-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2020; 9(1): 1-4
doi:10.5923/j.diabetes.20200901.01

Diagnosis of Diabetes Mellitus in a Resource-Constrained Setting: A Comparison of Fasting Plasma and Two Hours Post Prandial Glucose Values
Allison Frederick Igila, Ojule Aaron C.
Department of Chemical Pathology, Faculty of Basic Health Sciences, University of Port-Harcourt, Rivers State, Nigeria
Correspondence to: Allison Frederick Igila, Department of Chemical Pathology, Faculty of Basic Health Sciences, University of Port-Harcourt, Rivers State, Nigeria.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

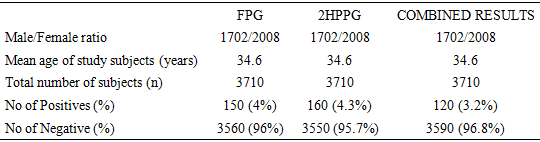
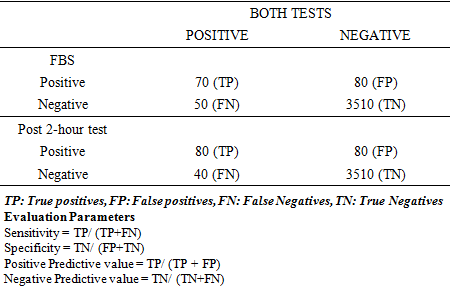
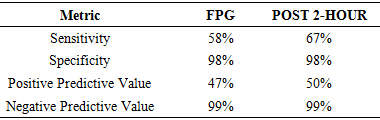
Background: Studies has shown that the prevalence and incidence of diabetes mellitus varies with type of diagnostic criteria used: fasting plasma glucose of ≥ 7 mmol/l or a two hours post prandial glucose of ≥ 11.1 mmol/l or a glycated haemoglobin of 6.5%. This mean that the sensitivity and specificity of these parameters may vary. Though the diagnostic criteria of FPG and 2HPPG is used independent of the other, the cost of these tests become important and significant with regards to choice in resource- constrained setting. Aim: This study is to compare the ability of FPG and 2HPPG diagnostic criteria in making a diagnosis of diabetes from oral glucose tolerance test (OGTT) results in this resource constrained locality. Methods: A retrospective study of OGTT results from the laboratory of a tertiary hospital in southern Nigeria. WHO criteria for diagnosing diabetes mellitus using FPG≥ 7mmol/l and/or a 2HPPG ≥ 11.1 mmol/l from each subject was compared for sensitivity, specificity and accuracy. This OGTT results were determined using the glucose oxidase method to evaluate plasma glucose. Results: 150 subjects were diagnosed diabetic when the FPG was used, while 160 subjects were diagnosed diabetic when 2HPPG parameter was used. Those that were simultaneously positive for both FPG and 2HPPG were 120 and were regarded as the true positives (TP) for the purpose of this study. The sensitivity of both FPG and 2HPPG were 58% and 67% respectively while the specificities were both 98%. Conclusion: From this study, it was noted that more subjects were diagnosed diabetic using the 2HPPG which also had a higher sensitivity and positive predictive value. Therefore, the use of 2HPPG should be encouraged for targeted screening of diabetes mellitus to reduce a false sense of security for those who may be misdiagnosed and FPG test used for mass screening of diabetes mellitus to save time.
Keywords: Post prandial glucose, Fasting plasma glucose, Glucose oxidase
Cite this paper: Allison Frederick Igila, Ojule Aaron C., Diagnosis of Diabetes Mellitus in a Resource-Constrained Setting: A Comparison of Fasting Plasma and Two Hours Post Prandial Glucose Values, International Journal of Diabetes Research, Vol. 9 No. 1, 2020, pp. 1-4. doi: 10.5923/j.diabetes.20200901.01.
1. Introduction
- The management of diabetes mellitus and its complications is fast becoming a major health challenge globally [1]. Some complications eventually end in amputation of limbs, which, to a reasonable extent, affects the patient’s way of life, his economy and the economy of the country in general, as work hours are lost through hospital admissions and visits [2]. This condition is worsening as the world wide incidence and prevalence of diabetes mellitus is increasing [3]. Fasting plasma glucose, two hours post prandial (2HPP) glucose and glycated haemoglobin (HbA1c) can all be used for making diagnosis and managing diabetes. This has been made possible with the use of universally accepted cut-offs for making diagnosis of diabetes for each of these diagnostic parameters (FPG, 2HPPG and HbA1c). The diagnostic criteria for glucose value using the FPG is a plasma glucose value equal to or greater than 7.0mmol/l with symptoms of diabetes or subjects having this value on two different occasions. For 2HPPG, a diagnosis of diabetes mellitus can be made with a plasma value greater than 11.1mmol/l, while a glycated haemoglobin (HbA1c) value greater than 6.5% is seen as being diabetic [4]. Of the three criteria, fasting plasma glucose is widely used in this part of the world and can easily be carried out in every health centre, both in rural and urban areas. Unlike the fasting plasma glucose, glycated haemoglobin is not widely available especially in the rural areas, because it is more expensive and requires more specialized and expensive equipment.Apart from the non-availability of glycated haemoglobin in most rural areas, it is more expensive than the fasting plasma glucose and this may have guided health practitioners’ preference of FPG or 2HPPG test over glycated haemoglobin as the first line screening test. Values of fasting plasma glucose and 2- hours post prandial glucose have been shown to be affected by subjects’ preparation and time of sample collection, [5] apart from the effect race, age and sex have on plasma glucose values. Studies have also shown that the prevalence of diabetes mellitus will vary with the diagnostic parameter used. This therefore means that the outcome of a screening test based on the diagnostic cut offs for FPG and 2HPPG may vary, even in the same subjects. This has therefore made it necessary to compare the diabetes diagnostic cut-offs of fasting plasma glucose and 2-hour post prandial glucose values of subjects in this resource-constrained region, in order to further evaluate the preferential use of these diagnostic criteria in our study area.
2. Methods
- This is a retrospective study of oral glucose tolerance test (OGTT) results from the worksheet of the Chemical Pathology laboratory of the University of Port Harcourt Teaching Hospital in southern Nigeria for a period of six months. The glucose oxidase kit by Randox laboratory [6] was used to estimate both FPG and 2HPPG values by the laboratory. The WHO diabetes diagnostic criteria of ≥ 7mmol/L for fasting plasma glucose and ≥ 11.1mmol/l for 2-hour post prandial glucose were compared for each individual OGTT result. The percentage of subjects that were diagnosed diabetic using the fasting plasma glucose alone was noted and those that were diagnosed diabetics using only the 2-hour post prandial glucose cut off was also noted. For the purpose of this study, the number of subjects that were positive simultaneously for both FPG and 2HPPG were taken as true positives (TP) even though each diagnostic criterion is independent of the other. These ‘true positives’ were used to calculate sensitivity, specificity and accuracy for both FPG and 2HPPG.The sensitivity was calculated by dividing the number of true positives over the number of both true positives and false negatives (FN) for FPG and 2HPPG. The specificity was also calculated by dividing the true negatives (TN) with both the true negative and the false positives. The positive predictive values for both fasting plasma glucose and two hours post prandial glucose was also calculated by dividing the true positives by both true positives and false positives (that is by the total number of positives), while the negative predictive value was determined by dividing the true negatives by both true negatives and false negatives.
3. Results
- A total of 3710 oral glucose tolerance test (OGTT) results were analysed using EPI Info Version 7. One hundred and fifty (150) subjects representing 4% of the total results were diagnosed diabetic when their fasting plasma glucose results alone was used (fig. 1). When the two hour post prandial glucose parameter (2HPP) alone was used, the number of subjects that were diagnosed diabetic was one hundred and sixty (160) subjects (4.3%) (Fig 2).
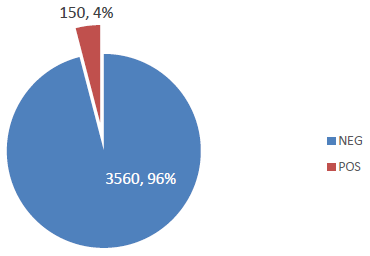 | Figure 1. Outcome of Fasting plasma glucose test |
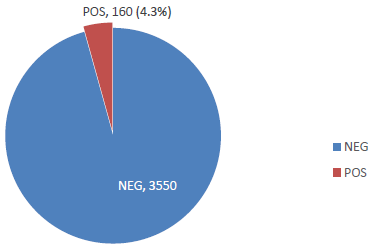 | Figure 2. Outcome of the 2 hours Post test |
|
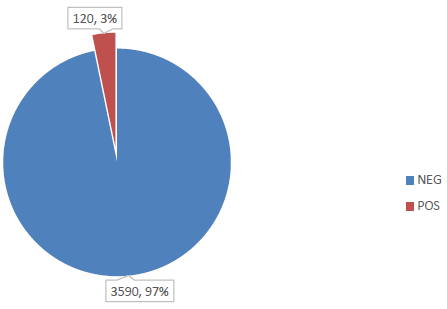 | Figure 3. Outcome of Both Tests |
|
|
4. Discussion
- Diagnosis of diabetes mellitus can be made using fasting plasma glucose (FPG) value of ≥7mmol/l or a random plasma glucose value of ≥ 11.1mmol/l and/or a 2HPPG value ≥11.1mmol/l. Where glycated haemoglobin value is used, a value ≥ 6.5% is defined as diabetic [4]. Each of these diagnostic criteria can be used independent of the others and could give different incidence rates of diabetes mellitus as seen even in this study. (Table 1) Studies have shown that the use of any of these diagnostic criteria influences the incidence and prevalence of diabetes mellitus [7]. This was observed in a study that looked at prevalence of diabetes mellitus using these different diagnostic criteria, where different incidence of diabetes mellitus was observed. When the 2HPPG criteria was used for diagnosing diabetes, there was a slightly higher incidence of diabetes mellitus than with the FPG criteria. The incidence of diabetes would again change when all those that were positive for both FPG and 2HPPG were taken as true positives (fig 3). The incidence dropped from about 4% for FPG and 4.3% for 2HPPG to 3% when both criteria were used simultaneously. (Fig 3)Analytical sensitivity which can be defined as the probability that a test result would be positive when the disease is present [8] was assessed using the results of FPG and 2HPPG against the ‘true positives’. Fasting plasma glucose test had 58% sensitivity while the 2HPPG had 67% sensitivity (table 3). The 2HPPG test was more sensitive for diagnosing diabetes mellitus than FPG in this study. Though both had the same specificity (98%), which is the probability that a test result will be negative when the disease is not there. This meant that both the 2HPPG and the FPG test had equal ability to be negative when the disease is not there, thus reducing the number of false positives and false negative results.The analytical sensitivity and specificity are a measure of diagnostic accuracy [8]. The diagnostic accuracy, therefore, was slightly higher for 2HPPG, since both the FPG and the 2HPPG had about the same specificity but 2HPPG had a slightly higher sensitivity (Table 1). When considering the analytical accuracy of a test, a higher sensitivity and specificity is preferred and this therefore infers that the 2HPPG test can be said to have a better analytical accuracy than fasting plasma glucose, as seen in this study (Table 3). A study showed that more patients above 60 years were diagnosed diabetic when the 2HPPG criterion was used against the glycated haemoglobin criterion [9] (Table 1). This was attributed to delayed insulin response to glucose load [9]. This could also be a possible explanation for the increase diabetes incidence seen with the 2HPPG in this study. In that study, subjects with body mass index (BMI) below 25 were more sensitive to glycated haemoglobin than 2HPPG. In this study though the effect of age and BMI on the various criteria were not specifically evaluated, it could be a possible explanation for the increase incidence of diabetes seen with the use of 2HPPG criterion.The probability that the disease (diabetes mellitus) is present when the test is positive is referred to as the positive predictive value of the test [10]. In this study, it was again higher for 2HPPG (50%) than FPG (47%). Though a higher percentage for the positive predictive value for both tests would be preferred, the slightly higher positive predictive value for 2HPPG means that 2HPPG test had more true positives than FPG, and could therefore be regarded as a better screening tool.Since both 2HPPG and the FPG tests are used as screening test, they are done most times on apparently normal subjects with little or no noticeable symptoms of diabetes. This makes diagnosing the disease, most times, the sole responsibility of the outcome of these test results and therefore very importantly, on the diagnostic accuracy of FPG, 2HPPG test and glycated haemoglobin. The diagnostic accuracy for the 2HPPG in this study was found to be higher than that of FPG test. This finding was in keeping with the results of other earlier studies, [11,12] which compared the diagnostic accuracy of FPG, 2HPPG and glycated haemoglobin and observed that glycated haemoglobin had the highest diagnostic accuracy and was therefore seen as a better screening test, followed by a 2HPPG test. In this part of the world, FPG and 2HPPG are readily available and can easily be done either with analytical kits or point of care testing equipment. The same cannot be said for glycated haemoglobin which is not readily available and where available, is very expensive. (About 10-15 times the cost of FPG). Judging from the economic realities in our environment, the use of glycated haemoglobin as a screening test may be very financially challenging, as well as being relatively unavailable. This has therefore made the use of either FPG or 2HPPG still a convenient alternative in this region. Though there is no consensus amongst professionals whether FPG or PPG is a better predictor of glycaemic control in resource poor settings when HbA1c is not available [11,12]. In this study the 2HPPG had a better accuracy level than FPG and this could be because the 2HPPG test being a dynamic tests, is believed to give a picture of the subject’s metabolic response to glucose load [13] but it is cumbersome to perform, time consuming and slightly more expensive than fasting plasma glucose [14] (about twice the cost of FPG). The disadvantages of glycated haemoglobin and 2HPPG, coupled with the unfavourable economic condition like ours, when weighed against the difference in the accuracy levels of fasting plasma glucose and 2HPPG tests in this study, may make the choice of which diagnostic parameter to use a difficult choice in our environment.
5. Conclusions
- The results of this study suggest that the 2HPPG may be a more accurate screening tool for diabetes mellitus than FPG. Therefore, the use of 2HPPG should be encouraged for targeted screening of diabetes mellitus as this will reduce a false sense of security for those who may have been misdiagnosed using the FPG. In order to strike a balance with regards to affordability of test, the turnaround time of test and diagnostic accuracy, FPG test may be used for mass screening of diabetes mellitus.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML