) ‘If the response is “Yes”, how often did this happen? Was it almost every month, some but not every month, or only in one or two months in the last 12 months?’; (5) ‘In the last 12 months, did you ever eat less than you felt you should because there wasn’t enough money to buy food? Yes or No’; and (6) ‘In the last 12 months, were you ever hungry but didn’t eat because you couldn’t afford enough food? Yes or No’. Responses of “often” or “sometimes” on questions 1 and 2 and “yes” for questions 3, 5, and 6 are coded as affirmative, as are responses of “almost every month” and “some months but not every month” for question 4. Each question was used individually for all analyses.
2.2.2. Body Mass Index
- Height was measured to the nearest 0.25 inch using a fixed stadiometer without shoes and socks. A bioelectrical impedance analysis (BIA) machine (Tanita SC-331S) was used to determine body weight (lbs.) and body mass index (BMI; kg/m2).
2.2.3. Body Fat Percentage
- Using a BIA machine, participants’ percent body fat was measured to the nearest 0.1%. Participants placed their feet on the Tanita’s electrodes and weighing platform and remained motionless until readings were displayed on the screen of the analyser.
2.2.4. Waist Circumference
- Waist circumference was measured by trained staff to the nearest 0.1 cm. The measurement was recorded twice, underneath the clothes and over the umbilicus area while the participant was standing with arms at the sides with relaxed abdomen. A third measurement was taken if the difference between the first two measurements was greater than 2 cm.
2.2.5. Stress
- Perceived stress was assessed using the 10-items Perceived Stress Scale, which has shown reliability in both Spanish and Mexican-origin populations [38, 39]. Questions asked how often in the past month had participants held particular feelings and thoughts with responses ranging from Never (0) to Very often (4). The score of items 1,2,3,9 and 10 are summed as are the reverse coding of questions 4, 5 7 and 8. The scale ranged from 1-40 with a score of 1-12 as low to no stress, 13-19 moderate and a score of greater than 20 considered high stress.
2.2.6. Demographic Covariates
- Demographic questions included age (continuous), nativity (US born vs. Mexico born), highest level of education completed (continuous), household monthly income ($0-$999, $1000 +, missing), and insured (yes/no).
2.3. Statistical Analysis
- Descriptive statistical analysis of demographic characteristics, food insecurity, stress and our obesity outcomes was first performed. Chi-square tests and ANOVA tests were used to examine bivariate relationships between our three measures of obesity (BMI, % BF, and WC) with demographic characteristics, food insecurity, and stress, with p values of <0.05 considered statistically significant. Variables with resulting significant associations in univariate analysis with each of our respective measures of obesity were included in multiple linear regression models as potential confounding variables. Stepwise linear regression was conducted to predict BMI by food insecurity, perceived stress, and significant demographic covariates. Finally interaction models were conducted to determine if the relationship between food insecurity and measures of obesity varies by the level of perceived stress. All analysis was conducted using STATA 14SE (Stata Corp 2014).
3. Results
- Table 1 shows frequencies and means of BMI, waist circumference, and body fat by food insecurity measures and perceived stress on our 554 participating women. Over 50% of participating women reported food not lasting or couldn’t afford a balanced meal at least ‘sometimes’ or ‘often’. However, a lower portion had responses: ever cut portion size (31.8%), didn’t have enough money to pay for food (19.5%) or were hungry and could not afford to buy food (13.5%). Approximately, one third of the sample is 30-39 or 40-49 years of age and the majority of the sample have between 7 and 12 years of education (63.2%). The majority of participants are immigrants from Mexico (87.1%) and do not have insurance (83.1%). Nearly half of our sample (44.6%) reported monthly household income of $999 or less with approximately one in ten respondents (11.3%) that refused to provide any income information at all. Our sample also had approximately 67% of moderate to high levels of perceived stress responses.
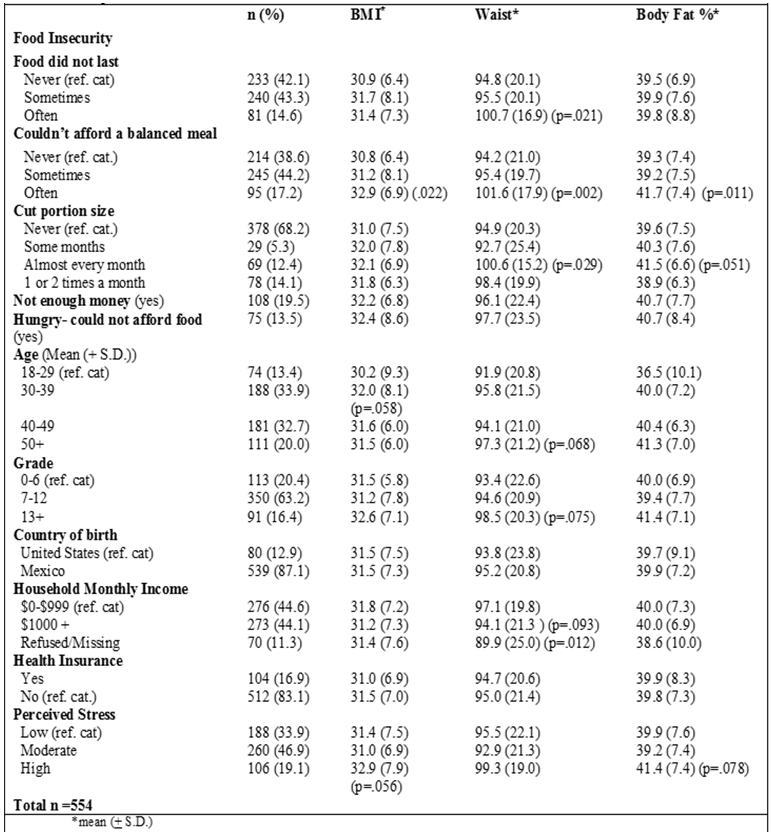 | Table 1. Average BMI, waist circumference, and body fat by food insecurity measures, demographic characteristics, nutrition and perceived stress |
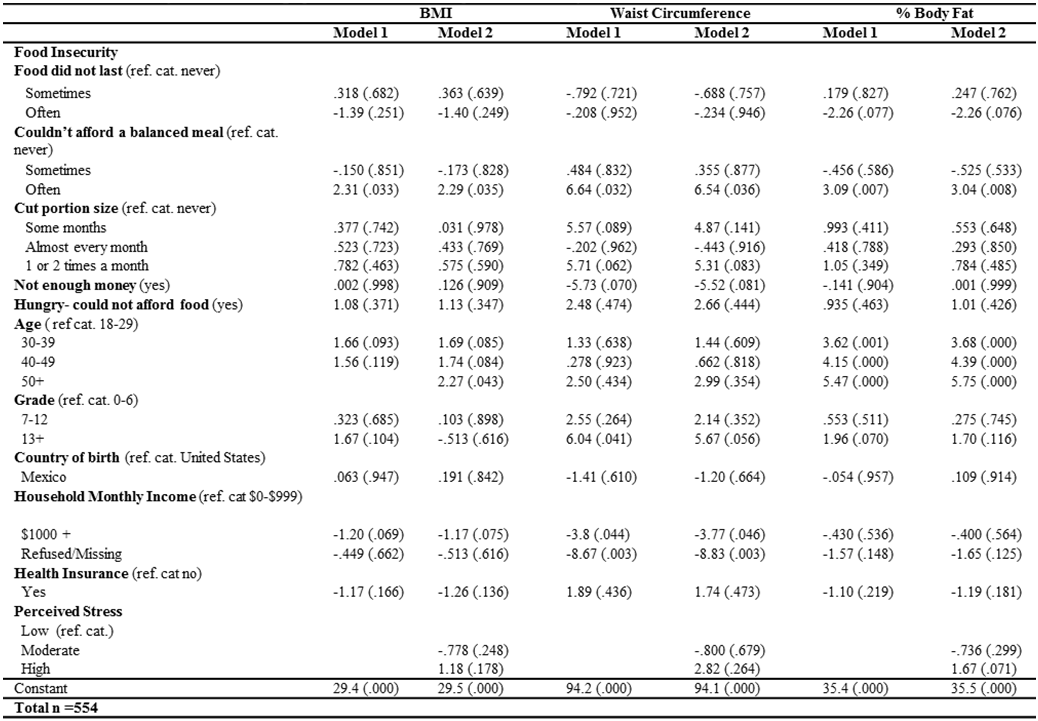 | Table 2. Food Insecurity measures, demographic characteristics, and perceived stress by BMI |
4. Discussion
- The purpose of this paper was to determine the relationship between food insecurity and measures of obesity in a sample of very low income Hispanic women and to determine if perceived stress moderates this effect measure. Multiple measures of obesity were used to assess associations with different dimensions of food insecurity. Findings from this study revealed that the relationship between obesity and food insecurity in a sample of very low income Hispanic women living in South Texas depends on the measure of obesity and the dimension of food insecurity. The only measure of food insecurity associated with all measures of obesity was often not having enough money to afford to eat balanced meals. Waist circumference was associated with the most dimensions of food insecurity, while BMI had the least associations. Finally, perceived stress was not a significant modifier in the relationship between food insecurity and any of the obesity outcome measures.There have been few studies that have investigated the relationship between food insecurity and multiple measures of obesity [33-35]. Our study’s findings suggest that food insecurity is likely to be most associated with waist circumference than BMI or % body fat in this sample of very low income Hispanic women living in South Texas. Other studies that have investigated the relationship between food insecurity and obesity have primarily used BMI rather than waist circumference or percent body fat. These studies predominantly have found a positive association between food insecurity and obesity especially for women [5-11, 25-28]; however, the functionality of this relationship remains unclear [6] and does not appear to hold for men. [7, 25-27]. The few studies that have included Hispanics have found high prevalence of food insecurity [4, 10] especially in low resource settings [12]. One study found a positive relationship between food insecurity and obesity for Mexican-American women, but neither men nor other Hispanic groups [11]. Therefore, our study adds to a growing knowledge of the likely association between food insecurity and obesity in low income populations of women living in the United States. Obesity prevention programs may need to address issues of food insecurity in order to have high impact on low and very low income populations.Findings from this study provide evidence that food insecurity that involves not having enough economic resources to eat a balanced diet or afford food on a regular basis may be related to a higher waist circumference. This is an important finding since past literature on the relationship between waist circumference and metabolic diseases is well established [20, 40] with Hispanics in particular having an increased propensity for metabolic diseases such as diabetes [41]. Our results should be considered along with a case-control study that found Latinas aged 35-60 years old with very low food security had 3.3 times greater odds of prevalent type II diabetes as compared to those food secure after controlling for potential confounding factors [41] Similar associations between food insecurity and metabolic diseases have been seen in other populations as well [42]. It is important to note that our study population includes low-income, Mexican-born women in a region of South Texas where prevalent diabetes is higher than the national average. While more research is needed to further evaluate this relationship, improving access to affordable nutritious foods may be a cost-effective approach to also preventing the onset of diabetes in this vulnerable population [43]. There is growing evidence that food insecurity may be associated with higher BMI scores in other non-Hispanic populations, yet, few studies have investigated this relationship with Hispanic populations [4, 10, 12]. This study provides evidence that the food insecurity measure - not having enough to eat a balance meal often - is associated with an increased average BMI in our sample; however, waist circumference had the most significant associations with multiple food insecurity measures. The use of BMI alone as a measure of obesity may not give a comprehensive depiction of this relationship between obesity and food insecurity in very low income populations as well as across different age and ethnic groups. Therefore, research examining the relationship between obesity and food insecurity should consider including multiple measures of adiposity as was done in this study. Perceived stress was not directly associated with any of the obesity outcome measures in this sample. Furthermore, perceived stress did not modify the relationships between any of the food insecurity domains and the obesity measures. Previous evidence on stress and obesity indicated that stress increases physiological biomarkers that may alter fat storage and metabolic pathways that could increase the likelihood of obesity [44, 45]; however the effect of stress on obesity in epidemiological studies is less clear [46]. One issue is that there are few studies that have examined the relationship of stress with respect to food insecurity or in very low-income Hispanics for adequate comparison to our findings in our study [16, 47]. Potentially due to the extreme poverty in this sample, the high baseline of moderate to high levels of stress in our sample (67%) may prove there was not enough variation to detect differences as it relates to measures of obesity or food insecurity. Living in extreme poverty that creates stress may impact biological mechanisms leading to increased risk for obesity for Mexican-American women living in the Texas-Mexico border region. This relationship was not tested in this study, therefore, future studies are needed to explore the relationship between aspects of living in poverty, such as stress, and changes in biological functioning that may create an increased risk for obesity or other metabolic disorders. In summary, the food insecurity measure not having enough economic resources to eat a balanced diet is strongly associated with BMI, waist circumference, and percent body fat in this sample of low-income, Mexican-American women. Additionally, waist circumference was most closely associated with multiple food insecurity dimensions relative to the other two measures. These findings warrant further examination in the Mexican-American population due to the over representation of those living in poverty areas such as colonias, as well as the high prevalence of obesity and metabolic disease in this population living in South Texas. Potential explanatory factors to explain this relationship may include environmental factors such as food access in neighbourhoods of the extremely poor, unmeasured social or cultural factors, or potential biological changes that may be associated with inconsistent access to food over long periods of time. Future research should further examine these possibilities in this population or relative to other race/ethnic groups.While these findings provide compelling evidence on the relationship between food insecurity and measures of obesity in particular waist circumference and BMI there are a number of limitations that should be noted. First, the sample selected for this study was recruited from an area of Texas that is characteristically poor with a very high Mexican American population. Therefore, inferences may not be appropriate for the larger Mexican American population in the United States. Additionally, because there is such a high concentration of Mexican Americans living in this region, the relationship between food insecurity and BMI, waist circumference, and percent body fat may operate differently in Mexican Americans who live in more acculturated, heterogeneous populations. Moreover, this sample of women did not meet the minimum recommendations for physical activity although it is worth noting the general population of Texas engages in similar levels of physical activity as what was observed in this border sample. Finally, due to the cross-sectional nature of this data, it is only make conclusions on associations and not infer causation. Therefore sampling of other low income Hispanics and other populations to determine if similar patterns hold true over time in other settings is a necessary next step. In conclusion, there is a strong and significant relationship between food insecurity related to having enough resources to eat a balanced diet and BMI, waist circumference, and percent body fat in low-income Mexican American women. While behavioural change is an important strategy for reducing obesity, consideration may need to be made as to how food access with high nutritional value, may be in and of itself a contributing factor in obesity in low income populations. This could be accomplished, for example by increasing the availability and decreasing the cost of fresh fruits and vegetables in low income neighbourhoods, or providing financial incentive for choosing healthier food options. Interventions that are implemented at a policy level may be necessary to address obesity in populations that are also food insecure.
ACKNOWLEDGEMENTS
- This work was supported by the National Heart, Lung, and Blood Institute (grant number HL111718) to the University of Texas Health Science Center San Antonio (Parra-Medina, PI).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML