-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Education
p-ISSN: 2162-9463 e-ISSN: 2162-8467
2017; 7(4): 59-66
doi:10.5923/j.edu.20170704.01

Effective Mode of Learning: Knowledge Gain through Problem Solving Exercise during Medicine Tutorial Session
Nan Nitra Than1, Htoo Htoo Kyaw Soe1, Senthil Kumar Palaniappan2, Soe Moe1
1Department of Community Medicine, Melaka-Manipal Medical College, Melaka, Malaysia
2Department of Medicine, University Hospitals of Leicester, Leicester, UK
Correspondence to: Htoo Htoo Kyaw Soe, Department of Community Medicine, Melaka-Manipal Medical College, Melaka, Malaysia.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Problem solving exercise has been used in clinical education of its potential in providing not only to make clinical judgments but also offers an alternative paradigm for accessing the knowledge of medicine. This study describes an overview of problem solving exercise in medical education and its applicability in teaching large groups of students in our medical institution. The main objectives of this study were to assess the student’s preference and acceptance of problem solving exercise (PSE) and to compare pre and post knowledge scores. The author reviewed the feedback records responded by third-year medical students after the problem solving exercise sessions during medicine tutorial. Quantitative and qualitative mixed design were used. Data were analyzed by using SPSS software for quantitative method. There is a significant difference of knowledge scores between the pre-test and post-test results after evaluating the outcome of hypertension related case scenario assessment. Qualitative analysis on the reasons showed the strengths and weakness of problem solving exercise program. The results were considered in light of future educational methods that underlies the problem solving exercise and its basic research. We concluded that problem solving exercise is the useful teaching learning method in undergraduate medicine professional which achieved higher knowledge gain, a worthwhile experience in clinical practice.
Keywords: Problem solving exercise, Knowledge gain, Learning, Medicine
Cite this paper: Nan Nitra Than, Htoo Htoo Kyaw Soe, Senthil Kumar Palaniappan, Soe Moe, Effective Mode of Learning: Knowledge Gain through Problem Solving Exercise during Medicine Tutorial Session, Education, Vol. 7 No. 4, 2017, pp. 59-66. doi: 10.5923/j.edu.20170704.01.
Article Outline
1. Introduction
- Problem solving is a mental process whereby a person applies and / or transforms knowledge and understanding in order to arrive at a solution to a problem [1]. Problem solving or reasoning processes is distinguished from problem based learning. It is converting an actual current state into a desired future state. In order to solve problems, one needs first of all an understanding or insight into the patient’s problem. This understanding must then be applied in real situation with real patients (or sophisticated simulations), employing all kind of clinical skills and laboratory tests [2]. This means that problem solving is minimal or absent in early stages of a course and becomes more and more important at the end of curriculum. The use of problem solving exercise (PSE) is worthwhile in medical related professionals to help the students improved by using this educational model [3].Problem based learning (PBL) defines method and philosophy involving problem first learning through work in a small groups and independent study [4]. PBL encourages independent learning and deeper understanding of a particular topic [5]. The focus is on effect of problem based learning on knowledge but neglected other aspects of physician competency [6-8]. It prepares students to construct a principled understanding of the issues in the problem case, to apply principles flexibly to problems of varying complexity as opposed to merely tackling individual problems or problems that can easily be solved [9]. The problem-based learning lets prospective teachers create a rich foundation for solving similar or more serious problems in the classroom, prepares them for their future learning [10]. Problem based learning guides students to identify learning issues, that needs to be learned to resolve the problem [11]. There is some important disadvantages to PBL; a tendency of students to jump to diagnostic conclusions and go through medicine textbooks to find out the treatment protocol for the disorder [5].The distinction between two is important. PBL is to develop students’ ability to raise questions; to think and take initiative for their own learning, PSE is to use these insights in order to diagnose and treat real patients [12, 13].In our university, PBL is used as a teaching learning method from first to final year bachelor of medicine and bachelor of surgery (MBBS) program. Knowing advantages of PSE, department of internal medicine, would like to introduce PSE as one of the teaching learning approach earlier in clinical years starting from 3rd year. However, in various medical School, PBL is used for early years like 1st to 4th year and PSE is used for final years. PSE is substituting PBL when the students’ number are increasing. However, in a significant fraction of these sessions, the students will find it more appropriate to enhance focus on clinical reasoning as well as take a problem solving approach (in contrast to traditional PBL tutorial) and faculty members will function as discussants and or resource persons i.e., these will be shaped into problem solving exercises and held in workshop format with a larger number of small groups that are able to listen to and interact each other [14].Core themes for PSE in medicine are breathlessness, chest pain, hypertension, Headache, anemia. One theme is divided into 3 days (Day 1, Day 2, and Day 3) and each section last for 2 hours. Other departments in this University are using PBL only; therefore, it is necessary to evaluate the outcome of PSE in terms of student satisfaction, meeting learning outcome or knowledge gain and teachers’ willingness and readiness for it. However, there is no study to support the acceptance of PSE by lecturer and students and this study tries to fulfill the knowledge gap for future teaching learning activities. Objectives of this study was to find out the student's preference and acceptance of PSE, to compare pre and post knowledge score of students after the session and to explain the reasons for preference in PSE.
2. Methods
- Third-year medical students were included in this study. We used the secondary data with record check list as data collection tools. The study design was a quantitative and qualitative mix design and data analysis was done by using SPSS version 12.
2.1. The Format Used in PSE Model
- The problem solving model for this tutorial teaching session has a four phase process; three for students to follow and one for the facilitator: A. Determination of the problem within groupsa) Gather information b) Identify the problemsB. Plan the solution to the problemsa) Arrange the identified problems b) Select alternative problem solving strategiesc) Select resources to implement the problem’s solutionsC. Implementationa) Apply or implement the plan using the selected solutionsD. Evaluate the plan by facilitator (an outcome analysis of the implemented plan)a) Determine the effectiveness of the planb) Determine the effectiveness of the problem solving process
2.2. Guideline for PSE
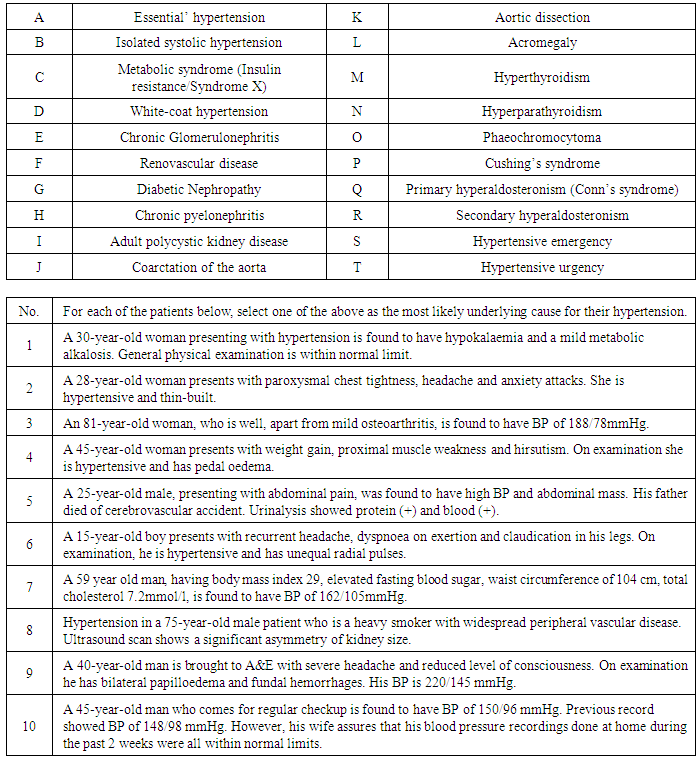
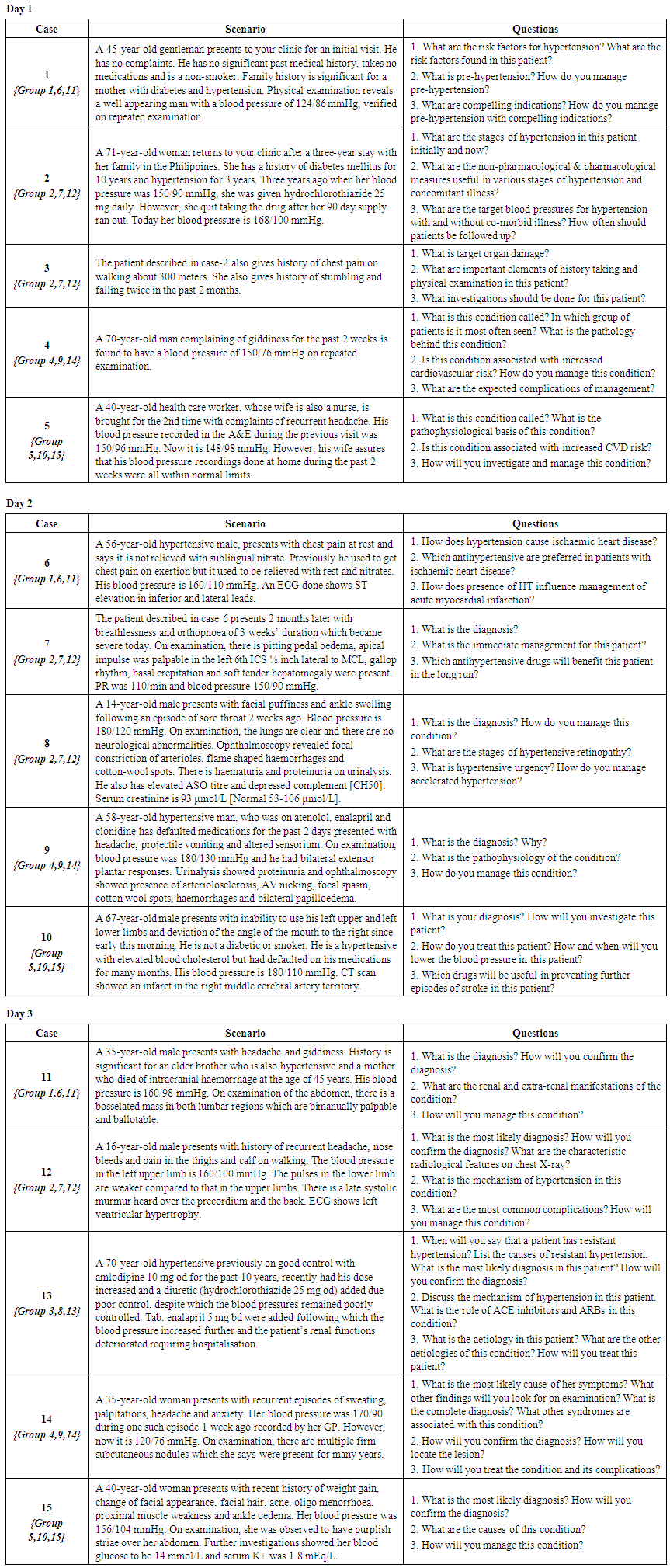
- Pretest questions were distributed before starting this PSE session (On day 1) to find out the knowledge gain of the specific disease condition. The questions for the case of hypertension included 10 questions and there was a table of correct answer to choose for (Table 3: Appendix).The guidelines for this two-hour session were established for the students. Students are divided into 15 groups (9 students each) and received similar problem solving topics with different approach and three questions each to be answered. The topics selected from medicine department were breathlessness, chest pain, hypertension, headache and anemia. Recommended text books for medicine are allowed to use. One theme is divided into three days to discuss (Day 1, Day 2 and Day 3) and each section last for 2 hours. First of all, facilitators distributed a case sheet containing 5 case scenarios of same complaint and asked the students to discuss among themselves for 30 minutes. (Appendix: Table 4)The two-hour session was divided into different segments; (a) distribution and presentation of information that would encourage the students’ understanding of disease of the patient presented, (b) discussion among students to achieve better solution to the problem, (c) presentation of the student’s achievement from the case discussion with power point by using computer and (d) explanation and discussion from facilitators for the specific topics.The time allocated for each section of these segments were divided; 30 minutes for gather information and discussion among them for three questions to answer on each day, 30 minutes for case presentation, 30 minutes for explanation from the facilitator and 30 minutes for question and answer sessions. Each group is responsible for one case scenario to present after discussion. Active participation by the group mates was to be emphasized. The post-test questions included the same questions of pretest and were asked to answer at the end of two hour sessions of presentation (on day 3) and students responded a written feedback for the preference of PBL or PSE with reasons.
3. Results
- A total of 121 third-year medical students participated in this study. All of them had not yet had PSE experience in chest pain, anemia, shortness of breath, hypertension and diabetes mellitus learning themes. The students gave feedback with a written comment about the preference of learning methods (either PBL or PSE) and reasons for their decisions.
3.1. Student’s Preference on PSE
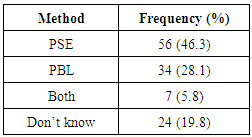
- Table 1 shows the percentage of students who prefer PSE or PBL; fifty-six students (46.3%) showed interest mostly for PSE, 34 students (28.1%) for PBL, 7 students (5.8%) in both PSE and PBL and 24 students (20%).
|
3.2. Knowledge Gain
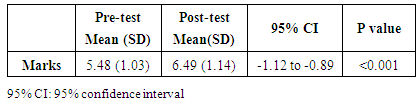
- The pre-test evaluation was done before the start of the session of hypertension PSE and the post test was done after the 2-hour session of PSE. The pre-test and post test results on the selected topic of hypertension showed there was significant difference of mean score between pre-test and post-test marks. The post-test means of marks (mean 6.49) was higher than pre-test (mean 5.48) with 95% CI for difference -1.12 to -0.89 as shown in Table 2.
|
3.3. The Reasons Given by the Students about 2-Hours PSE Session
- Of all 97 students, 81 students gave written reasons for choosing PSE or PBL or both.A. Knowledge gain from lecturersStudents commented on facilitators’ role in conducting PSE and achievement during the session. “All the lecturers gave out their opinion”“Gain a lot of knowledge listening opinions from different lecturers”“A chance to hear opinion from different lecturers, inviting lecturers whom we specialized in a particular field during the sessions makes PSE more interesting” “PSE is more effective and able to gain more information from various lecturers”“If PBL, we don't have chance to learn more things to get to know more about lecturers”.B. Knowledge gain from different aspects of the cases and from lecturersEleven students gave opinions and different aspects on discussing cases during the sessions of PSE; “I can give opinion and discuss more cases with different aspects”“PSE is better than PBL because of better understanding of all the situations” “PSE is better because more discussions could be done can give more knowledge based on the questions asked by other groups & easily differentiate the different diagnosis”, “give us a chance to revise various topics of medicine in an interesting way”“Personally find PSE more useful and we are able to discuss more topics, for a longer time and with guidance of more lecturers”There is one weakness in workload for student and the lecturer;“If lecturer or group member are uncooperative, then session is not effective”“Too much overload to study in a day, but we cannot continuously concentrate throughout PSE in such large group”. One student suggested off for earlier uploading the triggers in Gmail one day earlier. C. Comparing the cases discussed (one case discussion in PBL and many case discussions in PSE)One student compared the discussion of many case discussions in PSE and one case for PBL; “I am able to discuss more detail about one case rather than discussing few different cases together insufficiently” and “PBL is good because it allows us to brainstorm about clinical scenario”.D. The doubts One student gave feedback on the ability to discuss the doubts during two-hour session; “PSE has closer interaction with lecturers, more effective discussions, I can clear out our doubts immediately”.E. Students' groupsFour students gave the opinion about study groups and how they can exchange the ideas: “can discuss in larger group give more information and gain more knowledge”“Involves the whole batch makes discuss together”“Able to share information and ideas from other groups”“More interaction between batch mates and more quality discussion and brainstorming session& get to learn a few questions and topics in a single session”,“It gives chance to everyone to interact and exchange ideas. This helps everyone widen their knowledge and learn from each other”“More interesting and everybody will be taking part”.F. Benefits of being in smaller groups Students had benefitted from being in the smaller group in this PSE discussion; “Smaller groups focus more and everybody will have the chance to speak out and give their opinion”“Smaller group, better understanding and have time to prepare all triggers” “Able to learn better and effectively in small group discussions. We are also able to interact with our facilitator and the presenters”“Smaller classes and smoother and more active discussion”“Conducted in smaller groups and learn much better”.G. Strengths/ weakness/ suggestionsNine students commented on strengths and weaknesses of PSE and four students on PBL and one suggestion on the cases has been made; “PBL - detail, PSE - fast”“No waste of time for transferring to classes sharing of information more efficient”“More challenging and gives a wide scope of clinical knowledge”“Can learn something as a class, save time and energy”“Gain knowledge that cannot be found in books”One suggestion from the student to give the case scenario one day earlier to prepare the cases more nicely; “Give us the trigger one day earlier so that we can prepare for all questions and the lecturers and ask any of us”. One student impressed about usefulness in bedside learning through PSE; “PSE-more to clinical aspect and application of clinical theories to solve questions and can relate to the cases and these cases we counter every day in hospital”. One student has same idea through learning PBL, PSE; “Whatever knowledge got from anywhere is beneficial”.
4. Discussion
- The introduction of problem solving exercise in medical learning and evaluation of problem solving as a learning method was mainly positive from the idea of both the students and lecturers. This does not measure the level of support for reliability of PSE approach and its use in third year medical programmes. This study focus on specific challenges for facilitators who wish to introduce PSE in this medical program and the scenarios must effectively stimulate cues to resume the development of issues related to the topic areas. The clinical case discussion of specific topic in medicine in early clinical education is crucial for third year medical profession students. Students had the opportunity to apply in a problem-solving process that focused on selected patient case scenario. Each group of student, throughout the two-hour period, accessed and discussed among themselves for similar complaints of hypertension. The grouping of the students solved the problem of assigning a large number of students to a limited faculty facility and the facilitator. At the conclusion of each clinical session, the students responded to three questions on a previously set up questionnaire from lecturers. Careful review and critique of the answers by the academic faculty coordinator provided feedback to the students about their abilities to use the problem-solving process in solving a case study problem. Some students demonstrated excellent critical thinking and application of the problem-solving process. Other students were not as accomplished in their problem-solving abilities, but they were able to demonstrate basic problem-solving skills. Our students were asked to justify or explain their treatment decisions in their power point presentations after the discussions. The coordinator stated that the problem-oriented curriculum enabled students to understand interrelationships of content taught in different scenarios in a more effective manner than problem based learning. The outcomes from each case scenario were discussed with each participating lecturers. When the expert academician initially participated in the problem solving experiences, they often were more content-oriented than process-oriented. This orientation was reflected by several events: the comments on specific disease and presenting all the necessary information in two-hour session was difficult and the inadequate amount of time for problem solving and frequently did not proceed past problem identification. Several positive aspects of problem solving exercise experience were noted by the faculty coordinator; a small group interactional experience for students, an opportunity to practice a guided logical thought process that was designed to improve problem-solving skills, a foundation for treatment program planning and evaluation, an environment that allowed for immediate feedback to questions, the opportunity to observe the clinician's expertise, coordinators had the opportunity to develop instructional skills, the students had an opportunity to communicate with the classmates about aspects of patient's problems fully and the students began to appreciate an alternative form of several alternative treatment may exist for solving problems.In the PBL approach, students are at the centre of the learning process. Students engage in discussion of situations with all the complexity and ambiguities of real life problems, determine their learning needs, and develop appropriate approaches to solving problems. Students direct the discussion and receive feedback from their peers. Teachers serve as facilitators. They stimulate students towards self-directed learning, and ensure that all students were involved in the process. They do not transmit expert knowledge to students, but probe students’ knowledge by asking questions and encouraging specific kinds of cognitive activities. PBL requires students to spend more time and energy on conducting research, searching for information, sharing information, and commenting on information shared by their peers [11].There is a need to educate undergraduate students to be problem solvers in diverse clinical situations and environment. In one of the study on physical therapy, it provides the clear mandate and guide for teaching through problem solving [3]. It was described that developing educational experiences for problem solving and judgement is possible, so that scientific critical thinking occurs in clinical setting [3]. Even though this study was a small evaluation study and the results cannot be generalised to other medical universities or other subject modules, it does indicate the level of support for the acceptability of PSE approach and its applicability in third year medical program.
5. Conclusions
- In conclusion, a problem solving method to structure a clinical experience for the third-year medical students has been described. The results suggest that a significant knowledge gain occurred during the problem solving exercise in medicine and this gain in knowledge was closely related to the reasons behind and its strengths in practicing clinical solving skills. This study also demonstrates that the problem solving skills of students was improved by using this education model, and students’ and facilitators' reported experiences were worthwhile.
ACKNOWLEDGEMENTS
- We would like to thank third-year medical students who participated in this study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML