-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
World Environment
p-ISSN: 2163-1573 e-ISSN: 2163-1581
2013; 3(3): 71-76
doi:10.5923/j.env.20130303.01
Spatial Incidence of Tuberculosis in Enugu State, Nigeria
Igu N. I1, 2, Enete I. C2, Olaniyan F. A3
1Environment Department, University of York, UK, Y010 5DD
2Department of Geography and Meteorology, Nnamdi Azikiwe University, Awka, Nigeria
3Department of Geography, University of Ibadan, Nigeria
Correspondence to: Igu N. I, Environment Department, University of York, UK, Y010 5DD.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Tuberculosis is described as a global emergency; and is found more in the developing world. In this light, a retrospective study of the incidence of the disease was conducted in Enugu. The study focused on understanding if urbanization affects/promotes the disease, the most vulnerable; the age bracket that has it more, the gender differentials, among others. More urbanized centres were found to have a higher incidence and further analysis using Pearson product moment correlation coefficient showed a positive non-significant correlation of 0.309. Males were found to have a cumulatively higher incidence than the females with 57.4% and 42.6% occurrence respectively. Ages 25-34 years was found to have the highest percentage occurrence of 37.5%, while 0-14years with 1.7% occurrence was the least. Optimal location of more DOT centres was suggested to handle stigmatization, reluctance and inconsistency in treatment, which were identified contributory factors of the disease incidence, in the study area.
Keywords: Tuberculosis, Dots, New-smear Positive, Enugu
Cite this paper: Igu N. I, Enete I. C, Olaniyan F. A, Spatial Incidence of Tuberculosis in Enugu State, Nigeria, World Environment, Vol. 3 No. 3, 2013, pp. 71-76. doi: 10.5923/j.env.20130303.01.
Article Outline
1. Introduction
- Tuberculosis is a chronic, infectious disease caused mainly by the bacteria generally referred to as ‘mycobacterium tuberculosis complex’. Causing a quarter of all avoidable deaths, tuberculosis (TB) is the second largest cause of death from an infectious disease worldwide (after HIV), and is among the top ten causes of illness, death and disability in terms of years of healthy life lost overall.It is seen as both a non-vectored as well as a chronic disease, and is promoted or inhibited as a result of factors like economic status, hygiene, congestion, migration, lifestyle and habits like smoking, as well as attitudes towards treatments.Tuberculosis being an infectious disease, cannot be contained by political boundaries or more strict border controls. Even though the incidence is not much in Europe and North America, it cannot yet be controlled in the industrialized countries unless it is sharply reduced in the developing countries of Asia, Africa and Latin America. This is attributed to recent increases in human migration that have rapidly mixed infected with uninfected communities[1]. Because of its ease of transmission, tuberculosis anywhere in the world is a concern for everyone. While it remained a major health problem in developing countries, from the mid-1980s, the advent and spread of HIV, the virus that leads to AIDS, paved the way for tuberculosis to stage a comeback in the industrialized countries, and thus on the world scene. This is even more worrisome now that the prevalence of multi-drug resistant tuberculosis is increasing throughout the world[2], with an estimated 440,000 cases worldwide in 2008[3]. Infecting eight million new victims a year, tuberculosis also has a deadly link with AIDS, and this largely contributes to the increasing trend of the disease; and particularly so in sub-Saharan Africa, where the synergy between HIV/AIDS and tuberculosis is a grave problem[4].It affects both the male and the female gender alike, but is seen to be higher in males after adolescence[5]. Globally, there are 1.7 times as many male pulmonary tuberculosis cases reported annually as female cases[5] and this is because tobacco smoking and other such lifestyles is prevalent almost exclusively among men. Although women may enjoy some kind of protection against tuberculosis, this protection may be offset by biological and sociological vulnerabilities at certain life stages.Historically, tuberculosis has been associated with economic hardship, urbanization and other socio-economic factors. The evidence suggests that the prevalence of tuberculosis is disproportionately high among poor countries and among disadvantaged groups within countries; and equally seen to be associated with constrained macroeconomic conditions and periods of economic transition. Considering the multi-dimensional nature of poverty, its impact on the risk of tuberculosis might therefore best be accessed by looking independently at several types of deprivation such as income, food, housing, knowledge, power and access. The factors that make the poor more vulnerable to tuberculosis also make them more vulnerable to poor living conditions, malnutrition and other forms of illness, all of which may further exacerbate the risk of getting tuberculosis[6]; estimated that among the poor, tuberculosis could result in a loss of 20-30% of a household’s annual wages. It could however, be hypothesized that tuberculosis can cause a relatively poor individual or household to fall into poverty, even if the decline in economic status is only temporarily.The patients diagnosed with the disease, are referred to as the new smear-positive cases and the DOT strategy is used in the treatment. Globally, the DOTS (directly observed treatment, short-course strategy) have been recognized as the best cost-effective approach to tuberculosis control, to reduce the disease burden and to reduce the spread of infection[7]. Despite the success of this program among others, tuberculosis incidence and mortality are not falling rapidly enough to meet WHO targets, and in some areas, particularly in parts of Asia and throughout sub-Saharan Africa, they continue to climb.
2. Conceptual Framework
- Social inequities in health, buttresses the systematic differences in health status between different socioeconomic groups. Within any country or region, difference in health can be observed across the population. Genetic and constitutional variations ensure that the health of individuals varies, as it does for any other physical characteristic. The prevalence of ill health also differs between age groups with older people tending to be sicker than younger people, because of the natural ageing process[8]. Biologically also, variations also exist between the male and female gender with respect to which among them exhibit an advantage in survival.Tuberculosis in like manner, is a social disease, and as such healthcare-seeking behaviour among patients is influenced by gender, age, socioeconomic and social status, type of illness, access to services, and perceived quality of the service[9], which often interacts in a complex web. People can be confused as to the implications of tuberculosis symptoms, costs of transportation, the social stigma, the high cost of medication, and perceptions of patients about clinic facilities as unfriendly, and all these contribute to the complexity of the disease[10]. Understanding the aforementioned becomes then a necessity, as tuberculosis is one of the major public health problems in the world today, and no other disease has so much sociological, economic and health significance as tuberculosis[11].This study is focused on studying the incidence of the disease in Enugu, with a view to address the above issues while seeking to understand the stratification of patients along their gender, geography and socioeconomic status.
3. Study Area
- Enugu state is located between latitudes
 and
and  and longitudes
and longitudes  and
and  It has a population of 3,161,295 (NPC (National Population Commission), 1991) within a total area of 12,791sq.kms. This gives a population density of about 214 persons per sq km which is high when compared with the average national density of about 96 persons per sq km. expectedly; the population concentration is highest in urban centres than in the rural areas; and an average population density of 254 persons per sq km across the state. The state is situated on the highland of the Awgu, Udi and Nsukka hills to the east as well as Oji-river to the west. It is made up of a total of seventeen local government areas and lies in the region of the tropical rainforest with an annual rainfall range of between 152- 203cm, and temperature range of between 32 ⁰C and 37⁰C.
It has a population of 3,161,295 (NPC (National Population Commission), 1991) within a total area of 12,791sq.kms. This gives a population density of about 214 persons per sq km which is high when compared with the average national density of about 96 persons per sq km. expectedly; the population concentration is highest in urban centres than in the rural areas; and an average population density of 254 persons per sq km across the state. The state is situated on the highland of the Awgu, Udi and Nsukka hills to the east as well as Oji-river to the west. It is made up of a total of seventeen local government areas and lies in the region of the tropical rainforest with an annual rainfall range of between 152- 203cm, and temperature range of between 32 ⁰C and 37⁰C.4. Materials and Methods
- Data for this study were collected from the Enugu state ministry of Health as well as from interviews conducted at the DOT centres in the area of study. The disease incidence data for the seventeen local government areas (LGAs) in the state were gotten from the quarterly report (1st – 4th quarters) of the new smear-positive cases from 1995-2005.Population figures in this study are used to determine urbanization. L.G.As with high population figures were taken as more urbanized environments while lower population figures stood for rural L.G.As or L.G.As with lesser urbanized centres. 1991 population figure was used in the study since that was the available data (the next population census in the country was conducted in 2006 and was still being processed as at the time of the study). The 1991 census population figure was used to determine the proportion of population that is urban and then projected till 2005 at 2.83% per annum growth rate[12]. In determining the relationship between urbanization and disease incidence the Pearson Product Moment Correlation (PPMC) was employed. The value of r coefficient ranges from –1 < r < The higher the r coefficient, the stronger the nature of the relationship between observations. Coefficients close to 0.0 represent a weak relationship. Coefficients close to 1.0 or -1.0 represent a strong relationship. To test the differences in the incidence of tuberculosis between men and women the chi-square test of independence was used. The chi-square test of independence is basically a nonparametric version of the interaction term in ANOVA. The mean plots derived from Analysis of variance (ANOVA) were used to graphically depict variation in incidence of tuberculosis across space.
5. Discussion
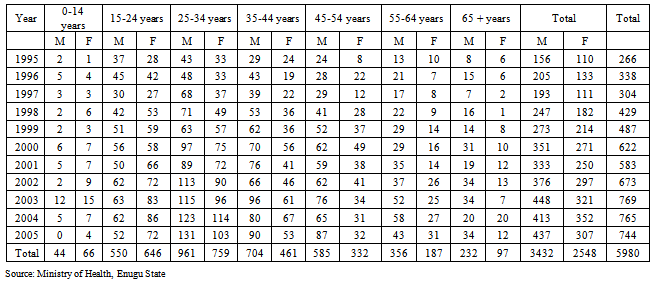
- In understanding the variation across space, the incidence data of 2000-2005 (table 1) showed that Enugu North had the highest incidence rate, followed by Nsukka and Igbo-eze north local government areas with incidence rate totals of 1001, 815 and 700 respectively; while Nkanu west and Nkanu east had the least total incidences of 27 and 18 respectively. The mean plots in fig. 1 graphically depict the degree of variation in incidence of tuberculosis in the study area.
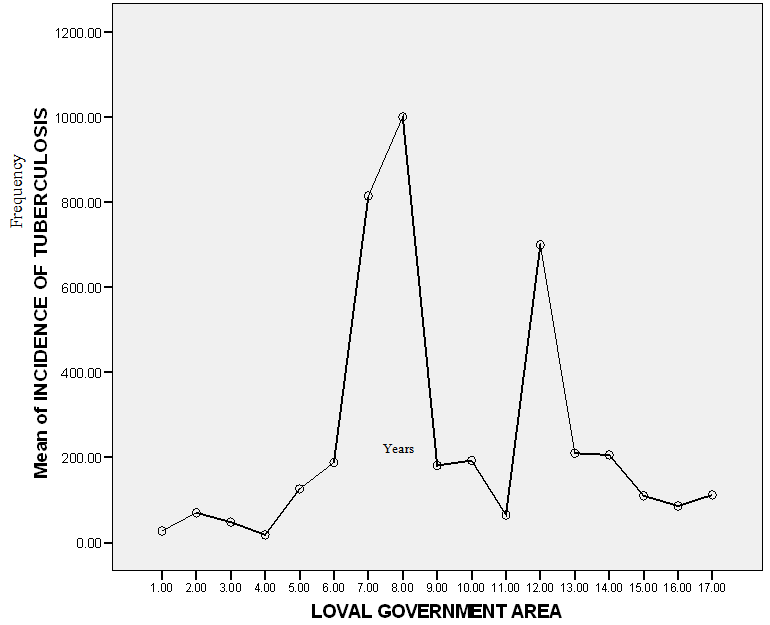 | Figure 1. Mean plot showing the degree of variation of the disease incidence |
|
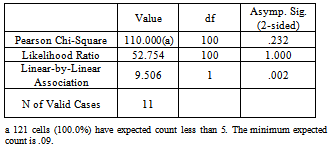
5.1. Sex of Patients
- Patterns of health and illness in women and men show marked differences. Men and women experience different health risks that stem from their biological differences as well as social, economic and cultural roles[14]. The study revealed a higher incidence for females from ages 0-14 and 15-24 years; while for ages 25-65 years and above, the incidence for males outnumbered that of the females. However, males were seen to have a cumulatively higher incidence than the females (table 3), with 57.4% and 42.6% occurrence respectively. This supports the global view that more men are diagnosed with tuberculosis than women[15, 16, and 17]. This is because men are more widely exposed to other people with infectious TB, as a result of their greater social interaction outside the home. Results of chi-square test of independence confirm this assertion. A chi-square test of independence was calculated comparing the incidence of tuberculosis for men and women. A significant result was found (X2(1) =23.2, p<.05). Men are more likely to have tuberculosis (52.7%) than women (47.3%) (Appendix 1).
|
5.2. Age of Patients
- Age has a very significant role to play in the issues of health. It determines to a great extent the issue of health, since the level of exposure of the bacteria, level of progression from infection to disease amongst others, vary with age. The incidence data in the study shows ages 25-34 years as having the highest percentage of 37.5%. This was followed by 20% for ages 15-24, and 17.5% for 35-44years. 45-54years age range had 13.3%, 65years and above had 2.5%, while 0-14years range had 1.7% (table 4).This could be explained by the degree of exposure that each age range has. The working population age range (15-54years) recorded a higher percentage incidence, while the dependents which made up the remaining category had the lower percentage occurrence. This further buttresses the fact that tuberculosis affects mostly people in their economically productive ages. The high level of infection at this stage could be attributed to the varying exposures and environmental insults that are highest at this stage.
|
6. Conclusions and Recommendations
- In attempting to understand the disease trend in the state, it was found that the incidence varied from year to year and across space. Many of the patients for one (behavioural) reason or the other preferred accessing DOT centres that were farther from them because of a perceived better health care, while for others, it was to avoid being stigmatized. This, in effect, makes most of them not to complete their stipulated duration of treatment, as they get discouraged after some time, due to enormous transport cost. This has the implication of facilitating multi-drug resistant type of tuberculosis, which is more deadly as well as more infectious. Tuberculosis was seen to affect both sexes in the study, with males having more of the occurrence. Both sexes as a result of the disease are vulnerable to a lot of things like frequent sickness, death, social and economic consequences. The study revealed the male folk as having more of the incidence; this in effect leads to distress on their part because of loss of income and inability to contribute significantly to household upkeep of which he is the head.The disease incidence was also found to be high particularly among those between the ages of 15 and 54, who constitute the work force and wage earners. This then goes on to affect the economy of the state and the nation at large both now and in future if not tackled. This is supported by reports from Thailand and India as follows: “one estimate, projects that the Thai economy will lose the equivalent or US $7 billion by the year 2015, solely to tuberculosis sickness and deaths. In India, the estimated loss of economic output due to tuberculosis deaths reaches more than US $370 million every year”[18].There is every need for the formal and informal sector to unanimously contribute to the combating of the disease through matching and forceful efforts.
APPENDIX 1
- Chi-Square Tests
References
| [1] | World Health Organization (1993). 46th year, no 4 July- August, Geneva. |
| [2] | World Health Organization (2008). Anti-Tuberculosis drug resistance in the world. Report No.4, Geneva, Switzerland. |
| [3] | World Health Organization (2010). Multi drug and extensively drug-resistant TB (M/XDR-TB): 2010 global report on surveillance and response. Geneva. |
| [4] | Cosmas, I. and Gagneux, S. (2009). The past and future of tuberculosis research. PLoS Pathog 5 (10): e1000600. Doi: 10.1371/journal.ppat.1000600. |
| [5] | World Health Organization (2002). Gender and Health, Geneva, Switzerland. |
| [6] | Ahlburg, D. A (2002). The economic impacts of tuberculosis. The STOP TB Initiative 2000 series. Geneva, Switzerland. |
| [7] | Park, K (2000). Park’s textbook of preventive and social medicine, seventeenth edition. M/s Banarsidas Bhanot publishers, India. |
| [8] | Dahlgren G, Whitehead M (2007). European strategies for tackling social inequalities in health: Levelling up Part 2. Copenhagen, WHO Regional Office for Europe (Studies on social and economic determinants of population health, No 3). |
| [9] | Tipping, G and Segall, M. Health care seeking behaviour in developing countries: an annotated bibliography and literature review. Brighton: Institute of Development Studies, 1995. (Development bibliography no. 12). |
| [10] | Rubel, A.J, Garro, L.C. Social and cultural factors in the successful control of tuberculosis. Public Health Rep. 1992; 107: 626-36. |
| [11] | Tungdim,M.G, and Kapoor, S. (2010). Gender differentials in tuberculosis: impact of socio-economic and cultural factors among the tribals of northeast India. The open social science journal, 3, 68-74. |
| [12] | N P C (1991) in National and state population projections. Nigeria population census 1991 Analysis Vol 6, National Population Commission, Abuja, Nigeria, 2002. |
| [13] | Igu, N.I (2007). Geographical analysis of tuberculosis in Enugu state, Nigeria. Unpublished M.Sc thesis, University of Ibadan, Ibadan. |
| [14] | Doyal, L (1998). Sex, gender and health preliminary conceptual framework, in Diwan A, Thornson A, Winkwist A.(eds): Gender and tuberculosis. Nordic school of public health, Gotebor; 1998: 29-40. |
| [15] | Rao, S. (2009). Tuberculosis and patient gender: An analysis and its implications in tuberculosis control. Lung India. official publication of Indian chest society, April-June; 26(2): 46-47.doi:10.4103/0970-2113.48897. |
| [16] | Sharma, P.R, Jain, S, Bamezai, R.N.K and Tiwari, P.K (2010). Increased prevalence of pulmonary tuberculosis in male adults in Shariya tribe of India: A revised survey. Indian J. Community Med. April, 35 (2): 267-271.doi:10.4103/0970-0218.66887. |
| [17] | World Health Organization (2008). Global tuberculosis control: surveillance, planning, financing, Geneva. |
| [18] | World Health Organization (1996). Groups at Risk: WHO report on the tuberculosis epidemic, Geneva. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML