-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2019; 8(2): 23-29
doi:10.5923/j.diabetes.20190802.02

Effect of Using Mobile Phone Communication on Drug Adherence of Type 2 Diabetes Mellitus Patients at Kitui County Referral Hospital, Kenya
Alice Wairimu Theuri1, 2, Anselimo Makokha1, Florence Kyallo1
1Department of Human Nutrition Sciences, Jomo Kenyatta University of Agriculture and Technology, Nairobi, Kenya
2Department of Food Science, Nutrition and Technology, South Eastern Kenya University, Kitui, Kenya
Correspondence to: Alice Wairimu Theuri, Department of Human Nutrition Sciences, Jomo Kenyatta University of Agriculture and Technology, Nairobi, Kenya.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Despite the increased use of mobile phone communication in Kenya, its application as a management tool in health care remains largely underutilized. This study aimed at evaluating the effect of mobile phone communication on drug adherence amongst Type 2 Diabetes Mellitus (T2DM) patients. This longitudinal study was conducted among 138 T2DM patients attending the diabetes clinic at Kitui County Referral Hospital. A structured questionnaire was used to obtain information on respondents’socio economic and socio demographic characteristics and drug adherence practices. Data was analyzed using SPSS version 21. After six months, the proportion of respondents who took their drugs at specific times increased from 58.2% to 74.6% in the intervention group (IG) compared to a decrease of 47.9% to 46.5% in the control group (CG). The Net Effect of Intervention (NEI) increase of 17.8% was statistically significant (p<0.05). The proportion of respondents who did not miss their diabetes drugs increased from 65.7% to 79.1% in the IG compared to a decrease from 63.4% to 54.9% in the CG, marking a significant NEI increase of 21.9% (p<0.05). Use of mobile phone communication increased adherence to diabetes medication in the aspects of no delayed and missed doses in Type 2 Diabetes Mellitus patients in this study.
Keywords: T2DM, Drug adherence, Mobile phone technology
Cite this paper: Alice Wairimu Theuri, Anselimo Makokha, Florence Kyallo, Effect of Using Mobile Phone Communication on Drug Adherence of Type 2 Diabetes Mellitus Patients at Kitui County Referral Hospital, Kenya, International Journal of Diabetes Research, Vol. 8 No. 2, 2019, pp. 23-29. doi: 10.5923/j.diabetes.20190802.02.
1. Background
- Diabetes is the fourth leading cause of death in the world and its prevalence has been increasing [1]. It is estimated that by 2030, the number of cases worldwide will exceed 400 million [2]. The most common form of diabetes is Type 2 Diabetes Mellitus (T2DM) which accounts for over 90% of diabetes cases [3]. About two-thirds of those with T2DM live in developing countries [4]. In rural Kenya, the prevalence of diabetes is estimated to be 16% [5]. A relatively large number of T2DM patients are treated at Kitui County Referral Hospital diabetes clinic in Kenya. Nearly 50 patients attend the diabetes clinic at the Kitui County Referral Hospital every week [6]. The ultimate goal in diabetes mellitus therapy is to achieve glycemic control [7] and this involves an interplay of self-management measures, including medication schedules [8]. Non adherence to medication is a common problem associated with sub-optimal clinical outcomes and increased health-care costs [9]. To address drug non adherence, the World Health Organization has recommended use of mobile phone technology which is not limited to face-to-face services to manage chronic diseases [10] and more so in diabetes care [11]. The use of mobile phone communication is fast and efficient [12], personal, highly transportable, and has wide acceptance among the patients [13]. In Kenya, the mobile phone subscriptions reached 46.6 million, while the number of short message service (SMS) rose from 816.887 million during the April-June 2018 quarter to 974.569 million during the July to September 2018 quarter [14]. Despite the rise in use of mobile phone communication in Kenya, the technology remains largely underutilized as a management tool in health issues [15]. This study aimed at evaluating the effect of mobile phone communication on drug adherence among patients with Type 2 Diabetes Mellitus at Kitui County Referral Hospital.
2. Method
- This was a longitudinal study that was conducted among T2DM adult patients attending diabetes clinic at Kitui County Referral Hospital during the months of April and May 2017. Data after intervention was collected in November and December 2017. Consenting T2DM patients aged 20-70 years visiting the Out Patient Department (OTP) diabetes clinic and diagnosed with T2DM at least one year before this study were included in the study while patients without mobile phones were excluded from this study. A structured questionnaire was used to collect data on socio economic characteristics and drug adherence practices of the respondents. The drug adherence practices included delayed and missed doses, travelling with drugs, use of unprescribed medicine and not absconding drugs. The sample size was determined using Krejcie & Morgan (1970) [16] method. The method was chosen because it is relevant for selecting samples from populations as small as 10 and as large as 100,000 where the population of patients suffering from T2DM seen at Kitui County Referral Hospital lies. The population for this study was taken as N = 200 who were the T2DM patients on follow up for the previous one month [17].s= χ2NP (1-P)/d2 (N-1) + χ2P (1-P)Where:s is required sample sizeχ2 is the table value of Chi-square for 1 degree of freedom at the desired confidence level. In our case we used 95% confidence level which yielded χ2= (1.96) (1.96) = 3.841N is the population sizeP is the population proportion (assumed to be 0.50 since this would provide the maximum sample size)d is the degree of accuracy expressed as a proportion (0.05).Using the formula 3.841(200) (0.5) (1-0.5)/ (0.05) (0.05) (200-1) + 3.841 (0.05) (1-0.05) =132 patients.The calculated sample size was increased by 10% cater for attrition. Therefore, 10/100 of 132=13.2, giving a total sample size of 132+13=145 individuals. Respondents were assigned to either an intervention (IG) or control group (CG). Out of the eligible 200 T2DM patients on follow up from the previous one month [17], 138 (67 in the intervention group and 71 in control group) completed the two phases of the study (baseline and after six months). Data was collected at baseline and six months. This intervention took a period of six months. Data on drug adherence was collected before and after the intervention. The intervention group received key messages via mobile phone sent five days in a week for a period of six months. The messages focused on adherence to diabetes drugs. The control group did not get any messages but received the usual care from the hospital. Drug adherence was determined by indications of taking drugs at specific times as required, not missing, or absconding from taking drugs, traveling with drugs and not using unprescribed drugs [18,19].Statistical analysisData was analyzed using SPSS software Version 21. The Net Effect of Intervention (NEI) analysis was used to determine the impact of the intervention at p≤0.05 significance level.Ethical approvalEthical approval was obtained from the Kenyatta National Hospital/ University of Nairobi Ethics and Research Committee (KNH-UON ERC), Permit No.KNH/ERC/R/66. Permission to carry out the study was obtained from the NACOSTI (National Commission for Science, Technology and Innovation), Permit No.NACOSTI/P/17/69901/16738. Each respondent gave informed written and oral consent before taking part in the study.
3. Results
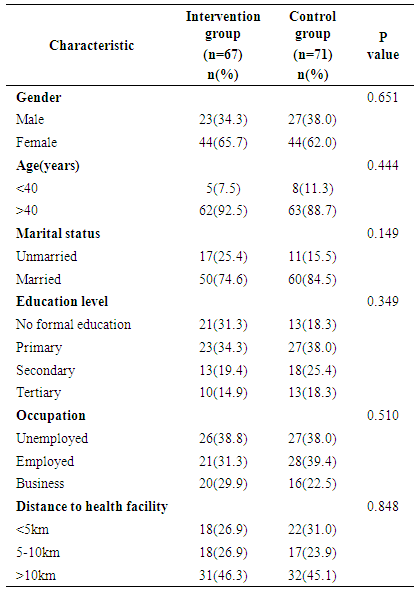
- The socio-economic characteristics of the respondents are presented in Table 1. Majority of the respondents (65.7% in the intervention group (IG) and 62% in the control group (CG)) were females. Majority of respondents were aged above 40 years (92.5% in the IG and 88.7% in the CG). Seventy four percent (74.6%) in the IG and 84.5% in the CG were married. Close to a third (31.3% in the IG and 18.3% in the CG) had no formal education while 34.3% in the IG and 38% in the CG had attained primary education. Less than a fifth (14.9% in the IG and 18.3% in the CG had tertiary education while the rest had secondary education. Majority of the respondents were unemployed (38.8% in the IG and 38.0% in the CG). Close to a third (31.3% in the IG and 39.4% in the CG) were employed and the rest were in business. Majority of the participants (46.3% in the IG and 45.1% in the CG) lived more than 10km away from the nearest health facility and only 26.9% in the IG and 31% in the CG lived within 5km of a health facility. No significant differences were observed between the study groups in terms of gender, age, marital status, education level, occupation and distance to health facility (Table 1).
|
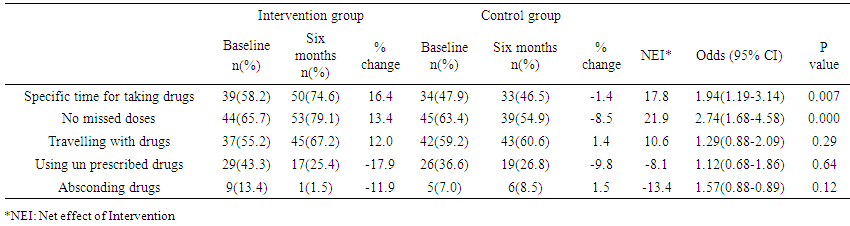 | Table 2. Drug adherence of respondents |
4. Discussion
- Majority of the respondents were female (66% in the IG and 62% in the CG). This is similar to the gender situation in a previous study done in two hospitals on comparison of glycemic control among T2DM patients in Kenya that showed a higher proportion of females (66.5%) compared to males (33.5%) [20]. Similarly, a study in Ghana to assess adherence to and factors associated with self-care behaviors in T2DM patients also had a higher proportion of female (72%) than male participants (28%) [21]. However, there are also some few studies that have reported a lower percent of females attending diabetes clinics compared to males [22,23]. The higher prevalence of females compared to males attending the clinics in many studies has been attributed to better health seeking behavior by women [24]. In this study, majority of respondents were aged above forty years (93% in the IG and 89% in the CG). Type 2 Diabetes Mellitus (T2DM) has been shown to affect mainly populations aged above 40 years [25]. The level of education among patients with T2DM is important to self-care practices and drug adherence. The current study had 31% in the IG and 18% in the CG with no formal education while 34% in the IG and 38% in the CG had acquired primary education. A study in India reported 29.8% with no formal education and 8.1% with primary education [26]. In another study in Bangladesh, 47% of respondents had no formal education and 30% had primary education [27]. Over one third (39% in the IG and 38% in the CG) were unemployed. This implies that the respondents were of a predominantly low socio economic status. A study among diabetes patients in Cote d’Ivoire reported a slightly lower proportion (31%) of unemployed respondents [28]. The results are lower than a study in Libya to assess glycemic control status among T2DM patients where the unemployed comprised 72.8% [29]. The reason for unemployment of respondents could be the study setting as most of the population came from rural areas and therefore opportunities are limited as noted by Maez et al. [30]. Glycemic control is important in T2DM patients as it reduces the risk of diabetes complications [31] that affects their health status and overall quality of life [32]. As Aminde et al. [33] found out, 54.4% of patients with diabetes in Cameroon had poor drug adherence, results that are similar to those in this study. Our study found that >40% of T2DM patients were not adherent to specific drug times. This proportion is higher compared to a study in Palestine by Elsous et al. [32] on T2DM patients that found 11% did not adhere to specific drug times while Sontakke et al. [34] in their study found that 35% of respondents did not adhere to specific drug times. Our study also found that 34% in intervention group and 21% in control group forgot to take their diabetes drugs. These findings are similar to a study by Elsous et al. [32] where 34% forgot to take their medicine. Hernández-Ronquillo et al. [35] reported that a lower proportion (13%) of patients missed doses while Sajith et al. [36] showed that 41% had missed doses. However, a study in Zimbabwe found 63% of respondents had missed the diabetes drugs [37] while Alqarni et al. [38] found that 54% missed their drugs. Huang et al. [10] found an increase of those who had no missed doses from 43.7% to 61% in the control group and 46% to 90% in intervention group after mobile phone intervention. This was significant (p<0.05 in both groups). A study by Vervloet et al. [7] on T2DM found that those in intervention group tended to miss doses less frequently than those in the control (15% vs 19%, p=0.065) while Louch et al. [39] found no significant difference between the groups with respect to self-reported insulin injection after mobile phone intervention. This study found that mobile phone communication had a significant effect on adherence to specific time for taking drugs. These results are similar to other studies that found that intervention with SMS significantly decreased (p<0.05) incidences of delayed doses [7,10]. Vervloet et al. [7] in their study noted that there was a significant difference (p=0.03) between the intervention and control groups in regard to adhering to standardized time windows. The reasons for non-adherence in this study as reported in Focus Group Discussion (FGD) were forgetfulness, travelling away from home and side effects of medication which are similar to those reported in other studies [40,41]. There was a high proportion of respondents not travelling with drugs (>40% in intervention and in control group). This is higher compared to studies on T2DM patients in Cameroon [33] and Mexico [35] where 27% and 13% did not travel with their diabetes drugs respectively. The results are lower compared to those by Mandewo et al. [40], who found that 55% of respondents did not travel with their drugs. The proportion of respondents using unprescribed drugs in both groups was low (<50%) at baseline and after six months, probably because of fear of being reprimanded. In their study on T2DM patients, Sontakke et al. [34] found that 45% of respondents took additional non prescribed medicine. Some diabetes drugs have been associated with treatment failure [42] and some patients believe that diabetes is curable as reported by Shah et al. [43]. Consequently patients may resort to use of herbal remedies [44] and over the counter medicine [45]. This may lead to drug interactions that further lead to pharmacologic inefficacy and side effects [45]. Given that diabetes mainly affects populations aged above 40 years, this leads to a decline in immune function [46] that in the long run calls for more pharmacology and this is likely to lead to adverse drug interaction [45]. It is for this reason that use of unprescribed drugs in T2DM patients should be discouraged. In addition, treatment failure may lead T2DM patients to abscond diabetes drugs as shown in this study. Other studies [19,32-34,47] reported that 5%-60% of T2DM patients absconded diabetes drugs. This may be because after a long duration of treatment, patients feel better or some give up treatment. Poor drug adherence in this population is a worrying trend given the high rates of diabetes in Africa and more so in Kenya [8]. Similar high rates of non-adherence have been reported in Cameroon (54%) [33] while lower rates have been reported in Uganda (16.7%) [42]. This might imply that inadequate attention is given to diabetes or might be attributed to forgetfulness. Majority (46% in the IG and 45% in the CG) of patients in this study lived 10km away from a facility, another possible reason for the low drug adherence. Poor cognition, which is common among the elderly, could also be a potential reason, considering that over 85% of respondents in this study were aged over forty years of age. This in turn may lead to poor drug adherence [48]. The high prevalence of unemployment could also be a factor since socio economic factors are related to medication adherence [32]. Given that diabetes patients in Kenya pay for their medicines, this may lead to poor drug adherence as drug costs and affordability are recognized challenges to controlling chronic diseases especially in low income settings [49,33]. Poor drug adherence could also be attributed to poor knowledge [50]. From the FGD, most respondents cited forgetfulness as one patient stated, ‘Since I work away from home, most drug times I am away and sometimes I forget to travel with the medication’. Another patient cited financial constraints. ‘I live far from home and sometimes I miss bus fare to go to the hospital and purchase the drugs’. The acceptable cutoff point for adherence rate is 80% or higher [38]. The present study is in agreement with WHO report that adherence to long-term therapy for chronic illnesses in developed countries is 50% and is even lower in developing countries [51]. Given the fact that this study relied on patients’ recall, the actual and true prevalence of drug adherence could be lesser than the reported proportions. It is important to motivate patients to take the medications as prescribed. The use of SMS can offer a promising intervention in diabetes and this can go a long way in managing the high cases of drug non adherence that is associated with sub-optimal clinical outcomes as stated above. The use of SMS messaging to improve medication adherence has also been demonstrated by other studies [9,52,12,53]. In the Thai study by Khwankhom [53], patients with tuberculosis who received daily SMS reminders improved drug adherence to over 90%. Though other studies [7,54,55] have demonstrated that the use of SMS did not lead to improved drug adherence our study showed positive results. More specifically, the use of mobile phone communication improved adherence to the time for taking diabetes drugs and with no missed doses. Bearing in mind that forgetfulness has been cited as one of the reasons leading to poor drug adherence in T2DM patients [33] use mobile phone communication in diabetes clinics could be effective since it resulted in improved adherence to drugs. The technology can also be used in other low income countries.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML