-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2017; 6(4): 73-82
doi:10.5923/j.diabetes.20170604.01

Influence of Visual Feedback Training on Distribution of Foot Pressure in Diabetic Neuropathy Patients
Gehan M. Ahmed1, Rania M. Tawfik1, Hanan A. Amer2, Waleed T. Mansour1, Hanan H. Battesha1
1Department of Physical Therapy for Neuromuscular Disorder and Its surgery, Faculty of Physical Therapy, Cairo University, Cairo, Egypt
2Department of Neurology, Faculty of Medicine, Cairo University, Cairo, Egypt
Correspondence to: Rania M. Tawfik, Department of Physical Therapy for Neuromuscular Disorder and Its surgery, Faculty of Physical Therapy, Cairo University, Cairo, Egypt.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background and Purpose: Neuropathies are the most common long-term complications of diabetes that affecting up to 50% of patients and considered a major risk factor for the development of plantar ulceration. The goal of this study was to investigate the effect of visual feedback training on re-distribution of planter pressure during standing posture in diabetic peripheral neuropathy patients as a trial for finding a method for reducing the risk of foot ulcer. Patients and Methods: This study was conducted on thirty diabetic patients from both sexes with mild peripheral neuropathy, their ages ranged from 45 to 60 years. The patients were randomly assigned into two equal groups. The study groups A (GA) received visual feedback training by using Biodex Balance System in addition to a selected physical therapy program. The control group B (GB) received the selected physical therapy program only. Results: The results revealed that, in the study group (A) there was a significant increase of plantar pressure at right and left heel, while there was a significant decrease of plantar pressure at right and left big toe and no significant differences of plantar pressure at right little toe post treatment. While in the control group (B) there was no significant difference of plantar pressure at right and left heel, big toe and little toe post treatment. Conclusion: Visual feedback training in addition to the selected physical therapy program was more effective than using the selected physical therapy program only for redistribution of foot planter pressure in diabetic neuropathy patients.
Keywords: Neuropathies, Diabetic peripheral neuropathy, Planter pressure, Visual feedback training
Cite this paper: Gehan M. Ahmed, Rania M. Tawfik, Hanan A. Amer, Waleed T. Mansour, Hanan H. Battesha, Influence of Visual Feedback Training on Distribution of Foot Pressure in Diabetic Neuropathy Patients, International Journal of Diabetes Research, Vol. 6 No. 4, 2017, pp. 73-82. doi: 10.5923/j.diabetes.20170604.01.
Article Outline
1. Introduction
- Diabetes Mellitus (DM) is a group of metabolic diseases in which a person has a high blood sugar, either because the pancreas does not produce enough insulin(diabetes mellitus type I, the first recognized form), or because cells do not respond to the insulin that is produced (diabetes mellitus type II, the more common form) [1].Diabetic peripheral neuropathy (DPN) is a damage or disease of nerves of the peripheral nervous system. Depending on the type of nerve affected secondary to diabetes mellitus; the sensation, movement, gland or organ function, and other aspects of health can be affected [2].Diabetic sensory polyneuropathy (DSP) is a major risk factor for the development of plantar ulceration. Because of the loss of protective sensation, patients with diabetes mellitus and peripheral nerve damage are at very high risk for developing neuropathic ulcer on planter surface of their feet which can lead to lower extremity amputation [3]. Moreover, neuropathy gives a dry fissured skin which leads to abnormal distribution of pressure in the foot when standing or walking [4].The abnormal pressure distribution in the foot resulting in an increased load under the forefoot and rear foot with an increase in the variability of plantar pressure during barefoot gait. The progression of DPN was not found to influence plantar pressure distribution however postural sway can affect the plantar pressure distribution [5].Effective balance training can improve context-specific instabilities of postural control of diabetic peripheral neuropathy patients. Training that compensates for disordered balance indicated by subclinical constraints with the guidance effect of external visual feedback can improve standing postural control in DPN patients [6].So, this study was conducted to re-distribute foot pressure in DPN patients by using visual feedback training as a trial for finding a method for reducing the risk of foot ulcer.
2. Patients and Methods
2.1. Patients’ Selection
- This study was conducted on thirty patients with diabetic peripheral neuropathy (DPN). The patients were selected from the out Patient Clinics of Neurology and Internal Medicine in Kasr Al- Ainy Hospitals and Out Patient Clinic of Department of Neurology, Faculty of Physical Therapy, Cairo University in the period from August 2015 to May 2016.Patients were randomly assigned into two groups of equal number using the roll of a dice, study group take (odd number) while control group take (even number). Patients were divided according to the treatment procedure into two groups equal in number to investigate the effect of visual feedback training on distribution of foot pressure.Inclusion criteria include patients have type II DM with symptoms and signs of mild (grade one) peripheral sensory neuropathy, duration of illness ranged from 5:20 years and the body mass index (BMI) ranged from 20:30 Kg/ m2.Exclusion criteria were history of pedal ulcer in the lower limb or amputation, advanced arthritis and osteoporosis in the lower limbs, recent or old mal union fractures of lower limbs, significant scar tissue or calluses on the feet, peripheral vascular diseases as varicose veins, balance disturbance rather than diabetic peripheral neuropathy (ear problems, Labyrinthitis, or cerebellar problems), visual disturbances, obesity (BMI more than 30 kg/m2), severe sensorimotor or autonomic neuropathy, acute nerve root compression (radiculopathy) affecting lower limbs, previous neurological problems as spinal cord injury or stroke and foot deformities or long leg discrepancy that impairing standing balance.
2.2. Instrumentations
- - Weight and height scale was used to measure the weight and height of all patients before starting the assessment for determining BMI.- Right Stride (RS) scan foot plate system (Tekscan, Inc. 307 west First Street South Boston, MA.02127-1309, USA) was used to identify the absolute peak pressure under the three planter areas on each foot (first metatarsophalangeal, fifth metatarsophalangeal, and centre of the heel). Reliability of this device was assessed using both the mean and the median values of three repeated trials. The system displayed moderate to good reliability of mean and median calculations for the three analysed variables across all regions of the foot [7].- Biodex Balance System (Biodex Medical Systems Inc., Brookhaven R&D plaza, 20 Ramsey Road Box 702, Shirley, New York 11967-0702) was used for treatment in the study group to improve balance and somatosensory awareness.
2.3. Procedures
2.3.1. Evaluation Protocol
- -All patients were submitted to the following:a) Clinical examinations: 1) The patients were examined by the neurologist according to the sheet of Department of Neurology of kasr Al Ainy Hospital, Cairo University (appendix I) for sensory and motor manifestations.2) Random serum glucose levels were done to ensure that the glucose level was controlled for all patients.3) The degree of neuropathy graded according to the grading neuropathy scale [8].4) Determination of body mass index: BMI was calculated according to the following equation:
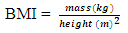 | (1) |
2.3.2. Treatment Protocol
- Patients were assigned into two groups equal in number:Group A (study group): (9 females and 6 males) received visual feedback training with Biodex Balance System for 12 sessions (every other day). The duration of session was ten minutes and repeated for three times as a total duration of session was about 30 minutes. The study group (A) received additional selected physical therapy program for DPN patients.Group B (control group): (10 females and 5 males) received the same selected physical therapy program for DPN patients without visual feedback training.- Visual feedback training program:The Biodex Stability System was used as visual feedback training to redistribute planter pressure for group (A) at balance lab, Faculty of Physical Therapy, Cairo University. Patient preparation:- The benefit of the system and how it works were explained to each patient.- The patient was instructed to step onto the platform with barefoot. The position of the support handles and its height were adjusted according to patient’s height and comfort. Patients were asked to grasp the supported handle during initiation of treatment session, then to leave it gradually as the treatment session proceeds.Instrument preparation and Dynamic limits of stability (DLS) training:- The system was switched on after connecting the printer.- The height of visual feedback screen was adjusted according to patient’s height; the locking knob was tightened to secure the display in the desired position.- The foot position and angle for each patient were detected by using alphanumeric grid on foot platform where the patient was centered as foot angle between 35 and 40 degrees.- The support handle was held while pulling out on the support handle release pin. - The handle was maintained to the desired position and the pin was locked the support handle in place was selected.- Level eight was selected (the most stable level), and then dynamic limit of stability training mode was selected.- The patient was standing on both feet and grasps the balance system handrails while holding onto the rails. The patient was instructed to try to achieve a centered position on platform, (once platform was set to motion). This is accomplished by shifting the position of patient’s feet to a position which was easy to keep the cursor on visual feedback screen in the center of the blinking center box, (16 boxes arranged around the center, the boxes at the top represent the anterior LOS, the boxes on the right and left of center represent medial and lateral LOS, while the boxes at bottom represent the posterior LOS).- Then the support handle was released gradually, the handle was held while pulling out on the support handle to release the pin. The handle was lowered and then the pin was released, and the patient was continued the training without support.- The training requires the patient to shift the center of gravity through weight shift to 16 targets positioned in ellipse.- The patients instructed to keep the cursor inside the central flashing box until it stopped flashing. Then patients asked to shift body weight to move the cursor over the second randomly appearing flashing box and keep the cursor inside it. The same process was repeated for each box till competed all boxes.- After centering the cursor at 16 squares, the platform was kept leveled beneath the patient’s feet while the patient was standing in a comfortable upright position.- Selected physical therapy program for diabetic peripheral neuropathy:1) Proprioception Exercises: Starting with static balance activities, progressing to dynamic balance activities, static balance activities was done by using the balance board while dynamic one done by walking on the floor according to Brooks. [9] protocol.All the proprioceptive exercises were performed for duration of 30 minutes with repetition ten times for every exercise for total 12 sessions, every other day. - Patients in both groups were standing on a level floor surface with one foot in front of the other, heel to toe with arms beside the body. - The patient was standing in this position for 30 seconds with his/her eyes opened then with eyes closed.- Balance board exercises: From standing position, each patient was instructed to move board forward, backward and from side to side using both feet. The previous exercises were repeated firstly with the eyes opened then with the eyes closed. Patient was standing on balance board firstly with support (hand rail) and then without support.- Walking on different surfaces: Walk in normal or heel-to-toe fashion over various surfaces; progress from hard, flat floor to uneven surface. Walking exercises were performed with eyes opened then eyes closed. Stair climbing up and down.- Rising up from a standard chair (four times) without arm support.2) Range of motion exercises (according to Goldsmith et al. [10] protocol):Active free range of motion exercises for ankle and subtalar joints were done. The patients were instructed to perform the exercises with repetition ten times for every movement. 1- Active dorsiflexion and plantar flexion of the metatarsophalangeal joints, holding each direction for ten sec.2- Active dorsiflexion and plantar flexion of the ankle joint, holding each direction for ten sec.3- Active supination and pronation of the subtalar joints, holding each direction for ten sec.3) Foot Care as a home program (advices):Patients were asked to follow these steps to take care of the feet that done every day (according to Timist et al. [11] protocol):Ÿ Clean feet daily, using warm not hot water and a soap. Dry the feet with a soft towel and carefully especially between toes.Ÿ Inspect feet and toes every day for cuts, blisters, redness, swelling, calluses, or other problems. Use a mirror on the floor at it works well for observation of planter aspect of foot, or get help from someone else if patient cannot see the bottoms of feet. Ÿ Moisturize feet with lotion but avoid getting the lotion between toes.Ÿ Each week or when needed, cut toenails to the shape of toes and file the edges with an emery board.Ÿ Always wear light tight shoes to protect feet from injuries. Prevent skin irritation by wearing thick, soft, seamless socks.Ÿ Wear rubber shoes material that fit well and allow toes to move. Break in new shoes gradually by first wearing them for only an hour at a time.Ÿ Before putting shoes on, look the shoes over carefully and feel the insides with hand to make sure that they had no tears, or objects inside that might injure feet.Statistical Analysis:The statistical methods for analysis of the results were used according to the following:- Data was summarized using range, mean and standard deviation for quantitative variables and frequency and percentage for qualitative ones.- Dependent (Paired) t-test was used to compare the difference within group, and unpaired t-test was used to compare the difference between two groups to compare between demographic data.- Comparisons between two groups were performed using mixed design (MANOVA) which was conducted to compare the plantar pressure at heel, big toe, and little toe for both sides (right, left) between the study group (A) and control group (B) in the “pre” and “post” tests.- P-values less than 0.05 were considered statistically significant and less than 0.01 were considered highly significant.- Statistical analysis was conducted using SPSS for windows, version 18 (SPSS, Inc., Chicago, IL).
3. Results
3.1. Comparison of Demographic Data for Patients in Both Groups (A&B)
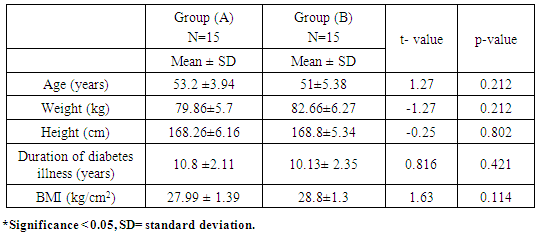
- Thirty diabetic patients (11 males and 19 females) with age ranged from 45 to 60 years participated in this study. The patients were randomly assigned into two equal groups; study group A (GA) and control group B (GB). (GA) consisted of (6 males and 9 females) with mean of age, weight, height, duration of diabetes illness, and BMI (53.2 ± 3.94 years, 79.86 ± 5.7kg, 168.26 ± 6.16 cm, 10.8 ±2.11years, and 27.99 ± 1.39kg/cm2) respectively. (GB) consisted of (5 male and 10 female) with mean of age, weight, height, duration of diabetes illness, and BMI (51 ± 5.38 years, 82.66 ± 6.27kg, 168.8 ± 5.34 cm, 10.13± 2.35 years, and 28.8±1.3kg/cm2) respectively. The duration of diabetes illness ranged from seven to fifteen years. Both groups were matched for age, weight, height, duration of diabetes illness, and BMI (Table 1).
|
3.2. Comparisons of Peak Plantar Pressure at Right and Left Heel
- Within each group:In Group A the mean values of plantar pressure at right and left heel in the "pre" and "post" tests were (13 ± 2, 12.2 ± 1.09) and (15.6 ± 1.81, 14.8 ± 1.92) respectively. This indicates a significant increase of plantar pressure at right and left heel post treatment with P-value =0.000*, 0.000* respectively. While in group B, where the mean of plantar pressure at right and left heel value in the "pre" and "post" tests were (11.41 ± 1.78, 11.66 ± 1.77) and (11.41 ± 1.67, 11.91 ± 2.15) respectively in the control (GB). This indicates no significant difference of plantar pressure at right and left heel post treatment with P-value=1.00, 0.37 respectively (Figure 1).
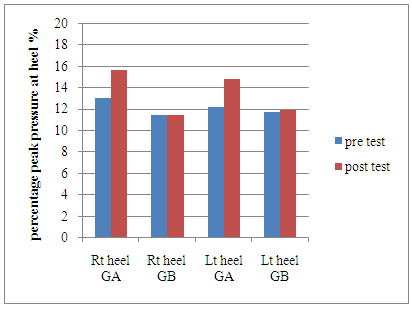 | Figure 1. Mean values of plantar pressure at right and left heel pre and post treatment in both groups (A&B) |
3.3. Comparisons of Peak Plantar Pressure at Right and Left Big Toe
- Within each group:In group A: the mean values of plantar pressure at right and left big toe in the "pre" and "post" tests were (6.6 ± 1.81, 5.8 ± 1.3) and (3.8 ± 1.48, 3.2 ± 1.09) respectively. This indicates a significant reduction of plantar pressure at right and left big toe post treatment with P-value =0.000*, 0.000* respectively.While in group B, the mean of plantar pressure at right and left big toe value in the "pre" and "post" tests were (6.91± 1.62, 5.83± 1.26) and (6.75 ± 1.6, 5.66 ± 1.23) respectively in the control group (B). This indicates no significant difference of plantar pressure at right and left big toe post treatment with P-value=0.30, 0.32 respectively (Figure 2).
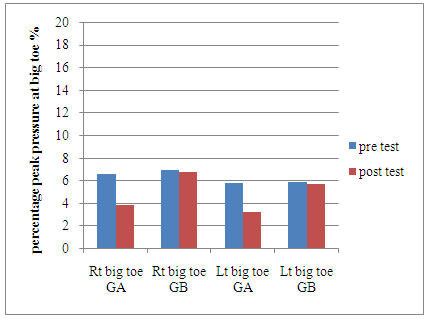 | Figure 2. Mean values of plantar pressure at right and left big toe pre and post treatment in both groups (A&B) |
3.4. Comparisons of Peak Plantar Pressures at Right and Left Little Toe
- Within each group:In group A: the mean values of plantar pressure at right and left little toe in the "pre" and "post" tests were (4.2± 1.3, 4.4± 1.24) and (3.4 ± 0.54, 3.6 ± 0.64) respectively. This indicates no significant differences of plantar pressure at right little toe post treatment with P-value =0.17, 0.12 respectively.Also in group B, the mean of plantar pressure at right and left little toe value in the "pre" and "post" tests were (4.83± 1.02, 4.33± 1.49) and (4.33 ± 1.23, 3.53 ± 1.19) respectively. This indicates no significant difference of plantar pressure at right little toe post treatment with P-value=0.18, 0.16) respectively (Figure 3).
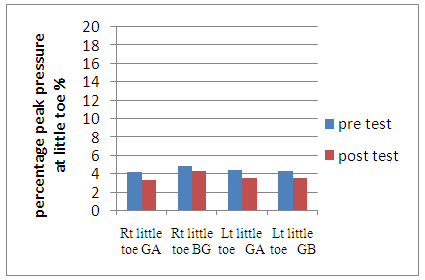 | Figure 3. Mean values of plantar pressure at right and left little toe pre and post treatment in both groups (A&B) |
3.5. Comparisons of F/R Ratio at Right Foot and Left Foot
- This ratio was calculated as the following: Forefoot planter pressure (pressure under big toe + pressure under little toe) divided by Rear foot planter pressure (pressure under the heel).Within each group:In group A: The mean values of F/R ratio for right and left side in the "pre" and "post" tests were (0.8 ± 0.22, 0.98 ± 0.30) and (0.47± 0.16, 0.6 ± 0.19) respectively. This indicates a significance reduction of F/R ratio for right and left side post treatment with P-value =0.000*, 0.000* respectively.While in the group B, where the mean of F/R ratio for right and left side value in the "pre" and "post" tests were (0.96± 0.12, 0.91± 0.16) and (0.90 ± 0.09, 0.87 ± 0.14) respectively in the control (GB). This indicates no significant difference of F/R ratio for right and left side post treatment with P-value=0.084, 0.315 respectively (Figure 4).
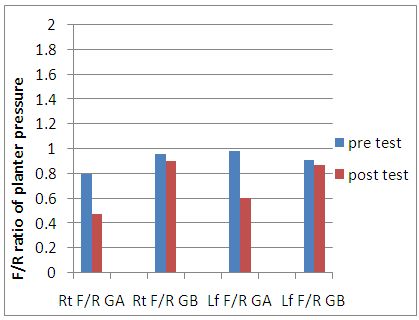 | Figure 4. Mean values of F/R ratio of planter pressure for right and left side pre and post treatment in both groups (A&B) |
4. Discussion
- The results of the current study revealed that, in the study group (A) there was a significant increase of plantar pressure at right and left heel, while there was a significant decrease of plantar pressure at right and left big toe and no significant differences of plantar pressure at right little toe post treatment. For the control group (B) there was no significant difference of plantar pressure at right and left heel, big toe and little toe post treatment.These results come in agreement with Rossi et al. [12] who reported that training on movable board in front of mirror is associated with improved postural control which can lead to a greater reduction of postural sway during training and thus a decrease of forefoot planter pressure.These results are supported by Salsabili et al. [13] who found that effective balance training by Biodex Balance System improves postural instabilities of patients with DPN by placing more emphasis on somatosensory information in balance training. Moreover, De León et al. [14] performed a study to determine the effect of biofeedback on foot pressure in DM patients with PN. The results showed that there was a significant improvement in the distribution of planter pressure at the end of walking training by using biofeedback with safe and regular plantar pressure redistribution without inducing any new area at risk under both feet.Also, Yu et al, [15] mentioned that peak pressures in the hallux and second to fifth metatarsal heads were not significantly changed in patients with or without diabetic claw or hammer toe deformities after balance training, but the hind foot peak planter pressure was significantly changed only after balance training. The results indicated that forward posture sway in patients with DPN especially with claw toe deformity increased forefoot plantar pressure to abnormally high levels so balance training has effect only at the heel. The authors concluded that planter pressure is regularly monitored in patients with diabetic foot with or without toe deformities might be detected earlier in order to prevent complications.Nicolas et al. [16] suggested the introduction of an original biofeedback system for improving balance control. The progression aimed at providing additional sensory information related to planter pressure distribution to the DPN patients through a tongue placed tactile output device to improve postural control during quiet standing. Visual feedback has an effect on the balance impairment in patients with PN as a result of type I DM. This was documented by Muhammad, [17] by using electrical balance board connected with computer as its screen acts as visual feedback. Vision act a direct role in stabilizing the balance by continually providing the nervous system with updated information about the position and movement of body segments in relation to each other and in relation to the environment. When patients stand with closed eyes, the posture sway will increase between 20% to 70%. This study also found that moving visual field can induce a powerful sense of self motion and misguiding visual cues induce significant increase in posture sway.Concerning redistribution of abnormal plantar pressure, the results of this study were disagree with the results of Goldsmith et al. [18] who found that high plantar pressures have been related to diabetic neuropathic ulceration that may be reduced by physical therapy training for eight weeks in the form of range of motion exercise in addition to balance training program for 20 patients with DPN aiming to reduce peak plantar pressures (PPP) and improve function as well as patient's quality of life.Jon et al. [19] also found that balance training and improvement of trunk control by using balance board exercises in the form of forward, backward and side to side trunk movement had an effect on the distribution of planter pressure. The authors conducted the study on 45 DPN patients for 12 weeks aiming to reduce the plantar pressure at fore foot during walking.Moreover Brooks, [9] found that there was a significant improvement of ankle ROM at the end of balance treatment in the form of proprioception exercise for three months in the DPN patients. This indicated that the application of balance training was effective in increasing the ROM which led to redistribution of abnormal foot pressure.The results of the current study also disagree with the findings of Santos et al. [20] who found that the proprioceptive training in diabetic women was effective in increasing the plantar tactile sensitivity. Balance program was effective in reducing the amplitude of antero-posterior oscillation of the center of pressure in the bipedal position with eyes open after 12 weeks of training.In the present study, no statistical significant difference was detected in plantar pressure at little toe in both groups. These results agree with the results of Cailli, [21] who carried out a study to assess patterns of plantar pressure occurring during the stance phase of gait in healthy subjects. At initial loading, the amounts of PPP were 70-100% of the body weight at the posterolateral aspect of the foot occurring within 0.05 seconds. In midstance, the weight bearing of the heel reduces one third, and weight bearing increases more distally toward the metatarsal heads. When body moves to push off phase, the weight bearing on big toe increased, usually the amount of PPP was 80% of the body weight on first metatarsal head. Under the toes, the hallux sustains the greatest pressure, while the fifth is the least, because center of gravity (COG) more closely to big toe while COG is far away from a little toe.The results of the current study revealed a significant reduction of F/ R ratio of planter pressure for both sides in the study group (A). These results come in agreement with the results of Caselli et al. [22] who performed a study to detect the effect of molded insole to reduce F/R ratio. The forefoot pressure was increased in the diabetic neuropathic foot, while rearfoot pressure was decreased and the (forefoot/rearfoot ratio) F/R ratio was increased which indicate an imbalance in the distribution of pressure with increasing degrees of neuropathy and may play an important role in the etiology of diabetic foot ulceration. So effective treatment by using molded insole for DPN patients showed reduction in forefoot pressure and increasing in rearfoot pressure, that lead to reduction of F/R ratio aiming to prevent forefoot ulceration.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML