-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Food and Public Health
p-ISSN: 2162-9412 e-ISSN: 2162-8440
2015; 5(5): 157-163
doi:10.5923/j.fph.20150505.02
Body Mass Index and Blood Pressure in a Semi-urban Community in Ota, Nigeria
Israel Sunmola Afolabi1, 2, Shalom Nwodo Chinedu1, 2, Emeka E. J. Iweala1, 2, Olubanke O. Ogunlana1, 2, Dominic E. Azuh2, 3
1Biological Sciences Department, Covenant University, Canaan land, Ota, Nigeria
2Covenant University Public Health and Well Being Research Group (CUPWERG)
3Economics and Development Studies Department, Covenant University, Canaan land, Ota, Nigeria
Correspondence to: Israel Sunmola Afolabi, Biological Sciences Department, Covenant University, Canaan land, Ota, Nigeria.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This study was designed to establish the relationship between body mass index (BMI) and blood pressure (BP) in an increasingly industrialised town in Nigeria due to the rising prevalence of hypertension in non-industrialised countries. Factors associated with BMI and BP levels were determined in three hundred adult male and female subjects in Ota community of Ogun State, Nigeria. The levels of the overweight among the male and female subjects were 53.03% and 47.37% respectively. The levels of hypertensive male and female subjects were 40.91% and 35.34% respectively. The overweight and underweight among the hypertensive male were 54.29% and 0% respectively; while the overweight and underweight among the hypertensive female were 42.86% and 28.57% respectively. Hypertension among the overweight, and hypotension among the underweight, are major health concern in Ota that requires intensive medical care.
Keywords: Body mass index, Overweight, Underweight, Age, Diastolic, Systolic, Blood pressure, Hypertension, Hypotension, Gender, Health
Cite this paper: Israel Sunmola Afolabi, Shalom Nwodo Chinedu, Emeka E. J. Iweala, Olubanke O. Ogunlana, Dominic E. Azuh, Body Mass Index and Blood Pressure in a Semi-urban Community in Ota, Nigeria, Food and Public Health, Vol. 5 No. 5, 2015, pp. 157-163. doi: 10.5923/j.fph.20150505.02.
1. Introduction
- High blood pressure (BP) is a leading cause of cardiovascular diseases. The increasing prevalence of cardiovascular diseases is putting a tremendous pressure on already overburdened resources in non-industrialised countries and reflects on the high prevalence of cardiovascular diseases [1, 2]. There are many uncontrollable risk factors that contribute to high BP - such as increase in age, race, heredity, and gender. However, there are some controllable factors, like the weight gain and obesity, stress levels, sodium intake, physical inactivity and certain drugs intake [2]. Understanding the function and proper management of the heart is essential to developing efficient strategies for controlling hypertension. The heart is composed of two independent pumping systems, one on the right side, and the other on the left. Each has two chambers, an atrium and a ventricle. The ventricles are the major pumps in the heart [3]. The left ventricle is the strongest of the heart pumps. Its thicker muscles need to perform contractions powerful enough to force the blood to all parts of the body. This strong contraction produces systolic BP. On the other hand, the diastolic BP is measured when the left ventricle relaxes to refill the heart with blood between the beats [3].High body mass index (BMI) could influence positively and to be independently associated with morbidity and mortality from hypertension and other chronic diseases [4]. Despite a growing burden of obesity and hypertension in developing countries, there is limited information on the contribution of BMI to BP in these populations [5]. Positive associations between body mass and BP have been documented [5]. This relationship, however, is not sufficiently explored among lean populations in Africa. The relationship between BMI and hypertension is of particular interest to developing countries because it has being observed rise cardiovascular mortality among lean hypertensive subjects. The volume of researches on cardiovascular diseases, as well as, risk factors associated with them is extremely low in Africa [5]. Therefore, this work was designed to further establish the relationship between BMI and BP in an increasingly industrialised Ota town, near Lagos, Nigeria. Ota is a town located in Addo-Odo/Ota local government area of Ogun State, Nigeria.
2. Methods
- BP was measured by six medically trained personnel with the aid of mercury sphygmomanometer. BMI and BP of three hundred (ninety-nine (99) adult male and two hundred and one (201) adult female) subjects were analysed. The subjects with one or both of the systolic (SBP ≥ 140/90 mm /Hg) and diastolic (DBP ≤ 90/60 mm Hg) were considered hypertensive and hypotensive, respectively [6]. Subjects with BP between the two values were considered normal as described by Tesfaye et al. [5]. The number of subjects whose BP were classified into each categories were counted and expressed as percentages of the total number of subjects in male and female. Also, the number of subjects with impaired systolic, diastolic and both BP were estimated and expressed as percentages of the total number of subjects with impaired BP. BMI was determined by physically measuring their weight (kg) and height (meter) with the aid of a C-ProduckTM weighing scale and meter rule respectively. The BMI was thereafter calculated using the formular: BMI (kg/m2) = weight (kg)/ height2 (m2). The subjects with BMI of 18.5-25, <18.5 and >25.0 Kg/m2 were classified as normal weight, underweight and overweight respectively following earlier classification of [6]. The number of subjects whose weight were classified into each categories were counted and expressed as percentages of the total number of subjects in male and female. Ethical clearance for the study was obtained from Ethical Committee in Covenant University and Covenant University Teaching Hospital, Ota, Ogun State, Nigeria. We adhered to the required ethical conducts throughout the study period. The results obtained were subjected to statistical calculation using megastat statistical software to obtain the appropriate mean, standard deviation, and correlation matrix between the parameters.
3. Results
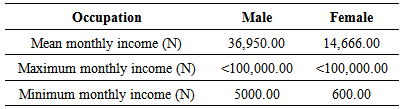
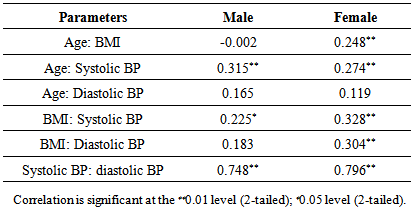
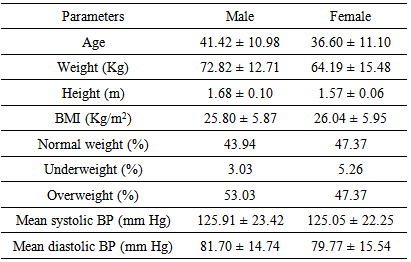
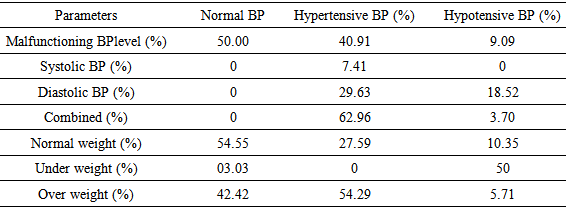
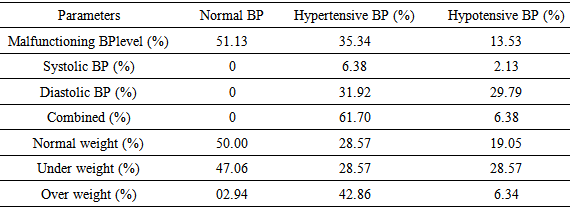
- The income statuses of the subjects are indicated in Table 1 while Figure 1 indicates the types of occupation of subjects. The levels of correlation between age and BMI, systolic BP and diastolic BP, as well as BMI and BP are indicated in Table 2. A significant positive correlation was observed between systolic and diastolic BP (0.748) in male subjects. In the same way, a significant positive correlation was observed between age and the systolic BP (0.315); BMI and diastolic BP (0.183); and BMI and the systolic BP (0.225) between the male subjects (Table 2). There was no significant correlation between BMI and age (-0.002); and also between age and diastolic BP (0.165) in male subjects. There was positive correlation between age and BMI (0.248); and between systolic and diastolic BP (0.796) in female subjects (Table 2). There was also positive correlation between BMI and diastolic (0.304) and the systolic BP (0.328) in female subjects. There was also positive correlation between age and diastolic (0.119); and the systolic BP (0.274) in female subjects (Table 2). Of the total subjects considered, 53.03% male and 47.37% female were classified overweight (Table 3). However, only 3.03% male and 5.26% female of the entire subjects were classified underweight (Table 3).
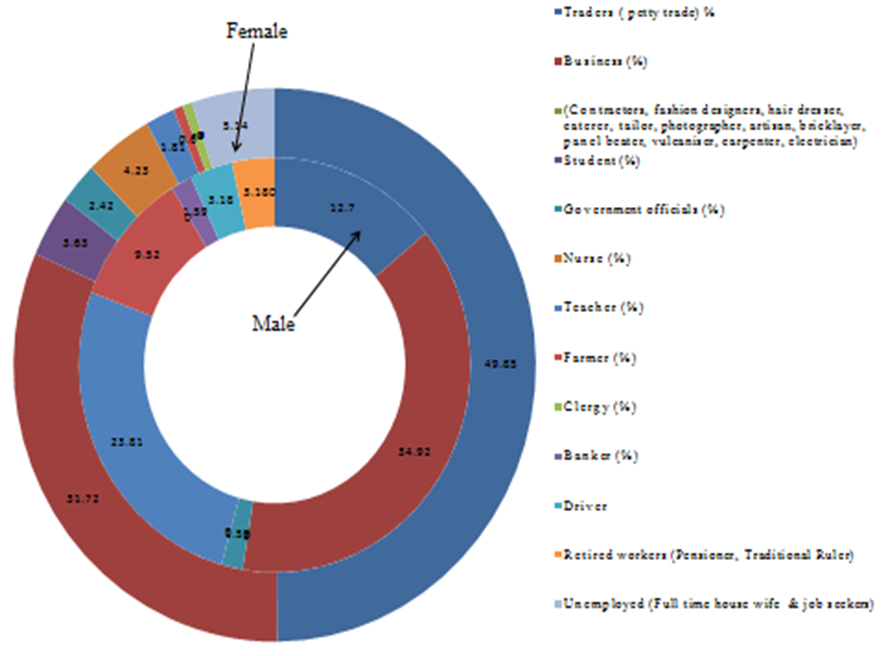 | Figure 1. The occupational distribution of subjects living in Ota, of Ogun State in Nigeria |
|
|
|
|
|
4. Discussion
- The Ota community included in this study encompassed both low and high income people. Six hundred naira (N600.00) and five thousand naira (N5000.00) are the minimum income for the female and male subjects respectively. The maximum income could be over one hundred thousand naira in both genders (Table 1). Business, teaching, petty trading and farming are the major occupation of the male subjects (Figure 1). Artisan, bricklaying, panel beating, tailoring, carpentry, vulcanizing and electrician are the major type of business peculiar to the male subjects (Figure 1). Also, petty trading and business constitute to the major occupation of the female subjects (Figure 1). Fashion designing, hair dressing and catering are the type of business peculiar to the female subjects (Figure 1). The slightly higher female clergy reported in this community may be due to the fact that most of the male clergy possessed other primary job other than the clergy job. There is possibility that the male clergy in this community are doing it as a secondary job. This is an attribute that is peculiar to the new privately Pentecostal churches.There is no association between aging and BMI in the male subjects. On the other hand, there is association (r = 0.248) between aging and BMI in female subjects (Table 2). Also, the BMI level is more critical in the determination of the systolic BP of adult male than that of the diastolic BP. This trend was also the same in adult female subjects. The relationship between BMI and BP level in adult female was more pronounced than in the male subjects (Table 2). Our finding is in agreement with the earlier report [5]. Aging also affect the level of systolic BP than the diastolic BP among adult male and female. However, the correlation between aging and BP (systolic and diastolic) was more accentuated in male than their female subjects (Table 2). Both types of BP are expected to increase with increase in aging [7-9].Our earlier finding on the health status of people in this same community in Ota reveals the extent of diabetes in this community where the females were more obese, and had lower random blood glucose levels and body mass index than the males [10, 11]. The correlation between body mass index and waist circumference to evaluate the health status of the indigenes of the community has been used to proper health awareness and in public health intervention programmes [12].In this study, overweight is a major concern in Ota community since 53.03% and 47.37% of its male and female subjects were overweight (Table 3). This may be attributed to their eating habits coupled with the sedentary lifestyle of the people [13]. Especially because the principal professional activities reported was teaching and trading (often associated with sitting long hours) [14]. The overweight was higher in male than in female subjects (Table 3). This may be attributed to the more laborious muscle (or body) building type of occupation (bricklayer, panel beater, vulcaniser, carpenter and electrician) performed by them (Figure 1). Another probable reason may be due to the higher consumption of high calorie foods or drinks like alcohol and cigarette smoking in the male subjects [15, 16]. Our earlier report on a similar study supports the use waist circumference as a reliable indicator for overweight adults and obesity and not for underweight adults [12]. The use of both BMI and waist circumference individually as a predictor of obesity and cadiovascular diseases have their relative advantages and limitations. There is the limitation of BMI does not reflect the changes associated with age, sex and bone mass density. Moreso, BMI may be gender bias since it does not take into account the body fat mass, which varies between men and women [17-19]. The earlier reported combination of BMI and waist circumference provides a more reliable prediction of obesity and cardiovascular related diseases than using the individual indices had also been disputed [20]. That notwithstanding, BMI is still the most widely used indices globally for measuring health status.Regular physical activity and a high intake of dietary non-starch polysaccharides /fibre were some of the earlier established protective factors against obesity [13, 21]. Obesity is associated to sedentary lifestyle, high intake of energy-dense and micronutrient-poor foods [13]. Increased communications about healthy eating and physical activity; and improved health services are strategies that may be implemented at preventing overweight and obesity in such community [13]. Hypertension, an increase in BP precedes the gain of weight [22]. Increases in body weight (body mass index) affect the activity of adipocytes and the secretion of adipokines (Leptin and adiponectin) [22]. These adipokines also affects the development of hypertension and other cardiovascular diseases [22]. The coordinated roles of ghrelin and leptin in the modulation of the weight changes had also been reported [23]. These two hormones secreted in the stomach and the small intestine modulate weight changes by controls human appetite for foods via the leptin-melanocortin pathway [24, 25]. The type of hypertension that can be generated by excess increase in weight is common in human that has salt sensitivity which can occur through increase in sympathetic activity mediated by the sympathetic nervous system. The regulation of the energy metabolism of the resting metabolic rate in human can be sometimes controlled by the sympathetic nervous system [26, 27]. Blood pressure increases with higher levels of dietary salt intake that increases the risk of cardiovascular disease [28, 29]. Physiological conditions such as cholesterol, triglycerides, catecholamine, plasma renin, plasma aldosterone, plasma adrenaline and plasma noradrenaline increases with decrease in hypertension due low salt intake and vice-versa [30-32]. Consumption of too much dietary salt increases the mass of the left ventricle, reverses the flexibility of the conduit arteries by thickening and stiffening it. Thus, the radius of the resistance arteries, including the coronary and renal arteries is reduced. The tendency for platelets to aggregate also increases with high dietary salt intake [33]. The increase in blood pressure with high dietary salt intake had also been attributed to the inability of kidney to ingest and excrete it when taken at a level above the 1 g /day that is far less than the salt intake levels in industrialised countries [34]. This normal human kidney capacity to process and excrete sodium that is commonly from dietary salt reduces with age. Increase in the capacity of plasma to inhibit Na+-K+-ATPase has also been implicated in an attempt to account for the mechanism of salt induced hypertension [34]. It raises blood pressure by inhibiting the sodium-calcium exchange pumps in the smooth muscles around the heart. These effects leading to hypertension can be remedied by living in silent and less stressful environment that is peculiar to the rural areas [34]. The involvement of insulin resistance and β-adrenergic systems in the development of overweight in hypertensive patients had been reported [26, 27, 35]. Gender of overweight hypertensive subjects determines their biochemical status [16]. High fasting lipoprotein and lower diurnal triglycerides have been reported in female overweight hypertensive subjects compared to male overweight hypertensive subjects [16]. These biochemical differences could be responsible for the differences observed between overweight hypertensive male and female subjects in the present study.The incidence of hypertension was bigger in male than female subjects (Table 4 and 5). These results are in agreement with earlier study [7] and showed that hypertension is therefore, a major health concern, specially, to male subjects in Ota community.The high level of high BP been reported in this study may be due to the increasing industrialization of Ota town as a result of its proximity to Lagos, a major metropolitan city in Nigeria whose population is highly exposed to unhealthy urban lifestyles such as excessive consumption of energy-dense foods and poor environment due to air pollution from frequent use of automobiles. The reverse is the case in some less polluted remote part of Africa whose population are having lower BP levels [1, 36]. Diastolic BP is the lowest BP measured in the arteries. It occurs when the heart muscle is relaxed between two contractions [7]. Systolic BP is the highest BP, which is a measure of the contraction of the chambers of the heart. It occurs when the heart contracts with each heartbeat [7]. Systolic heart failure typically occurs in men between the ages of 50 - 70 years who have earlier had a heart attack [3]. The failure of both the systolic and the diastolic BP was almost equally pronounced in hypertensive male (Table 4) and female (Table 5). Thus, the hypertension cases in this community are largely due to the failure of both the left and right ventricles of the heart in both genders [3, 37]. Our report is slightly different from earlier reports that linked men to have twice the risk level of developing blood-pumping (systolic) problems compared to women [38]. The level of subjects with malfunctioned heart due to diastolic BP was also high in both sexes. In fact, the level was more pronounced in women with hypotensive cases (Table 5). Thus, the high hypertensive cases in this community could (because there are a lot of factors that contribute to hypotension) be attributed to a lesser extent to the inability of the hearts’ left ventricle to relax and filled the heart with blood due to stiffness of its muscles [3, 38]. The hypotensive cases are clearly due to diastolic heart failure in both genders in this study (Table 4 and 5). We suggest further validation this claim with image analysis to evaluate heart morphology. Our data indicates that overweight subjects are the most susceptible to hypertension; while also revealing for the first time that the underweight subjects are most susceptible to hypotension. Our report is slightly different from earlier reports that linked both high systolic and diastolic BP to the overweight (high BMI) subjects [4, 39]. Efforts are been made to account for the mechanisms to support the way high BMI increases the risk of high BP [1]. The point of control of the haemoglobin metabolism, the sympathetic nervous system, vascular dysfunction and insulin resistance are of recent been implicated [40-42]. Increase in child weight at birth and provision of high quality early-life diet to children may, in part, account for the manifestation of low BP at adulthood [43]. The possibilities of various dietary factors, such as reductions in the salt content of food, have also been considered in preventing hypertension [43, 44]. Other nutritional means of lowering blood pressure are the increase intake of high protein diets, traditional diet that consists of a variety of fermented soybean products and vegetable based foods, which are rich sources of bioactive compounds (such as hesperiding) capable of promoting cardiovascular health [45-49], and abstinence from the consumption of processed red meat treated with high sodium and nitrites [21, 43, 50, 51]. Hypertension and overweight could therefore be subjects of major public health concern in Ota, showing that the intensive medical education about ways to alleviate or prevent hypertension is therefore essential in this region.
ACKNOWLEDGEMENTS
- Authors appreciate the support of staff of Covenant University teaching hospital and Addo-Odo local government officials during the data collection. We also appreciate the traditional head of Iyesin, and Ilogbo communities in Ota to facilitate our access to their citizen.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML