-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2018; 7(2): 36-40
doi:10.5923/j.diabetes.20180702.03

Factors Associated with Poor Glycemic Control among Patients with Type 2 Diabetes in the Southeast Region of Brazil
Débora Gonçalves da Silva, Luiz Alberto Simeoni, Angélica Amorim Amato
School of Health Science, University of Brasilia, Brazil
Correspondence to: Débora Gonçalves da Silva, School of Health Science, University of Brasilia, Brazil.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Brazil is an upper middle-income country with the fourth higher prevalence of diabetes and the fifth in diabetes-related health expenditure. By monitoring the factors related to glycemic control is critical to design and implement policies to reduce the morbidity and mortality of the disease. The aim of this study was to investigate the status of glycemic control and the factors associated with poor glycemic control among diabetics from the Southeast of Brazil. Methods: Data from 656 patients with diabetes attending public and private Endocrinology units were analyzed after reviewing medical records for sociodemographic, clinical and biochemical features in the northwest region of Minas Gerais, Brazil. We also investigated the factors associated with poor glycemic control among patients with type 2 diabetes (T2D). Results: Most patients were female with T2D, median age of 55.1 years and a median time since diabetes diagnosis of less than 5 years. Over 60% of patients had glycosylated hemoglobin (HbA1c) levels over 7%. Factors associated with poor glycemic control among patients with T2D were schooling for less than 4 years, longer time since diabetes diagnosis, treatment with insulin and less frequent follow-up with endocrinologists and dietitians. Conclusion: Our findings confirm data from previous studies indicating that educational level, duration of diabetes, and less frequent follow-up by endocrinologists and dietitians may negatively affect glycemic control. It is therefore possible that health policies focusing patients with these features might favorably affect glycemic control among patients with T2D.
Keywords: Diabetes, Glycemic control
Cite this paper: Débora Gonçalves da Silva, Luiz Alberto Simeoni, Angélica Amorim Amato, Factors Associated with Poor Glycemic Control among Patients with Type 2 Diabetes in the Southeast Region of Brazil, International Journal of Diabetes Research, Vol. 7 No. 2, 2018, pp. 36-40. doi: 10.5923/j.diabetes.20180702.03.
1. Introduction
- Diabetes is one of the most prevalent chronic-degenerative diseases worldwide. According to the International Diabetes Federation, approximately 415 million people were affected in 2015, and this number should reach 642 million by 2040. The disease is also a major concern due to its high mortality rates and health care associated costs [1].Diabetes has historically had a higher burden in high-income countries, but the disease is growing rapidly in low-to-middle-income countries. Data from a large study analyzing 198 countries between 2000 and 2008 indicated that overall diabetes prevalence grew by two percentage points between 1990 (7.4%) and 2008 (9.4%), with a similar level of growth for low-to-middle income countries (7.5–9.3%) [2]. Accordingly, another study involving 4372 million participants in 200 countries showed that low and middle-income countries replaced European countries on the list of the top ten countries with the highest prevalence of diabetes [3].This shift in diabetes prevalence in lower income countries may have a major impact in the morbidity and mortality of the disease, given to the many problems these countries face in providing appropriate care for patients with the disease [4]. Brazil is an upper middle-income country with the third highest number of children with type 1 diabetic (T1D) and the fourth largest number of people with type 2 diabetes (T2D) [1, 5]. Despite the well-established impact of glycemic control on the development of the vascular complications of diabetes, most patients do not achieve treatment goals, similarly to the situation worldwide [6, 7]. This underscores the need for more effective approaches to manage the disease, centered on each local scenario to establish factors related to poor glycemic control. Paracatu and João Pinheiro are the cities with the first (91,724) and third (48,472) largest number of inhabitants in the Northwest of the state of Minas Gerais, respectively. Both cities have a gross domestic product per capita of $7,234, slightly below the overall Brazilian gross domestic product per capita [8]. The aim of this study was to describe variables related to glycemic control in patients from these two cities, and examine the factors related to poor control.
2. Methods
- This was a cross-sectional study based on primary data collected from the medical records of all patients with diabetes who were attending the Endocrinology Outpatient Units from the Cities of Paracatu and Joao Pinheiro, from June to December of the year 2016. The diagnosis of diabetes was defined according to the American Diabetes Association (ADA) criteria [9] or when it was clearly stated in the medical records that the patient had a clinical diagnosis of the disease and was receiving anti-hyperglycemic treatment. We excluded pregnant women and patients without glycosylated hemoglobin (HbA1c) assessment of the previous 12 months. A structured questionnaire was used to collect information about socio-demographic, lifestyle, clinical, biochemical and diabetes follow-up characteristics. The study was approved by the local Ethics Committee of the Hyarte Education Center from Atenas Faculty, in Paracatu, and was performed according to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [10].Statistical analysisThe planned sample size was 563 subjects with diabetes. We determined this sample size considering the estimated prevalence of diabetes of 10.2% in Brazil [1], an absolute precision of 2.5% and a level of significance of 5%.Data from the questionnaires were tabulated to generate a database. Qualitative data were described as frequencies and quantitative data were described as median and interquartile range, since they were not normally distributed, as assessed using the Shapiro-Wilk test. Glycemic control was defined as satisfactory or not on the basis of HbA1c levels (< 7 and > 7%, respectively). Participants with satisfactory or unsatisfactory glucose control were compared with respect to socio-demographic, lifestyle and clinical variables using the Fisher or chi-squared tests. Statistical significance was considered when p values were less than 0.05. All tests were performed using the software GraphPad Prism (version 6.0).
3. Results
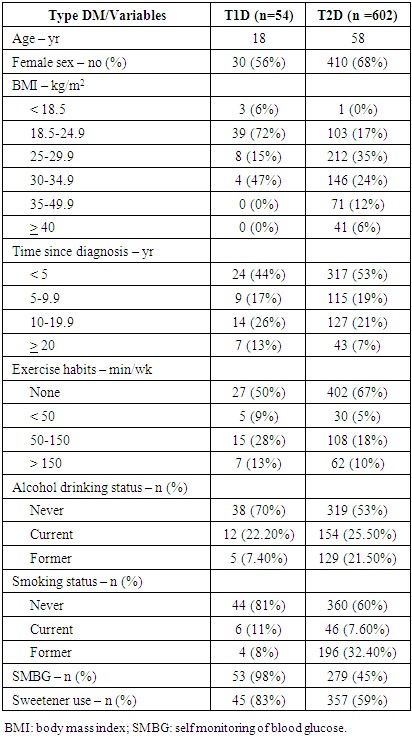
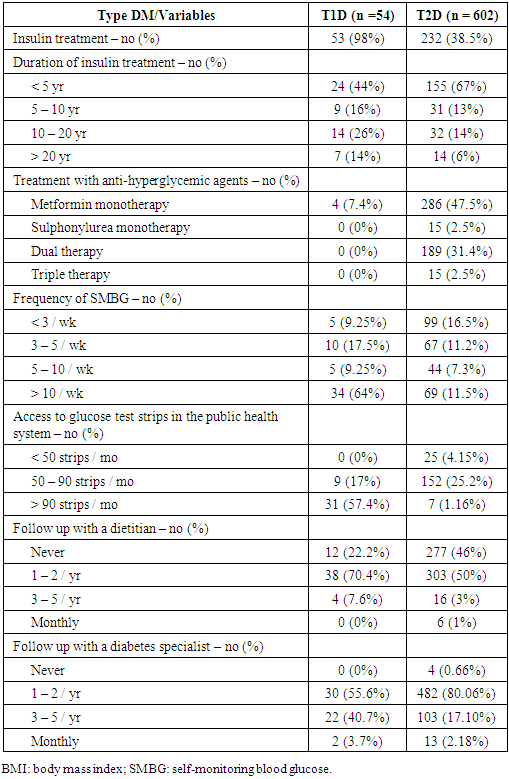
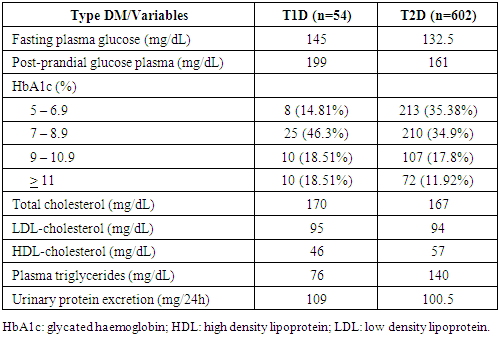
- We reviewed the medical records from a total of 656 patients (54 with T1D and 602 with T2D), and their demographic and clinical characteristics are shown in Table 1. The median age varied with the type of dysglycemia and most patients were female, particularly those with T2D. Most patients with T1D were of normal weight, had less than 5 or from 10 to 20 years since the diagnosis of the disease and self-monitored blood glucose levels frequently. Patients with T2D were mostly overweight or obese, had less than 5 years since diabetes diagnosis and did not self-monitor blood glucose levels. Moreover, most patients did not have smoking or drinking habits, and were sedentary.
|
|
|
|
4. Discussion
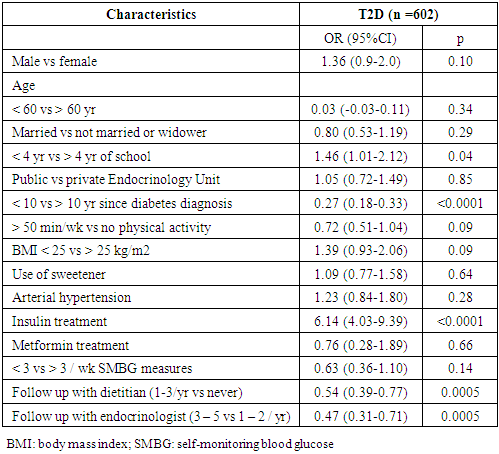
- In this cross-sectional study examining the socio-demographic and clinical characteristics of patients with diabetes in the Northwest region of Minas Gerais, we found that most patients attending outpatient Endocrinology Units were women with T2D and measures of glycemic control above target levels. Our data are in agreement with those from a large Brazilian cross-sectional study involving 6,701 outpatients with T1D (15%) and T2D (85%) aged over 18 years indicating that most patients showed inadequate glycemic control. The authors also reported that patients with a longer period since diabetes diagnosis had worse control and that women who receiving insulin treatment were more likely to reach target HbA1c levels, despite no significant gender difference in glycemic control [11]. Similar studies were conducted in other middle-income countries. A cross-sectional Indian study including 16,607 patients with a mean age of 53 years reported a mean HbA1c level of 8.1%, and that only 31% reached the target value of less than 7%. In concert with our findings, this study showed that treatment with insulin use was associated with poorer glycemic control. The study also found that advanced age, longer duration of diabetes and increased plasma triglyceride levels correlated with HbA1c levels above treatment goals [12].We found a greater number of female patients with T2D attending outpatient Endocrinology Units. Although this finding does not imply a higher prevalence of the disease among women, it is in concert with data from a systematic review of 9 population-based studies involving diabetics at the age of 17 or more in the Caribbean region, which showed a higher prevalence of the disease among women. The authors attributed this to the higher frequency of diabetes risk factors among women, especially obesity [13].We found that among patients with T2D those with less than four school years had a 46% increase in the chance of showing HbA1c levels above the target. Low education level is associated with overall poor health [14], and may also negatively affect glucose control [15, 16]. Similarly to our findings, a study in Israel involving 228,846 patients (mean age of 60 years) reported that poor glycemic control was associated with a lower education level, in addition to young age, longer duration of diabetes and belonging to an ethnic minority [17]. Moreover, higher education level was correlated with better knowledge about diabetes complications and greater adherence to diet, despite not having a better glycemic control [18]. However, the association between education level and diabetes control is not well-established, since other studies addressing this have shown no relationship, despite including a similar proportion of patients with HbA1c above the target levels [19]. We found a high frequency of obesity among patients with T2D, but not T1D. However, this frequency was lower than that observed in the United States. In the latter country, a study of electronic medical records data from 38 states between 2009 and 2011, with data from 259,595 patients, revealed that 47.8% of patients with T1D were obese, whereas 63.4% of those with T2D were obese. The authors also reported a high frequency of HbA1c above target levels [20].Our findings also indicated that most patients with T1D and T2D were sedentary. Similar results were described in another Brazilian study carried out in Sao Paulo, with patients aged between 60-69 years, in which over 85% of the subjects reported no physical activity [21]. Exercise is a major component of T2D treatment due to its beneficial impact in insulin resistance. The effect of physical exercise in increasing insulin sensitivity is significantly maintained for about 60 hours after the exercise session and returns to baseline levels after 3 to 5 days. A trial conducted in France, with a 1-year follow-up intervention of 26 patients with T2D, involving a 3-week residential programme combining high exercise volume (15-20 hours/week) and restrictive diet (500 kcal/day), showed that 54% of patients stopped/decreased their medications following the intervention, whereas only 19% increased or introduced new drugs [22]. Although physical activity was shown to be protective among patients with T2D, we found no association between physical activity and better glucose control. This is possibly explained by data collection from the medical records, which may have impaired a precise analysis of exercise intensity and regularity by study subjects, and by limited sample size. There was also no association between a smaller BMI and better glucose control, possibly explained by the small sample size.Despite the data from our study and many others indicating that a low proportion of patients with diabetes reach glycemic goals, a study conducted in Brazil indicated a decline in diabetes-attributed mortality among adults aged 30 to 69 years, between 1996 and 2011, especially among women. The reasons for this are not completely understood, but it has been discussed that it may reflect increased primary coverage by the local health system, the introduction of the national plan for diabetes to ensure access to insulin since 1991, the national plan to reorganize the care of patients with diabetes and hypertension since 2001, and the national program of pharmaceutical provision for hypertension and diabetes since 2002, ensuring the distribution of tax-free supplies and drugs for patients with diabetes [23].Our data also indicated that a high rate of diabetics treated with insulin do not achieve glycemic control goals. The association between insulin treatment and poor diabetes control is reported in other countries. A study conducted in a university hospital in Malaysia between 2009 and 2014, involving 220 diabetic patients with established cardiovascular disease and a mean age of 64 years, showed that insulin therapy was more frequent among patients with more severe comorbidities, and that insulin therapy was associated with poor disease control, with over 60% of the patients showing HbA1c greater than 8% [24]. However, it should be pointed that this study, similarly to ours, was cross-sectional and the relationship between insulin treatment and poor control may not be a causal one. Indeed, it is more likely that the inertia in starting insulin therapy and also in adjusting it to reach glycemic goals may lead to treatment being considered to patients with more comorbidities and difficulties in reaching control. In keeping with this, insulin was used predominantly in the group of patients with longer duration of diabetes, and this could reflect the difficulty in achieving adequate control in the setting of beta cell pancreatic failure, not due to insulin treatment per se.
5. Conclusions
- Our findings indicate that most patients being followed up at public and private Endocrinology units in the Northwest region of Minas Gerais are middle-aged women, with poor glycemic control. Moreover, the factors associated with poor control among patients with T2D were a lower education level, prolonged time since diabetes diagnosis, insulin treatment and less frequent follow-up with dietitians and endocrinologists. However, these findings may not generalizable to the overall population with diabetes given that study participants were mostly women with less than 5 years since the diagnosis of the disease. Moreover, due to its cross-sectional design, it is not possible to establish the cause-effect relationship between these factors and glycemic control from the current findings. Notwithstanding, they point to the need of establishing an effective multidisciplinary program that can address the multiple variables that interfere in the complexity of this challenging disease, especially in lower-income countries.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML