-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Food and Public Health
p-ISSN: 2162-9412 e-ISSN: 2162-8440
2016; 6(2): 52-57
doi:10.5923/j.fph.20160602.04

Dairy Fat Consumption and Mortality due to Cardiovascular Disease. Does Source of Fats Matter?
Paula Moliterno1, Florencia Cerruti2
1Escuela de Nutrición, Universidad de la República, Montevideo, Uruguay
2Universidad Católica del Uruguay, Montevideo, Uruguay
Correspondence to: Paula Moliterno, Escuela de Nutrición, Universidad de la República, Montevideo, Uruguay.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study analyzed data for correlation between dairy fat availability for consumption and cardiovascular mortality, in adults of both sexes from 35 to 74 years of age, across a selection of countries. In addition we focused on the dietary levels of vegetable and animal fats in countries with high and low cardiovascular mortality.Mortality statistics were taken from the WHO, 2014. Data pertaining to fat availability for consumption was obtained from Food Balance Sheets (FAOStat, 2011). Consumption patterns of animal and vegetal fats were analyzed for countries with high and low cardiovascular mortality.Evolution of dairy fat consumption has changed over time. Cardiovascular mortality showed high rates in countries within the region. Countries with low cardiovascular mortality showed higher levels of vegetable fat consumption, while countries with high mortality rates showed higher levels of animal fat consumption. No particular pattern was observed for dairy fat. This study found no significant correlation between dairy fat consumption and cardiovascular mortality.
Keywords: Dairy Fat, Cardiovascular Disease, Mortality, Vegetable and Animal Fats
Cite this paper: Paula Moliterno, Florencia Cerruti, Dairy Fat Consumption and Mortality due to Cardiovascular Disease. Does Source of Fats Matter?, Food and Public Health, Vol. 6 No. 2, 2016, pp. 52-57. doi: 10.5923/j.fph.20160602.04.
Article Outline
1. Introduction
- Cardiovascular disease (CVD) is responsible for approximately 17 million annual deaths greatly affecting countries of low and medium income, determined in 2008 the main cause of mortality in adults younger than 60 years old [1]. The World Health Organization (WHO) estimates that the number of deaths caused by this disease will grow 23.3 million by 2030, continuing as the leading cause of death globally [2].Unhealthy diet has been defined by the WHO as a modifiable risk factor and fundamental determining in the incidence of CVD [3], reason why the lipid fraction of the diet has traditionally been involved in its management and risk prevention [4]. International statistics indicate a strong correlation between the consumption of saturated fat (from animal products) and mortality caused by coronary heart disease [5]. Evidence shows that high intake of saturated fat (SF) and industrial trans fatty acids is associated to a greater incidence of these diseases [6], so the recommendation to diminish its consumption has become a priority health measure to reduce the risk of CVD [7-9].Traditionally, dairy products have played a fundamental role in human nutrition associated to their composition rich in nutrients; however, dairy fat has a varied fatty acid composition, highlighting the saturated palmitic fatty acid with proven metabolic effect on cardiovascular health. An ecologic study on year 1979 showed a strong correlation between the availability of dairy fat and mortality by cardiovascular disease (r= 0,75) [10]. These results along with those gathered by the Seven Countries Study [11] have determined a recommendation on the inclusion of low-fat dairy in promoting cardiovascular health. Nonetheless, lately, evidence available shows contradicting and inconclusive results related to the consumption of dairy products and risk and mortality due to CVD [12-15].In this context, we proposed the hypothesis that a higher availability of dairy fat for human consumption is correlated to higher rates of cardiovascular mortality, since dairy products constitute food which saturated fat has fatty acids known for its implication in the development of CVD.The main objective of this study was to observe the evolution in the consumption of dairy fat and the availability of vegetable and animal fat in a group of countries where the rates of cardiovascular mortality cover a broad spectrum. Intended to provide new information relevant to elucidate the contradictions described in previous paragraphs, the relation between availability of dairy fat for consumption and cardiovascular mortality rates in countries with extreme cardiovascular mortality was analyzed.
2. Material and Method
- A descriptive, observational and cross-sectional study was designed.Data of availability of dairy fat, animal fat and vegetable fat for human consumption was obtained through Food Balance Sheets of FAO (FAOStat, 2011) for the period of 1970 to 2011 [16]. This instrument allows determining the apparent national consumption of each food, presenting the structure of the main food supply of a country during a reference period. Based on this information, animal fat are subcategorized in meat fats and dairy fats. Meat fat constituted the animal fat except dairy fat.Data of 24 countries of different continents were added considering those included in the Turpeinen study of 1979; United States and Canada, Italy, Portugal, France, England, Netherlands, Switzerland, Spain, Poland, Finland, Romania, Sweden, Austria, Norway and Germany; Japan; Australia and New Zealand. In order to complement the analysis with Latin American countries that were not included in the study mentioned, data from Uruguay, Argentina, Chile, Brazil and Costa Rica were included.For cardiovascular mortality analysis, data published by the WHO in 2014 [17] was used. Age-standardized cardiovascular mortality rates were analyzed for adult age (35 to 74 years old). Additionally, specific-sex mortality rates were analyzed. Cardiovascular mortality causes were considered as all below the item “circulatory system diseases” in the International Classification of Diseases (ICD-10) [18].For the study of the consumption of animal and vegetal fats, 10 countries in the extreme spectrum of mortality rates were selected. Based on prior, low mortality rates were considered fewer than 100 (each 100.000) and high mortality, rates higher or equal to 100.1 (each 100.000).To study the association between the availability of dairy fat and mortality due to CVD in 24 chosen countries, the statistical Pearson correlation coefficient test was applied.All analyses were conducted with the use of SPSS statistical software.
3. Results
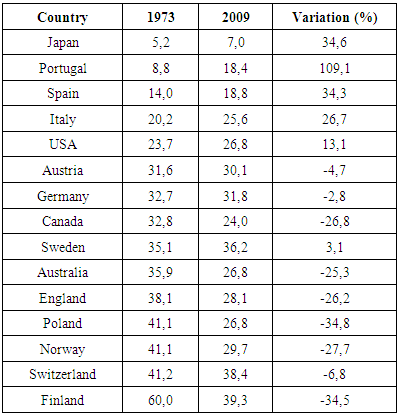
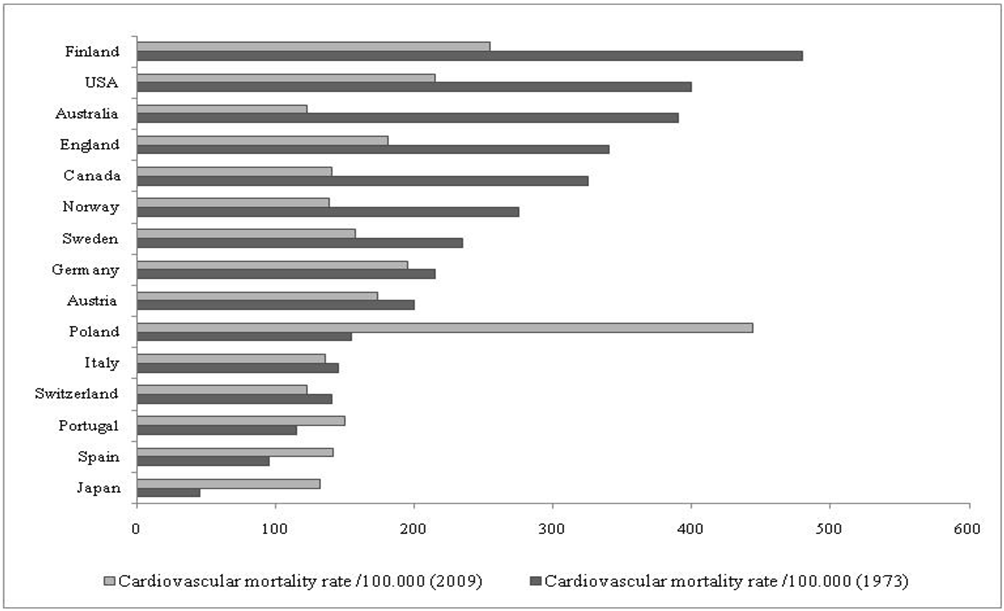
- Mortality rates due to CVD are shown comparatively in Figure 1. The difference in cardiovascular mortality was more than 5 times between the first place Rumania (436/100.000) and the last one France (80.4/100.000). Statistics indicate that Rumania (436 each 100.000) and Poland (294.2 each 100.000) are among the countries which cardiovascular mortality rates are higher. In Latin America, Brazil (249 each 100.000), Argentina (198.5 each 100.000) and Uruguay (176.9 each 100.000) were placed with higher cardiovascular mortality rates.
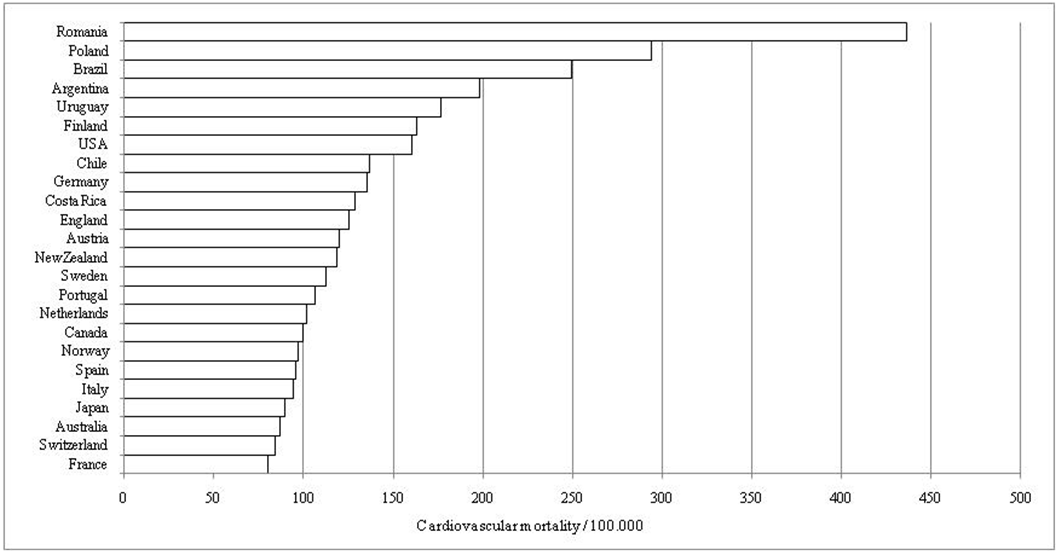 | Figure 1. Cardiovascular mortality among adults (35-74 years old), both gender, in a selection of 24 countries. WHO 2009 |
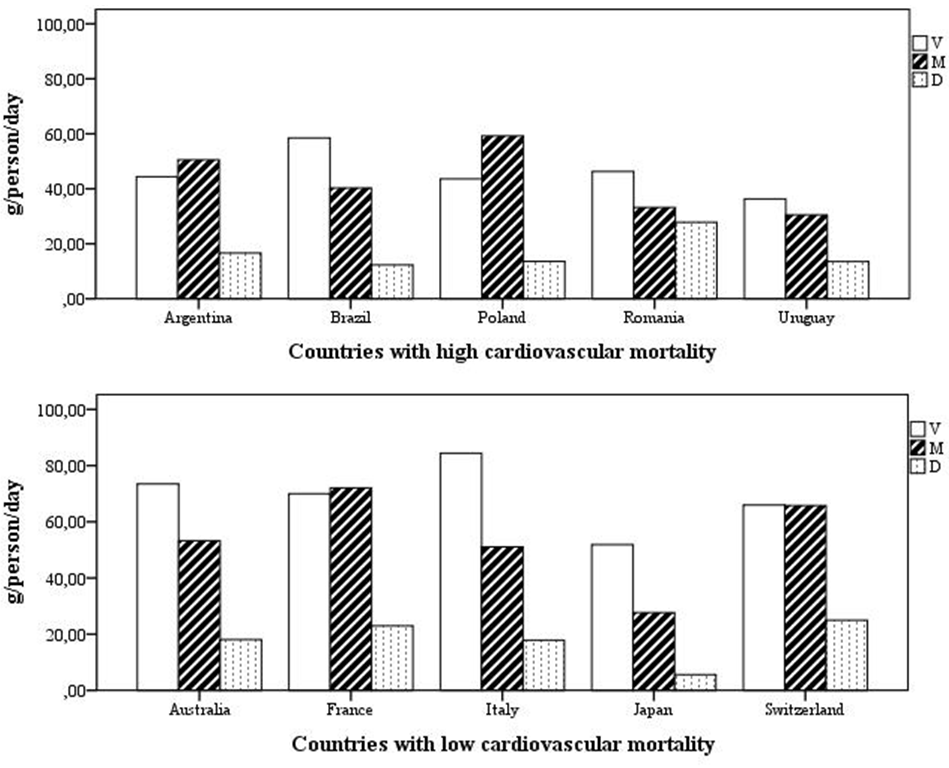 | Figure 2. Availability for human consumption of major food fats in 10 countries with high and low cardiovascular mortality, respectively. V = vegetable fats, M = meat fats, D = dairy fats |
|
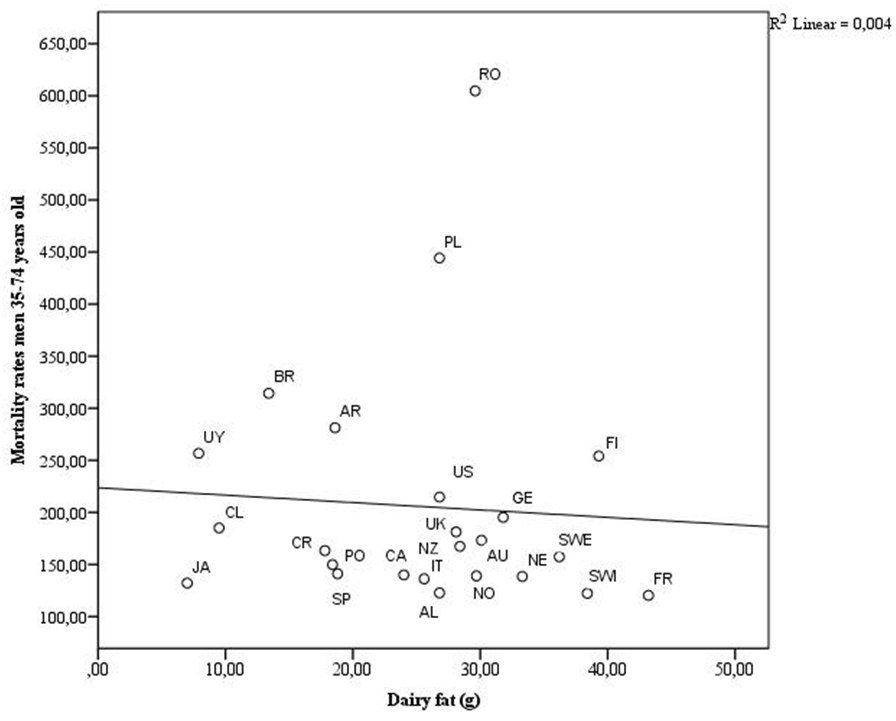
 | Figure 3. Comparison of mortality due to CVD among adult men (35-37 years old) for a countries selection. WHO 1973, 2009 |
4. Discussion
- The main find of this study was that currently, no statistically significant correlation exists between availability of dairy fat for consumption and mortality due to CVD, unlike past findings (r= 0,75 p<0,001) [10], which may not allow to confirm the hypothesis at first formulated. At the present time, an increase in availability of dairy fat for consumption in adult men would not be statistically associated with increases in mortality rates due to CVD. Moreover, changes in location of countries at the correlation line were observed, showing differences among those two variables over time. In 1979, countries such as Finland and New Zealand of important dairy production were located at the upper extreme of the correlation line, whilst Asian countries like Japan and the Mediterranean countries were located on the lower extreme. Currently, Finland is located among countries with major availability of dairy fat for consumption and lower mortality rate. Such variations could be related to successful community-based intervention actions that have been carried out since 1971 in order to reduce the problem of CVD in Nor Karelia, extending nationwide, with emphasis on unhealthy diet as one of the fundamental risk factor [19]. On the other hand, Japan showed lower cardiovascular mortality rates and modest availability of dairy fat for consumption, being vegetable fats the predominant type of food fats. However, the analysis of variation of male mortality rates over time showed an important increase which occurs with a non proportional increase of availability of dairy fat, coinciding with increasing evolution of availability of dairy fat in Asian region. Uruguay, cattle country, valued for the quality of its dairy products, showed availability of dairy fat among the modest and leading mortality rates due to CVD. The results of this study show that evolution of cardiovascular mortality over time does not correlate proportionally with evolution of availability of dairy fat for consumption. In this regard, it would not be appropriate to draw conclusions based on a single risk factor such as dairy fat for its rich SF content, coinciding with results published by O’Sullivan et al. that when examining consumption of dairy products as a natural and key food group typically high in this fatty acids found no significant statistical association with mortality due to CVD [RR 0.87 (0.62; 1.20)] [20]. Likewise, Soedamah-Muthu et al. found no significant association between milk consumption and total mortality [RR per 200 ml/d 0.99 (0.95; 1.03)] [21]. The analysis of consumption patterns of meat, vegetable and dairy fats in countries with high and low cardiovascular mortality did not allow categorical statements such as ones observed in the past 10. Even though countries with low mortality showed higher availability of vegetable fat and countries with high mortality exhibit higher availability of animal fat for consumption, no particular pattern was observed for dairy fat. It is essential to consider dairy fat consumption in the global context of the evolution of different CVD risk factors. It is a complex nutrient whose beneficial effects have been proven on cardiovascular health. A meta-analysis conducted by Elwood et al., showed a reduction of 10% to 15% in the incidence of coronary heart disease in subjects who reported greater consumption of milk compared to those of lower consumption [14]. Another meta-analysis subsequently published by the same group showed decreased risk of coronary heart disease incidence in the group with higher consumption of milk compared to those with lower consumption [0.92 (0.80; 0.99)] [15].On the other hand, the dairy food matrix may be just as important as its individual components, as it would condition dairy fat velocity of digestibility, determining a different metabolic effect on postprandial triglycerides, affecting bioavailability of dairy fat depending on sub type of dairy product [7, 22-23]. Some limitation on this study should be mentioned: the study type which for its characteristics does not contemplate multiple risk factors that can influence CVD, whilst by themselves they do not allow to prove cause-effect relationship between these two variables. While randomized control trials represent the best study design to examine dairy consumption effect on cardiovascular health, they are more expensive and require more time in order to relate the exposure to certain diet risk factor and its disease incidence. Other limitation to be mentioned is that the association between availability of dairy fat and mortality due to CVD is analyzed without adjusting for possible confounders which may incidence on cardiovascular mortality, for it is not possible to discard that absence of association relates to the effect of this factors. It should be noted that consumption of dairy fat measured through Balance Sheets does not constitute an effective food intake, but an estimate of the food supply per person available for human consumption. Furthermore, this analysis was based on international statistics and public and reliable sources of information.Analysis of the relationship between dairy consumption and CVD should consider the complexity of this food group with multiple nutrients implicated in cardiovascular function under mechanisms still not fully elucidated but that transcend the SF of dairy fat [23]. Dairy consumption contributes to a significant share of calcium, magnesium, phosphorus and potassium, essential minerals for the management of hypertension, a major risk factor at present [21, 24]. In addition, certain dairy peptides have been identified with beneficial effect on blood pressure by inhibiting angiotensin converting enzyme [25].The behavioural and modifiable character of the diet as a risk factor offers the prospect of acting positively. The multi factorial nature of CVD makes necessary that action strategies for prevention and their control be comprehensive, guiding efforts not only towards restricting SF to <10% of daily energy intake, but also to the inclusion of 400-500 g of fruits and vegetables a day, regular consumption of fish and control of sodium chloride less than 5 g per day, as part of a physically active lifestyle [8]. In this context, the consumption of dairy products should be encouraged, by virtue of its many health benefits.
5. Conclusions
- In this study we found no statistically significant correlation between availability of dairy fat for consumption and mortality due to CVD. The evolution of cardiovascular mortality over time and its multi factorial nature makes necessary comprehensive strategies for management of cardiovascular health. Dairy foods are complex and many mechanisms have been described by which their consumption may manage cardiovascular health, regardless of fat content.
ACKNOWLEDGEMENTS
- We would like to thank José Boggia MD, PhD for his suggestions and review of the manuscript. We acknowledge publication support by the School of Nutrition, University of the Republic, Uruguay.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML