-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2020; 9(1): 12-22
doi:10.5923/j.diabetes.20200901.03

Current Practice in the Management of Type 2 Diabetes Mellitus in Jordan: Results of the Jordanian Diabetes Management Practices Study
Munther Momani1, Fares Haddad2, Muries Barham3, Jamal Aldarawasheh4, Chahine Fadel5, Nisrine Sabra6, Jean Tannous7
1Consultant, Endocrinologist, University of Jordan, Jordan University Hospital, Amman, Jordan
2Senior Consultant, Endocrinologist, King Hussein Medical Center, Amman, Jordan
3Consultant, Endocrinologist Al Basheer Hospital, Amman, Jordan
4Consultant, Endocrinologist, Princess Basma Teaching Hospital, Irbid, Jordan
5Medical Director Levant, Sanofi, Beirut, Lebanon
6Clinical Operations Manager, Sanofi, Beirut, Lebanon
7Medical Manager, Sanofi, Beirut, Lebanon
Correspondence to: Munther Momani, Consultant, Endocrinologist, University of Jordan, Jordan University Hospital, Amman, Jordan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background and Aims: The aims of this study were to determine the proportion of T2DM patients achieving optimal glycemic control of glycated hemoglobin A1c (HbA1c) below 7%, to describe the profile of patients with T2DM in Jordan, and to describe the management and care of patients with T2DM in public institutions in Jordan. Patients and methods: This is a multicenter, cross-sectional study included 432 diabetic patients from 22 sites across Jordan. Data related to the socio-economic profile, medical history, diabetes-related complications, physical examination, glycemic control, episodes of hypoglycemia as well as concomitant anti-diabetic therapy were collected. Results: The proportion of T2DM patients achieving glycemic targets (HbA1c<7%) was 29.2% and 18.1% achieving the HbA1c <6.5%. The proportion of T2DM achieving the triple target HbA1c<7%, normal blood pressure (SBP/DBP: 140/90 mmHg) and LDL-C<100 mg/dL was 8.1%. 41.9% of the subjects had micro or macro vascular complications, including Retinopathy (19.4%), Sensory Neuropathy (17.6%), Microalbuminuria (4.9%) and Angina (5.8%). Furthermore, 5.6% patients were hospitalized one time due to DM during the past 12 months. 16.4% of patients experienced symptomatic hypoglycemia in the past 3 months, 6.8% of which had severe hypoglycemia. Conclusion: This study shows that the glycemic control in the majority of a cohort of patients with diabetes managed in the public healthcare sector in Jordan was suboptimal, which is consistent with previous findings from local, regional and international cohorts. The results demonstrate the urgent need to design and launch projects to improve metabolic control among patients with type 2 diabetes in Jordan.
Keywords: Type 2 diabetes in Jordan, Management practices, Real-life study
Cite this paper: Munther Momani, Fares Haddad, Muries Barham, Jamal Aldarawasheh, Chahine Fadel, Nisrine Sabra, Jean Tannous, Current Practice in the Management of Type 2 Diabetes Mellitus in Jordan: Results of the Jordanian Diabetes Management Practices Study, International Journal of Diabetes Research, Vol. 9 No. 1, 2020, pp. 12-22. doi: 10.5923/j.diabetes.20200901.03.
Article Outline
1. Introduction
- Type 2 Diabetes Mellitus (T2DM) is a major worldwide concern and a complex chronic condition requiring multiple care processes, professional expertise and patient education in order to optimize control of risk factors to prevent complications. It was estimated that the prevalence of DM was 415 million in 2015, compared with 108 million in 1980 [1]. The most prevalent form of DM is type 2 (T2DM), which showed highly increasing in the last decade. According to the International Diabetes Federation (IDF), more than 90% of people with diabetes have T2DM [2,3]. The number of patients with T2DM is expected to reach 629 million by 2045. The major concern that there are some patients with undiagnosed T2DM, already have complications such as retinopathy, chronic kidney disease, neuropathy, and cardiovascular diseases [2,4,5]. In 2015, the total deaths due to DM and its complications exceeded 5 million, with more than 80% of diabetes-associated deaths occurring in low- and middle-income countries [1]. Therefore the regular follow-up and rapid management of diabetes are very important to save lives and prevent these complications. Throughout the former few years, there have been significant advances in medications, insulin delivery, and glucose monitoring technologies. Unfortunately, the majority of the people with diabetes and their health-care professionals have limited or no access to many of these tools due to inadequate financial and/or health-care resources [6,7]. Also, in the high-income countries, many communities and practice areas are populated with low-income, underinsured individuals. Additionally, the appropriate use of resources is highly dependent on the education of the health-care team members and people with diabetes [8]. Managing T2D is complex, time-intensive and ongoing. As such, primary care physicians (PCPs) are challenged to meet the changing medical needs of those with the disease. The challenge becomes even more daunting when there is limited access to the most current tools and treatments as well as supporting personnel, notably diabetes educators [9,10].The primary goal of the treatment of diabetic patients is to achieve good (near standard) metabolic control, thus preventing the onset of long-term complications [11,12]. International diabetes societies (ADA, EASD) have made global recommendations aiming to achieve optimal levels of glycemic control HbA1c < 7% [13]. Also, substantial efforts are devoted to improve diabetes management with evidence-based guidelines. Despite all recommendations related to glycemic control, a large number of patients do not reach the target HbA1c value below 7% [13]. This is associated with multifactorial challenges including the resources allocated to diabetes education, patients’ adherence to lifestyle therapy in addition to the patients and physicians common barriers to timely introduction and effective use of insulin. According to the International Diabetes Management Practices Study (IDMPS Wave 5) results, extent of glycemic control across the Middle East region among patients with T2DM ranged from 31.1% in KSA to 41.9% in UAE [14]. A large number of epidemiological studies have been conducted at the regional level and included Jordan, to assess the quality of care in DM patients, and/or compliance with treatment guidelines and programs [15]. However, there is a lack of data on the quality of care of DM patients treated in the Public Institutions in the country. Public institutions are accountable for the treatment of the majority of diabetic patients, yet for logistical limitations these institutions were underrepresented in previous registries on this topic [15]. Therefore, there is need to better assess the current medical practices in diabetes management in Jordanian public institutions in order to develop an action plan that can improve the quality of care of diabetic patients in the country.The Jordanian Diabetes Management Practices Study (JDMPS) is a disease registry that focuses on T2DM patients seen by general practitioners, family medicine, internists, diabetologists/endocrinologists who are experienced in diabetes management and insulin therapy (initiation and titration) and working in the public institutions in Jordan. It will help assess diabetes treatment practices in a real-world setting to evaluate compliance with international guidelines. This will provide supportive data for national recommendations for the management of diabetes and will help in putting in place strategies that will lessen the disease burden, prevent the onset of long term complications and reduce healthcare resources spent.
2. Materials and Methods
- We followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology Statement) guidelines during the preparation of this prospective cohort study [16]. The study was conducted in full accordance with the guidelines for Good Clinical Practice and the Declaration of Helsinki, and data for each patient were collected only after obtaining signed written data release forms.
2.1. Study Design, Setting, and Follow-up
- This was a national, multicenter, observational, cross-sectional study performed between November 2017 and April 2018. The study was conducted in 22 diabetic centers across Jordan to assess current practices in the management of patients with T2DM.
2.2. Eligibility Criteria of the Study Participants
- We enrolled both male and female adult patients (> 18 years old) diagnosed with T2DM, visiting the physician during the recruitment period of the study. We excluded patients with type 1 diabetes mellitus, current temporary insulin therapy (gestational diabetes, surgery, pancreas cancer, pancreas disorders, and acute illnesses), current pregnant or lactating women, and patients who enrolled in clinical trials at study entry. To reduce selection bias, physicians from each site were asked to enroll 15–25 eligible patients consecutively. All patients signed an informed consent form prior to enrollment. Both the study protocol and informed consent were approved by the local ethical committee.
2.3. Variables and Data Collection Methods
- For each eligible patient, the following data were collected: the socio-economic profile, diabetes medical history including; diabetes-related complications, physical examination, glycemic control (fasting and post-prandial blood glucose, HbA1c), self-monitoring blood glucose, episodes of hypoglycemia as well as concomitant anti-diabetic therapy, and patient education.
2.4. Study Outcomes
- The primary outcome was to determine the proportion of T2DM patients achieving glycemic targets HbA1c below 7%. The secondary outcomes were; (1) description the management of care of patients with T2DM including: the proportion of T2DM achieving the HbA1c<6.5%, the target glycemic control (HbA1c) in elderly population (more than 65 years old), the proportion of T2DM achieving the triple target HbA1c<7%, normal blood pressure (SBP/DBP: 140/90 mmHg) and LDL-C<100 mg/dL, (2) the level and type of diabetes education, (3) description of oral and injectable therapies patients with T2DM were exposed to before study entry, (4) the frequency and the severity of episodes of hypoglycemia patients with T2DM during the past 3 months.
2.5. Compliance with Ethics Guidelines
- All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Declaration of Helsinki in 1964, as revised in 2013. Informed consent was obtained from all patients for being included in the study.
2.6. Statistical Methods
- This is an observational study powered for the primary endpoint of the proportion of T2DM patients achieving glycemic targets HbA1c below 7%. The sample size was determined based on the primary objective and on the precision that is expected.With 400 T2DM patients we will be able to estimate the proportion of T2DM patients achieving glycemic targets HbA1c below 7% to within a margin of error of at most ±4.9% using 95% confidence interval.All variables recorded during the study were summarized. Absolute and relative frequencies were provided for categorical variables. Mean and standard deviation were provided for continuous variables. For quantitative variables, t-test was used to in case of normal distribution, while a Wilcoxon signed-rank test otherwise. Chi square test was used for categorical variables. A p-value of less than 5% was considered statistically significant. Univariate and multivariate logistic regression analyses were applied to identify the predictive factors for poor control of HbA1c (>7%). Univariate logistic regression considered each factor individually and multivariate considered all factors simultaneously. Multivariate Model selection was carried out using stepwise and forward method by removing variables from the model that were not significant. The Hosmer–Lemershow test was used to measure the goodness-of-fit of the logistic regression model with p-value ≤ 0.05 indicating boor fitness of model. Odds ratios (OR) with 95% confidence intervals (95% CI) were provided. All statistical tests were performed using SPSS program version 25.
3. Results
3.1. Patients Characteristics
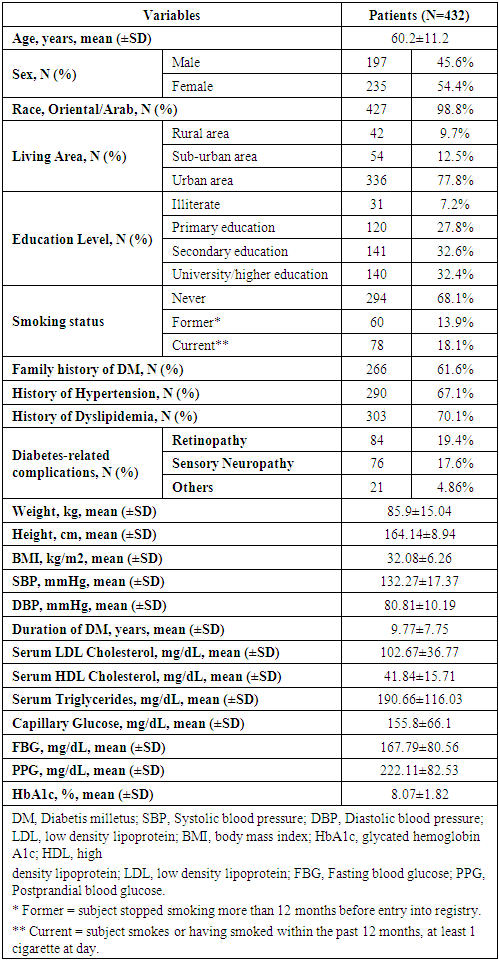
- In this cross-sectional study, we enrolled 432 diabetic patients. All of the 432 patients were eligible with no protocol deviations. The demographic and clinical characteristics of the 432 eligible subjects are shown in Table 1.
|
3.2. Glycemic and Lipid Results
- The mean capillary glucose level was 155.8±66.1 mg/dL, while the mean fasting blood glucose was 167.79 (±80.5) mg/dL, and the mean postprandial blood glucose was 222.11 (±82.53) mg/dL. Regarding the HbA1c test, about 419 (97%) had HbA1c test before. The test was performed in 421 patients with mean HbA1c of 8.07% (±1.82). Out of the 421 patients, the mean HbA1c for patients using an oral agent only as monotherapy was 6.627% (±1.1), which was significantly lower than the HbA1c for those using dual therapy 8.04% (±1.9, p<0.01) or more than two oral drugs 8.21% (±1.3, p<0.01). The highest mean HbA1c was observed in patients who were treated with dual oral therapy plus insulin 9.015% (±1.3), followed by those using monotherapy plus insulin 8.77% (±1.9), and those using insulin only 8.54% (±1.4) (Figure 1).
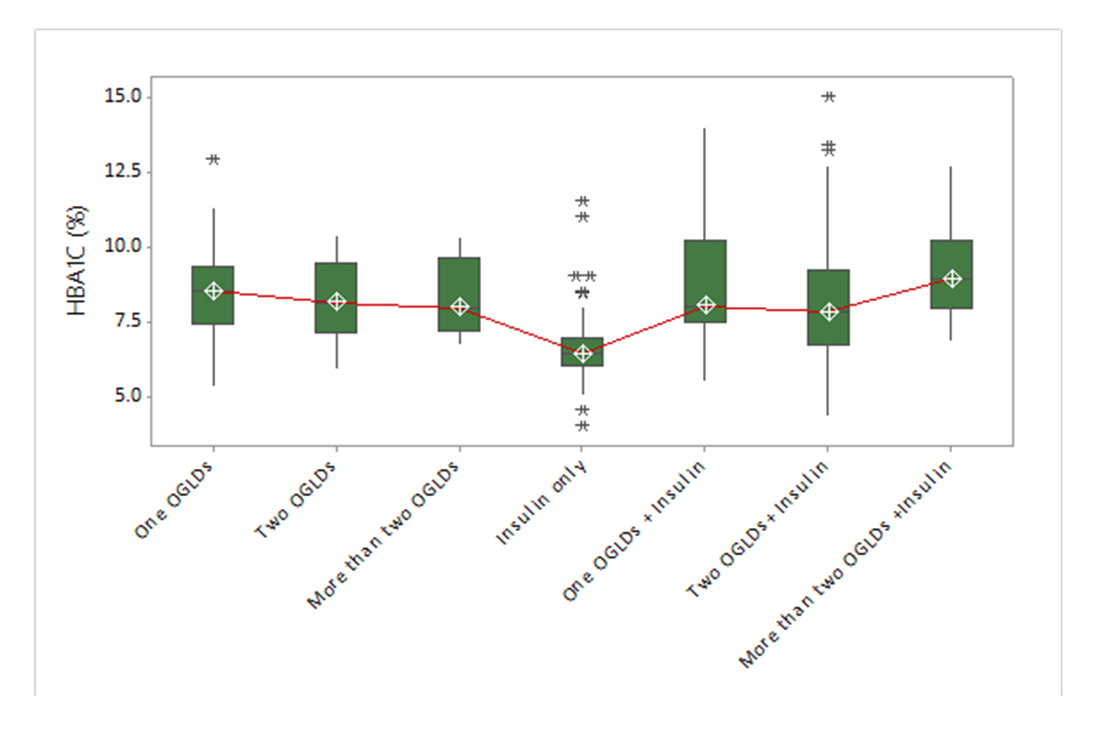 | Figure 1. Mean and standard deviation of the patients classified by the administered medications |
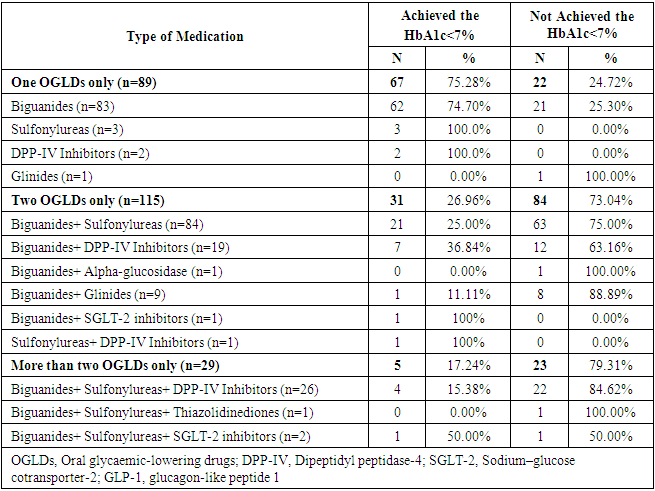
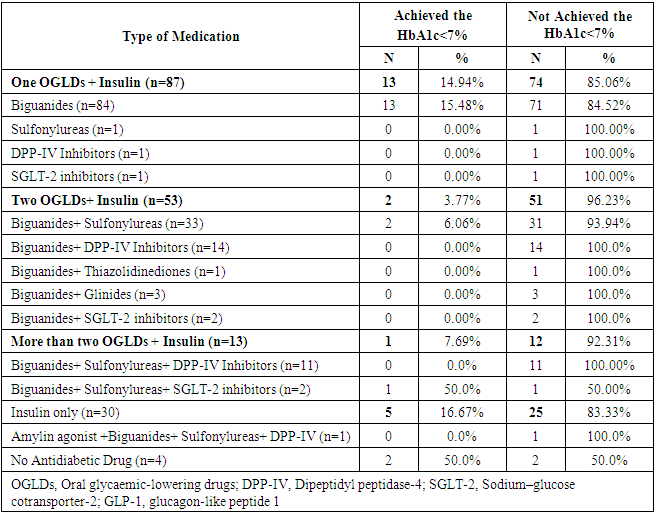
3.3. Antidiabetic Drugs
- Up to the study visit, 95 patients (22%) were treated with monotherapy, 117 (27.1%) were treated dual therapy, and only 29 (6.7%) were treated with more than two OGLDs. The most common monotherapy administered were biguanides, while the biguanides plus sulfonylureas were the most common dual therapy (Figure 2). Furthermore, 31 patients (7.2%) received insulin only, 88 patients (20.4%) received insulin plus one OGLDs, 53 (12.3%) were treated with insulin plus two OGLDs, and only 13 (3%) were treated with insulin plus more than two OGLDs (Figure 3).
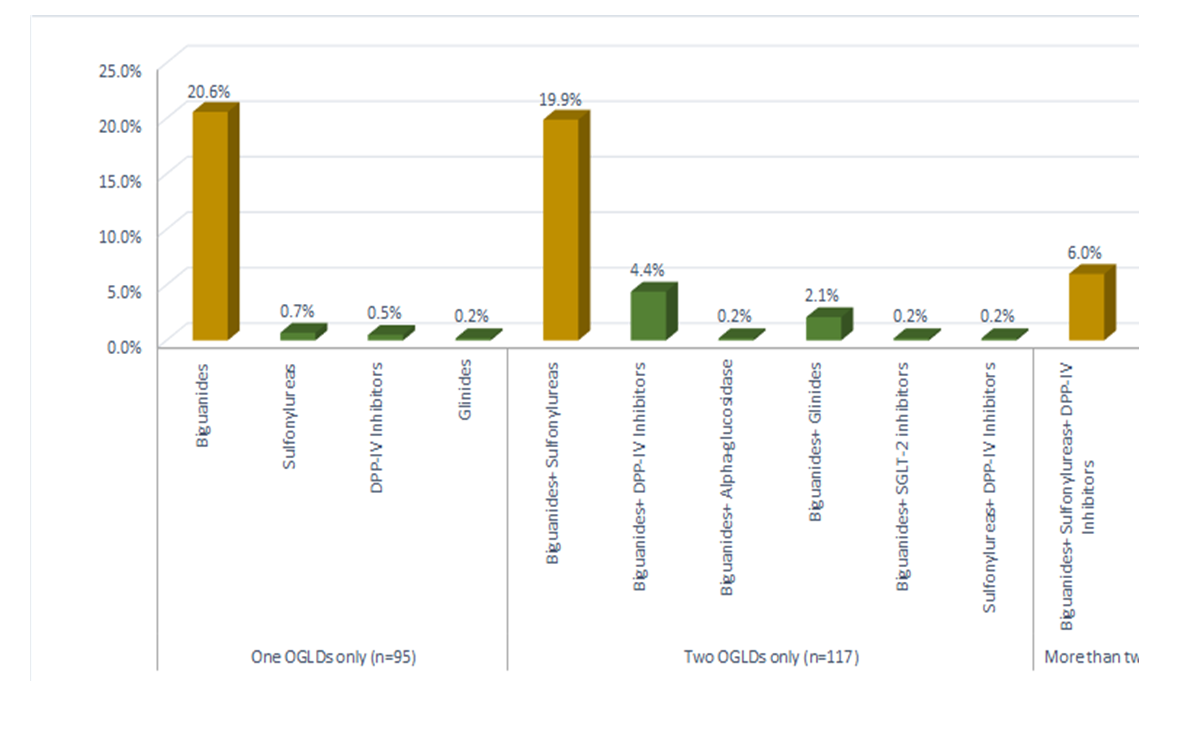 | Figure 2. Discretion of the oral antidiabetic regimens (without insulin) administered by the patients with Type 2 Diabetes were exposed to before study entry |
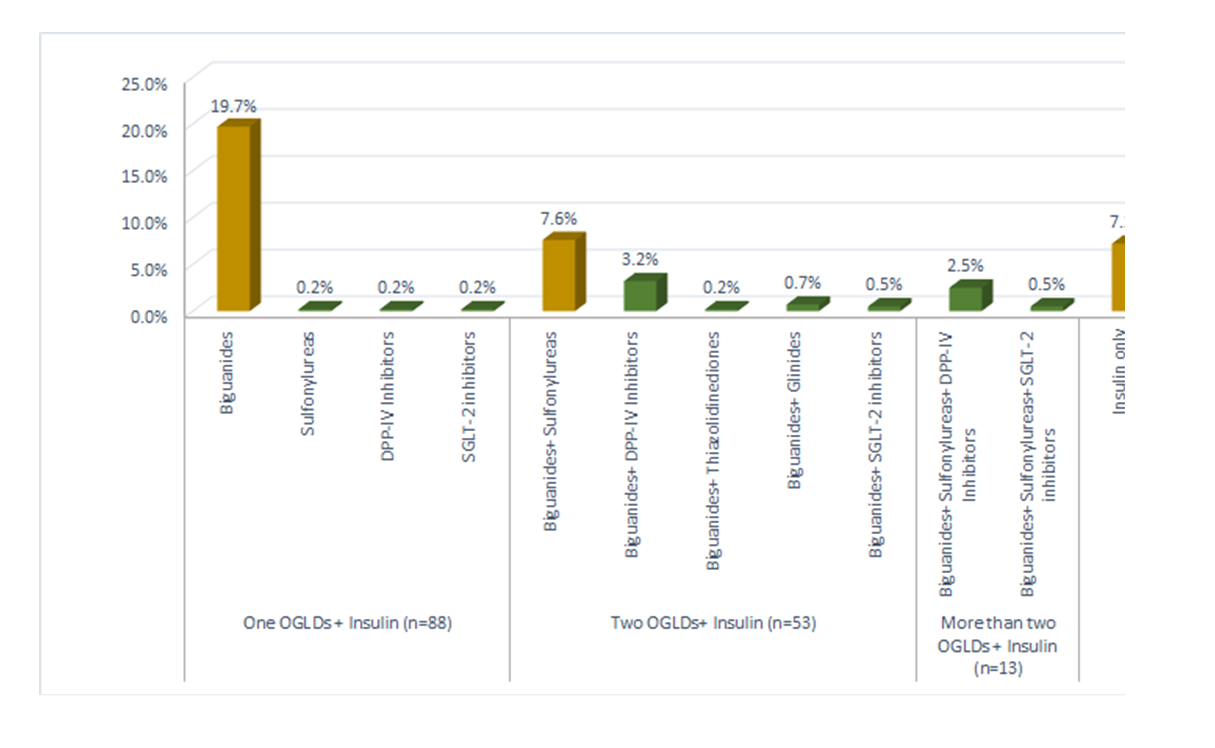 | Figure 3. Discretion of the oral antidiabetic regimens plus insulin administered by the patients with Type 2 Diabetes were exposed to before study entry |
3.4. Proportion of Patients Achieving the Glycemic Targets
- Out of 421 patients, the proportion of T2DM patients who achieved the glycemic targets of HbA1c<7% was 126 (29.9%), while the proportion of patients who achieved the targets of HbA1c below 6.5% was 78 (18.5%). The triple target of HbA1c<7%, normal blood pressure (SBP/DBP: 140/90 mmHg), and LDL-C<100 mg/dL was achieved by 35 (8.3%) patients. Table 2 shows the achievement of HbA1c of <7% according to the oral medication administered without insulin. A higher number of patients on monotherapy achieved the HbA1c<7%, 67 (75.28%). Inversely, for T2DM patients who were treated by two OGLDs or more, the number of patients who didn’t achieve the same glycemic target were higher than the patients who achieved the glycemic target. For patients who were treated with insulin only, 5 patients (16.67%) achieved the HbA1c<7% and 25 (83.33%) patients did not as seen in Table 3. Adding insulin to OGLDs was not associated with high glycemic control in T2DM patients. The overall correlation between the level of control (achieved the HbA1c<7% or not) with the administered medications showed a statistically significant difference between the type of medication and achieving the glycemic control (p<0.001).
|
|
3.5. Patients’ Behavior towards Insulin Initiation and Needle Injections
- Out of 187 patients receiving insulin treatment, about 78 patients (41.7%) used a reusable pen, 87 (46.5%) used a disposable pen, and 34 (18.2%) used vials. 13 patients (7%) discontinued insulin therapy, most of them were due to fear of hypoglycemia. On the other hand, out of the patients receiving insulin, 134 patients (71.7%) had a benefit from the support on how to use insulin. This support was in form of call center in 38 patients (28.4%), counseling by a diabetic nurse in 89 patients (66.4%), home visit by community nurse in 26 patients (19.4%), and others.
3.6. Patients Education and Follow up
- A total of 352 patients received diabetes education. Of them, 300 patients (69.4%) reported that they received diabetes education program by the clinical staff. The most commonly used facility for education was the hospital-based diabetes center for 134 patients (44.7%), followed by the community-based diabetes center in 38 (12.7%). Furthermore, this education was commonly delivered through a physician in 211 (59.9%), or nurse in 193 (54.8%). The educational programs were either structured courses 13 (3.7%), random education (not structured) 111 (31.5%), individual education 248 (70.5%), or in group education 6 (1.74%). In addition, the content of educational programs was varying, which might be increasing the knowledge on how to use medication for 332 patients (94.3%), increasing the knowledge about the nature of diabetes for 273 patients (77.6%), increasing the skills of self-management (SMBG, titration of insulin) for 194 patients (55.1%), changing the attitude and behavior for 205 patients (58.2%), or increasing the knowledge on diet and exercise for 270 patients (76.7%).
3.7. Results of Hypoglycemia
- The symptomatic episodes of hypoglycemia were reported in 71 patients (16.44%) with T2DM in the past 3 months. Most of those patients were receiving biguanides plus insulin 22 (31%), insulin only 9 (12.7%), biguanides/sulfonylureas plus Insulin 7 (9.9%), biguanides only 5 (7%) and the rest of patients were on either one or two OGLDs. Out of the patients with hypoglycemia in the past 3 months, the frequency of severe episodes was reported in 29 (6.8%) patients. Of them, eight patients were on biguanides plus insulin and three patients were on insulin only.
4. Discussion
- In this cross-sectional, observational study, 432 diabetic patients were enrolled. Among them, 421 patients are included in the primary and secondary analysis including HbA1c level because we have 11 patients with missed data for HbA1c value. The mean age of the patients was 60.21±11.2 years, mean of weight 85.96±15.04 Kg, mean of height 164.14±8.94 cm, mean of body mass index was 32.08±6.26, mean waist circumference 103.87±14.8 cm. Only 89 (20.6%) of the patients were diagnosed before the age of 40 years and the average duration of DM was 9.77±7.75 years. About 266 (61.6%) of the included patients had family history of DM, and 290 (67.1%) of the included patients were suffering from hypertension and almost all of them received antihypertensive treatment. Our analysis showed that 303 (70.1%) diagnosed with dyslipidemia, 291 (67.3%) of them received dyslipidemia treatment. This study demonstrated that the proportion of T2DM patients achieving glycemic targets (HbA1c) below 7% was 126 (29.2%) and 78 (18.1%) achieved the HbA1c <6.5, while the proportion of T2DM patients not achieved glycemic targets (HbA1c) below 7% was 295 (68.3%). The level of control in the public sector is very similar to the 31.5% obtained in the International Diabetes Management Practices Study Wave 7, conducted in 24 private centers in Jordan back in 2016 [33].Out of the patients who achieved HbA1c below 7%, 103 patients (23.90%) received oral medications, 16 (3.70%) received oral medications plus insulin, and 5 (1.2%) received only insulin. The overall correlation between the level of control (Achieved the HbA1c<7% or not) with the administered medications showed a statistically significant difference between the type of medication and achieving the glycemic control, p <0.0001.In accordance with our findings, Pinchevsky et al. [17] conducted a cross-sectional study to determine the proportion of patients who achieved the triple target (HbA1c, blood pressure (BP), and cholesterol) in South Africa and reported that the number of patients who achieved the HbA1c <7 was 69 (19.3%). Moreover, the HbA1c for patients using an oral agent as monotherapy was 8.7% (±2.6), which was lower than the HbA1c for those using monotherapy insulin 9.3% (±2.1). The patients using combinations of orals/insulin had an HbA1c of 9.5% (±2.6). In direct agreement with our results, the combination of insulin and oral medications does not work to reduce the ratio of HbA1c, on the contrary, it may increase this ratio. This finding was supported by the results of Liu and his colleagues [18] who reported that among 5961 diabetic Chinese patients, the percentages of patients with optimal diabetes control (HbA1c<6.5% or <7%) were 21.4% and 35.2%, respectively. Another 35.6% had HbA1c between 7% and 9%, and 28.2% had HbA1c >9%. Only 24.9% of insulin users (n= 3669) achieved HbA1c<7% and 33.8% of the oral medication users (n= 4340) achieved HbA1c<7%. They concluded that the patients treated with insulin were less likely [OR, 0.508; 95% CI (0.350–0.738), p=0.001] to achieve the three targets compared with those who are not on insulin. Insulin treatment is generally started after oral agents have failed, but simply using insulin does not necessarily imply an improvement in glycemic control. It has been reported that 61.53% of Chinese patients with type 2 diabetes are treated with insulin [19]. The number of patients using insulin in China is large, but only 37% of them attain ideal glycemic control. One possible reason is the poor skill in determining the dose. Poor injection technique could also be an important reason for poor blood glucose control [20]. Because T2DM is a chronic disease with progressive deterioration in beta cell function, duration of diabetes may be playing a role in the poor control of glycaemia among insulin-treated patients [21]. According to 2019 American Diabetes Association (ADA) recommendations, the early introduction of insulin should be considered if there is evidence of ongoing catabolism (weight loss), if symptoms of hyperglycemia are present, or when A1C levels (>10% [86 mmol/L]) or blood glucose levels (≥300 mg/dL [16.7 mmol/L]) are very high [22].Our results demonstrated that the proportion of T2DM achieving the triple target HbA1c<7%, normal blood pressure (SBP/DBP: 140/90 mmHg) and LDL-C<100 mg/dL as per recommendations of international guidelines was 8.1% and the proportion of patients who did not achieve was 89.4%. This finding is similar to those of Lui et al., [18] who reported that the among 2736 subjects for whom data for all three parameters were available, the percentage of patients meeting all recommended ABC targets was 5.4%. They reported that smoking, higher BMI and insulin use were each associated with failure to achieve one or more of the treatment goals. Regarding the diet and life style modification of T2DM patients, we reported 193 patients (44.7%) on a controlled diet and 232 patients (53.7%) were not. Life-style changes such as balanced diet and physical exercise are important factors in achieving good controlling on T2DM and avoiding its long-term complications [23]. Adherence has been defined as the extent to which a person’s behavior–taking medication, following a diet and or executing lifestyle changes corresponds with agreed recommendations from a health care provider. These rates are consistent with the findings of similar studies in neighboring countries, where the rate of adherence to diet varied between 10.7 and 36.5% [24–26]. In Yemen, only 21.0% of patients adhered to the recommended diet and 15.0% adhered to regular exercise [27]. Several socio-demographic and clinical factors were associated with patients’ adherence. The low adherence rate amongst the study patients was reflected on their level of glycemic control (HbA1c). According to the ADA 2019 recommendations, all adults, and particularly those with T2DM, should decrease the amount of time spent in daily sedentary behavior. Prolonged sitting should be interrupted every 30 min for blood glucose benefits, particularly in adults with T2DM [22].In this study, a total of 300 patients (69.4%) received diabetes education by clinical staff and 126 patients (29.2%) did not. In a similar study conducted in 24 private institutions and clinics in 2016 (International Diabetes Management Practices Study Wave 7), among 350 patients, 60.4% of T2DM patients received diabetes education and 50% were involved in an educational program provided by the physician or his/her clinical staff [33]. The types of diabetes educational facility were Hospital-based diabetes center in 134 patients (31.0%), Community-based diabetes center in 38 (8.8%). The education was delivered through a physician in 211 (48.8%), a nurse in 193 (44.7%), a dietician / nutritionist 59 (13.7%), a certified diabetes educator 58 (13.4%), and a person with diabetes 14 (3.2%). Although education alone is not a cure for the disease, the type 2 diabetes patient is not able to achieve metabolic regulation, if does not know the basic principles of nutrition, physical activity, care of the lower extremities, as well as specific skills related to the administration of subcutaneous injection of insulin, control of blood sugar levels, and other necessary parameters [28,29]. The teaching of the technique of injection of insulin by the patient and a family member is the most important part of the educational program. Initially, the technique of injection is taught and then the calculation of the required units of insulin, the selection of sites, and the way of handling the equipment in order to prevent contamination and injuries. Afterwards, basic principles regarding diet, maintenance of body weight, resting, and prevention of hypoglycemia or deregulation of blood sugar are taught [22,29–31].Regarding the anti-diabetic therapies patients were exposed to before study entry, our results show that over half of patients with T2DM in public institutions in Jordan, at least in our population and during the time-period considered, are treated with OGLDs, whereas insulin is chronologically and progressively delayed until it becomes the only medication effective to treat these patients. Concomitantly, within the group treated with OGLDs the percentage of people with HbA1c below 7.0% decreased in patients with long standing diabetes. This trend follows the chronological progressive algorithm proposed by most treatment guidelines in order to attain HbA1c levels able to prevent development and progression of chronic complications. However, data from our study population show that the use of insulin to control hyperglycemia is far from attaining this aim: the percentage of people with HbA1c < 7.0% markedly decreased instead of improving when insulin was added to T2DM treatment. In addition, a high proportion of patients (41.9%) were exposed to micro and macro vascular complications including Retinopathy and Sensory Neuropathy. It is worth mentioning that the rate of complications was considerably lower (30.6%) in the private institutions [33]. Patients’ socio-demographic characteristics and behavior may act as barriers to the insulin timely initiation. The delay in insulin initiation in T2DM patients can be correlated to the prolonged use of OGLDs to high proportion of patients in the first few years of diabetes. This agrees with reports from developing countries on delay in insulin initiation/intensification (clinical inertia) and not translating the clinical assessments into actions to improve glycemic control. This might have led to the high rates of micro and macro vascular complications observed in the study patients. The high proportion of patients with more than one microvascular complication may be due to the low proportion of them achieving glycemic control. The cardiovascular risk factors observed in majority of patients in the study can also be correlated to long standing diabetes.Another notable finding of our study was that over half of T2DM patients receiving insulin (52.4%) were using premixed insulin (with around 39% on premixed human insulin) and correspondingly fewer being treated with a basal/prandial strategy.This pattern of insulin use contrasts with the available international guidelines. Early initiation of insulin therapy should be considered in patients not achieving the target HbA1c of <7%. The American Diabetes Association recommends that for patients with T2DM who are not achieving glycemic goals, drug intensification should not be delayed. Insulin should be considered as part of any combination regimen when hyperglycemia is severe, especially if catabolic features (weight loss, hypertriglyceridemia, and ketosis) are present. Basal insulin alone is the most convenient initial insulin regimen. Intensification of insulin treatment can be done by adding doses of prandial to basal insulin. Starting with a single prandial dose with the largest meal of the day is simple and effective, and it can be advanced to a regimen with multiple prandial doses if necessary [22]. In addition, the American Association of Clinical Endocrinologists Diabetes Management Algorithm confirms that patients taking two oral antihyperglycemic agents who have an A1c >8.0% and/or long-standing T2DM are less likely to reach their target A1c with a third oral antihyperglycemic agent, insulin should be added to the regimen and the dosage should be adjusted at regular and initially fairly short intervals, measured in days, to achieve the targeted glycemic goal. A full basal-bolus program is the most effective insulin regimen and provides greater flexibility for patients with variable mealtimes and meal carbohydrate content. Premixed insulins provide less dosing flexibility and have been associated with a higher frequency of hypoglycemic events compared to basal and basal-bolus regimens [32].Furthermore, it is notable that in our T2DM cohort, basal insulin dosing was relatively low, especially in patients with a high body mass index (BMI), which may also contribute to poor glycemic control.Clearly, the earlier initiation of insulin treatment in T2DM patients in Jordan may be one way of improving diabetic control, in addition to more widespread use of a basal/prandial strategy when appropriate, noting that this approach would require additional patients’ education. However, there are a number of possible explanations for our findings which may act as barriers to the implementation of this approach. In our study, 74% of diabetes education was delivered to patients in less than 1 hour, around 30% of patients reported no diabetes educational program by clinical staff, and 27.3% reported no benefit from support on how to use of insulin. In addition, about half of the included patients required co-payment for medication. As such, additional drug costs may act as a barrier to their use for many patients. The relative infrequency of SBGM by these patients may also be a reflection of cost. In line with infrequent SBMG, concerns regarding dose titration may also apply. These may explain why, while the managing physicians are experienced in insulin therapy, its timely use in T2DM patients, and use of appropriate regimens may not necessarily be employed.In view of these findings, it is essential to gain a better understanding of the failings and barriers to improved diabetes care in Jordan. This situation must be carefully considered by health and academic authorities in order to implement effective strategies – such as implementation of diabetes education at every level - to effectively modify this situation. We postulate that the implementation of improved strategies would decrease the heavy socioeconomic burden derived from poorly controlled people with T2DM.Our strength points were that we comprehensively assess the current practice and management of T2DM in Jordan including the socio-economic profile, diabetes medical history including; diabetes-related complications, physical examination, glycemic control (fasting and post-prandial blood glucose, HbA1c), self-monitoring blood glucose, episodes of hypoglycemia as well as concomitant anti-diabetic therapy, and patient education. In addition, our study conducted in 22 diabetic centers across Jordan would allow the generality of the results. On the other hand, this study has some limitations. Due to the nature of the study as a cross-sectional study, some of the data were missed from the patients’ records. Our sample size was relatively small, but we considered the diverse population and the geographical distribution of the included patients.
5. Conclusions
- In conclusion, this study demonstrates that in accordance with current global findings, the glycemic control of the majority of a cohort of patients with diabetes managed in the public healthcare sector in Jordan was suboptimal when assessed according to HbA1c levels. Our findings highlight the significant gap that remains between international recommendations and the current standard of care for diabetic patients in Jordan. Improved compliance with international recommendations is necessary to deliver a better quality of diabetic care. This will require improvements in adherence to lifestyle therapy with balanced diet and physical exercise, in the education of patients on disease management and the earlier use of insulin and basal–prandial protocols, allied with improvements in SBMG in patients with T2DM. The results demonstrate the urgent need to design and launch projects to improve metabolic control among patients with T2DM in Jordan.
ACKNOWLEDGEMENTS
- This study was sponsored by Sanofi. The authors thank the study participants, trial staff, and investigators for their participation. Editorial support was provided by Dr. Hussien Ahmed MD, of RAY-CRO and was funded by Sanofi. All the patients were acknowledged of their participation in the study.
Disclosure
- M. M. is a speaker for Hikma, Dar Al Dawa, Merck & Co., Sanofi, Pfizer, Astra Zeneca, Novartis, Novo Nordisk, Boehringer Ingelheim, Eli Lilly and Takeda. C. F., N. S. and J. T. are employees of Sanofi.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML