-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2019; 8(2): 17-22
doi:10.5923/j.diabetes.20190802.01

Balance Assessment during Cognitive Dual Task Performance in Diabetic Peripheral Neuropathy
Nawal A. Abo Shady1, Shaimaa I. El-Jaafary2, Ibrahim M. Hamouda3, Radwa Y. Mohammad1
1Department of Physical Therapy for Neuromuscular Disorders & its Surgeries, Faculty of Physical Therapy, Cairo University, Egypt
2Department of Neurology, Faculty of Medicine, Cairo University, Egypt
3Department of Physical Therapy for Neuromuscular Disorders & its Surgeries, Faculty of Physical Therapy, Kafrelsheikh University, Egypt
Correspondence to: Radwa Y. Mohammad, Department of Physical Therapy for Neuromuscular Disorders & its Surgeries, Faculty of Physical Therapy, Cairo University, Egypt.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: Diabetes Mellitus results in an impairment of cognitive tasks. Few studies addressed the effect of cognitive –motor dual task in Diabetic Peripheral Neuropathy patients. The purpose of this study was to assess the influence of cognitive dual task on balance, Comparisons between effect of the single-task and dual-task on balance and to implement cognitive dual tasking in balance rehabilitation in DPN patients. Subjects and Methods: This study is a cross section design included 60 female subjects distributed into 3 groups, GI included 20 patients with sensory DPN, GII included 20 patients with sensory-motor DPN and GIII included 20 healthy age-matched subjects participated in the present study. The age ranged from 50 to 60 years old. Subjects were assessed by Montereal Cognitive assessement (MoCA) and Biodex Balance system (BBS). The performance of patients and healthy subjects was compared on BBS, on mental task (verbal fluency) and when performing the mental task while balancing. Results: There was a significant decrease in MoCA in Group I & II. There was a significant increase in overall stability index (OVSI), antero-posterior stability index (APSI) and medio-lateral stability index (MLSI) at dual task compared with that at single task in group I and II (p < 0.01). However, there was no significant difference in OVSI, APSI, and MLSI between single and dual tasks in group III (P > 0.05). There was significant decrease in number of words at dual task compared with that at single task in the three groups (p < 0.001). Conclusion: This study is the first to demonstrate the effect of cognitive –motor dual task in DPN patients on balance and cognition. The results support the view that motor control is influenced by cognitive function. So it is important to implement cognitive training as postural control demands attention under certain circumstances.
Keywords: Dual task, Balance, Diabetic Peripheral Neuropathy, Biodex Balance System
Cite this paper: Nawal A. Abo Shady, Shaimaa I. El-Jaafary, Ibrahim M. Hamouda, Radwa Y. Mohammad, Balance Assessment during Cognitive Dual Task Performance in Diabetic Peripheral Neuropathy, International Journal of Diabetes Research, Vol. 8 No. 2, 2019, pp. 17-22. doi: 10.5923/j.diabetes.20190802.01.
Article Outline
1. Introduction
- Diabetic peripheral neuropathy (DPN) is the most common complication associated with diabetes mellitus. DPN is defined as a 'symmetrical, length-dependent sensorimotor polyneuropathy attributable to metabolic and microvessel alterations as a result of chronic hyperglycaemia exposure and cardiovascular risk covariates' according to The Toronto Consensus Panel on Diabetic Neuropathy [1]. Neuropathy progression follows a distal-to-proximal gradient so the effects of DPN on strength and balance are most evident at the ankles and feet, sites of the distal endings of large, myelinated motor and sensory fibers. The loss of nerve function can have dramatic implications for both standing and walking tasks [2].Balance is defined as the ability to maintain line of gravity within base of support with minimal postural sway. Balance requires multiple sensory systems coordination including, vestibular, somatosensory, and visual systems [3]. Diabetic population is at high risk of fall with an overall incidence of 1.25 fall/person-year and increases with neuropathy due to poor peripheral sensation [4]. Most of studies reported higher instability during standing in diabetic patients with PN compared with diabetic patients without PN and healthy control subjects during standing [5]. Balance is the most basic requirement to prevent falling, activities of daily living performance and independent life [6].Diabetes has long-term complications in the brain, which are poorer cognitive ability and more abnormalities seen with brain imaging compared with people who do not have diabetes [7]. The incidence of dementia in patients with diabetes was increased by 50–100%, relative to non-diabetic individuals. This increased risk involved both Alzheimer’s disease with a ∼ 50–100% and vascular dementia with a∼100% [8]. The dual-task is the concurrent performance of two tasks that can be performed independently and have distinct and separate goals [9]. Task- oriented activities are functional movements that are essential for actual living. A number of studies have attempted to reduce fall risk by improving dual tasking in a variety of populations who are at a high risk of falls [10].
2. Material and Methods
2.1. Subjects
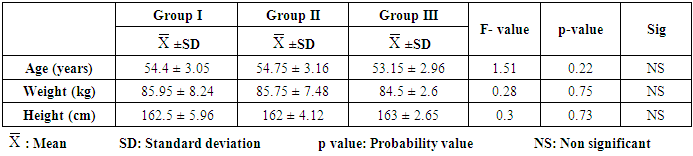
- A total of 60 participants were included in this study divided into 3 groups (GI includes 20 patients with sensory DPN, GII includes 20 patients with sensory -motor DPN and GIII includes 20 healthy age-matched volunteer subjects). The descriptive characteristics of the participants are presented in Table 1. the included subjects were Medically diagnosed with type 2 diabetes and stable, under diabetic control, their age were between 50 and 60 years, had the ability to stand on both feet, Duration of diabetes was more than 10 years and cooperative subjects with ability to understand instructions and follow simple verbal commands & simple calculations. Selection of patients was based on careful clinical assessment, and neurological examination. The patients were recruited from Kasr El-Aini Hospital, Faculty of Medicine, Cairo University and National Institute of Diabetes & Endocrinology. Participants were excluded if they had foot ulcer, Foot amputation. Lack of blood sugar control, Internal ear infections, Visual problems or blind, Non-diabetic neuropathy (due to Charcot–Marie–Tooth disease or alcohol), Other diseases affecting balance, musculoskeletal problems such as vertebral column and limb deformity, History of repeated ankle sprains in the year before, Severe pain influencing balance, Any clinically significant medical or psychiatric condition (including Dementia or Alzheimer’s) and finally unwillingness to be in the study. The study was approved by ethical committee of Faculty of Physical Therapy, Cairo University. All the participants read and signed the sample consent form after receiving information about the study purpose, assessment procedures, possible benefits, privacy and use of data to ensure full cooperation from each patient.
|
2.2. Instrumentation
- i. Montreal Cognitive Assessment (MoCA): it was a one-page 30-point test administered in 10-minutes. It was designed as a rapid screening instrument for mild cognitive dysfunction, possible score is 30 points; a score of 26 or above is considered normal. The sensitivity of MoCA is 4.5 times that of mini-mental scale in detection mild cognitive impairment. It evaluates different cognitive domains: attention and concentration, executive functions, memory, language, visuoconstructional skills, conceptual thinking, calculations, and orientation [11]. The Arabic version was used for our patients [12].ii. Biodex Balance system (BBS): it consists of Multiaxial standing platform, it can be tilted to 20 degree which permits the ankle joint mechanoreceptors to be stimulated maximally [13]. All trials were done with barefoot and Foot position was recorded using coordinates on the platform's grid be sure of consistency of the test [14].iii. Electronic stopwatch and Voice recorder: Electronic stopwatch helped in counting down for tasks need 60 seconds. Voice recorder was used to be sure that there wasn't any repetition of words and counting number of words that was told during the verbal fluency test.
2.3. Procedure
- The study used a dual task design to investigate interference between concurrent performance of mental and balance tasks in normal subjects and patients who suffer from Diabetic peripheral neuropathy. Each subject was tested under 3counterbalanced conditions:Performing mental task (Verbal Fluency Test) while sitting, was a very useful test that was used to evaluate executive functions and language. Category fluency test seems to be more sensitive than the phonological test [15]. Subjects were asked to name fruits over a period of 1 minute. Total scores was the number of fruits named in 60 s.Standing on Biodex Balance System, in this study the platform stability was selected to be at level 8. The data generated from this test were in the form of balance index which included: Overall balance index, Anterior/Posterior index (A/P) & Medial/Lateral index (M/L). High values resembled balance disturbance (increase rate of body swaying during the test).Performing mental task on Biodex Balance System, maintaining balance on BBS and Verbal Fluency Test at the same time. To minimize order effects the order of the postural and mental task conditions was counterbalanced across subjects, a minimum of one single task baseline balancing trial was discarded as a practice trial, and subjects were permitted to sit between trials if they felt fatigued, If overbalancing occurred during a test (using hand rails or requiring steadying by the rater) the measurement was stopped and the test repeated.Descriptive statistics and ANOVA-test were conducted for comparison of the mean age, weight and height between the three groups. Two-way mixed MANOVA test was conducted to compare the effect of task (single versus dual) and the effect of groups (between groups), as well as the interaction between task and group on mean values of postural stability, limits of stability, cognition verbal fluency and cognition arithmetic.
3. Results
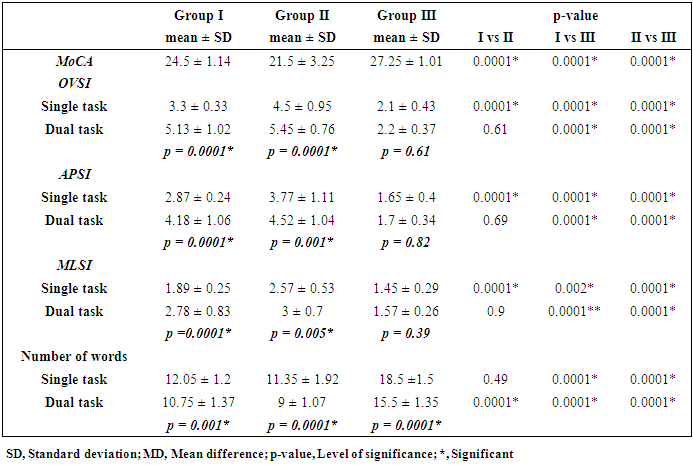
- There was a significant difference between the three groups in the mean value of MoCA (p = 0.0001). Group III > I >II (p = 0.0001).Effect of task and group on APSI, MLSI, OVSI and number of wordsMixed MANOVA revealed that there was a significant interaction of task and group (F = 6.25, p = 0.001). There was a significant main effect of task (F = 50.29, p = 0.001). There was a significant main effect of group (F = 39.17, p = 0.001). Table 2 showed descriptive statistics of APSI, MLSI, OVSI and number of words and the significant level of comparison between groups as well as significant level of comparison between single and dual tasks in each group.
|
4. Discussion
- The aim of the study was to assess the influence of cognitive dual task on balance in patients with DPN, comparisons between effect of the single-task and dual-task on balance and to implement cognitive training especially dual tasking in balance rehabilitation in patients with DPN.In this study females were selected as in diabetes mellitus the males were widely affected in cognitive functions [16]. So it was needed to know the effect of DPN on females. Also, most of male patients have foot ulcers and toe amputee which were exclusion criteria.The results showed mild cognitive impairment in DPN groups compared to control group this result agreed with Bhardwaj et al concluded that T2DM patients with DPN have impaired cognition as validated by delayed P300 latency and as the duration of T2DM increases, the cognitive functions deteriorate [17]. Strachan et al. stated that chronic hyperglycemia in type 2 diabetes mellitus patients significantly damages the velocity of information processing such as working memory and some aspects of attention [18]. Also Thabit et al. proved that there were significant executive impairments, particularly in verbal fluency, on a standardized measure of executive function [19].However the result of study disagreed with Ba-Tin et al who concluded that diabetes, in general, is associated with cognitive dysfunction, but the additional presence of peripheral microvascular disease does not add to cognitive decline [20]. This might be due to change in subjects' age.Mild cognitive impairment in DPN could be explaned by that the changes in cognitive function was induced because of long term of hyperglycemia [21]. Long-time poorly controlled diabetes with alternating high and low glucose levels may worsen neurotransmitter function. Decrease in cerebral blood flow with stimulation of the thromboxane A2 receptor that occur with diabetes could contribute to the inability of cerebral vessels to vasodilate adequately that lead to ischemia. Also hyperglycemia potentiate ischemic damage is lactate accumulation, causing cellular acidosis and worsening injury. Finally, Accumulation of glutamate in case of hyperglycemia and ischemia where Glutamate is an excitatory amino acid neurotransmitter, which causing neuronal damage in the brain [22].There was significant decline in cognitive function in Sensory-Motor DPN than Sensory DPN groups this may be due to progression of DPN because of uncontrolled glucose level.However Moreira et al contradict with the present study where Moreira concluded that cognitive impairment does not seem to be related to the presence and/or severity of PDN [23]. This was due to short duration of diabetes mellitus.The result of postural stability test showed significant increase in OVSI, APSI and MLSI at dual task compared with that at single task in DPN patients which resembled balance disturbance (increase rate of body swaying during dual task). And significant decrease in number of words at dual task compared with that at single task. The data indicate that DPN patients demonstrate impairment in cognitive and motor functions during dual‐tasks compared with controls. These impairments were compared with single‐task in both the cognitive and motor functions.These results agreed with Pellecchia who concluded that the cognitive tasks were given with graded difficulty. The results showed the postural sway increased as difficulty of the cognitive task increased [24]. Also, Huxhold et al. and Shumway-Cook et al. supported the U-shaped relationship of attentional demanding tasks and postural [25,26]. Finally Brauer concluded that the patients took more time and were less efficient to correct posture in dual tasking conditions, where as healthy subjects showed a smooth and correct pattern without effort [27].Howerver, this study disagreed with Vuillerme and Nafati who concluded that increased attention during a reaction-timed cognitive task increases muscular stiffness and, subsequently, postural control [28]. The discrepancy between this study and the present study was due to change in methodology and may be by training as there was consistent evidence that both physical and cognitive training combining them in simultaneous way amplifies their efficacy.This finding provides initial evidence that dual tasking impairs balance in DPN patients which could be explained by the U-shaped relationship of attentional demanding tasks and postural sway based on Yerkes–Dodson law. The law states that "performance increases with physiological or mental arousal, but only up to a point. When levels of arousal become too high, performance decreases'' [25].The anterio-posterior stability index showed increase the incidence to fall forward or backward than to fall right or left side in medio-lateral stability index in single and dual task so must be careful to minimize risk of falls in DPN patients by balance exercise.Despite of the important conclusions observed in this study some limitations of the must be known Psychological aspect of the patients during assessment procedures, Cooperation of the patients during the conduction the study and Patients' life style.
5. Conclusions
- DPN patients had cognitive impairment that negatively affected the motor control. So it is important to implement dual tasking in balance rehabilitation as it concerned in all ADL especially this age that range from 50-60 are still working and must be independent. Also, to slow down or overcome the complications of dual task and balance.
ACKNOWLEDGEMENTS
- Special thanks for Dr. Manar Elsayed Ismaiil, Dr. Sobhy Mahmoud Aly for their valuable effort and continuous encouragement during this work.
Abbreviation
- Montereal Cognitive assessement (MoCA), Biodex Balance system (BBS), overall stability index (OVSI), antero-posterior stability index (APSI) and medio-lateral stability index (MLSI), Diabetic peripheral neuropathy (DPN) Activity of daily living task (ADL)
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML