-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2017; 6(1): 1-6
doi:10.5923/j.diabetes.20170601.01

Use of Electronic Instruments for the Opportunistic Screening of Undiagnosed Diabetes and Other Disorders of Glucose Metabolism. The Diabetes Screening Palermo Study “D.S.P.S.”
Tindaro Iraci, Vittorio Di Carlo, Francesco Magliozzo, Luigi Galvano
Italian Society of Family Doctors, Palermo
Correspondence to: Tindaro Iraci, Italian Society of Family Doctors, Palermo.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction: The Diabetes Screening Palermo Study evaluated, in the general practice setting, the effectiveness of a screening strategy for type 2 diabetes mellitus (T2DM). This study used electronic instruments to identify individuals at a high risk of diabetes and to provide early detection of undiagnosed T2DM and prediabetes. Methods and results: This is an observational study in primary care from Italy. The screening programme was divided into two phases. Phase 1: identification of patients at high risk of diabetes through the analysis of databases of general practitioners. Phase 2: screening to test for diabetes or prediabetes using fasting plasma glucose (FPG) and the 2-h plasma glucose value after a 75-g oral glucose tolerance test (OGTT). The OGTT was a central component of the screening programme and a significant proportion of individuals at high risk for diabetes, which is defined as those with impaired fasting glucose (IFG), had blood glucose levels, after the glucose load that either were compatible with a diagnosis of T2DM or impaired glucose tolerance (IGT). Resultsafter 24 months of the study: the total study was composed of 26 410 subjects, of which 13 319 (50.43%) were at high risk of T2DM. 8174 subjects, representing the 61,37% of those at high-risk, had at least one measurement of fasting plasma glucose (FPG). A total of 5428 subjects equal to 66,41% of those with at least one measurement of fasting blood glucose and equal to 40.75% of all high-risk subjects, had impaired fasting glucose (IFG) A sample of 965 subjects with IFG, were then subjected, at random, to an OGTT, on the basis of which 136 subjects (14.09%) were identified with IGT and 83 subjects (8.60%) gave a response compatible with the diagnosis of T2DM. Conclusion: In a primary care setting, a proactive approach towards diabetes screening, especially performing OGTT in subjects with IFG, facilitated the early diagnosis of T2DM. This reduced the percentage of cases of undiagnosed diabetes and allowed the identification of individuals with prediabetes who required preventive interventions. Through a process of clinical audit, the computerised systems, facilitated the identification of people at high risk for diabetes and led to better management of the screening programme.
Keywords: Diabetes screening, People at high risk of diabetes, Disorders of glucose metabolism, Oral glucose Tolerance Test (OGTT), Computerised systems
Cite this paper: Tindaro Iraci, Vittorio Di Carlo, Francesco Magliozzo, Luigi Galvano, Use of Electronic Instruments for the Opportunistic Screening of Undiagnosed Diabetes and Other Disorders of Glucose Metabolism. The Diabetes Screening Palermo Study “D.S.P.S.”, International Journal of Diabetes Research, Vol. 6 No. 1, 2017, pp. 1-6. doi: 10.5923/j.diabetes.20170601.01.
1. Introduction
- Type 2 diabetes (T2DM) is a chronic disease with a high prevalence and constant growth. Data from the eighth report of the Health Search from the Research Institute of the Italian Society of General Practitioners (SIMG) in 2013-2014 [1] showed a trend of increasing prevalence from 5.9% in 2005 to 7.7% in 2013. The prevalence grows with age; one in five people above 75 years of age suffers from diabetes. The prevalence of diabetes is also higher in obese and overweight individuals, as well as those who are not physically active [2]. Data from the literature also shows that in 30-50% of cases, diabetes is not diagnosed [3] and that the diagnosis of diabetes is often delayed. An early diagnosis would allow for therapeutic intervention with positive results in terms of the prevention of long-term complications [4, 5].It is widely accepted that the clinical diagnosis of T2DM is preceded by a long asymptomatic phase during which the disease can only be diagnosed if actively detected through screening procedures.The screening programme should be directed at the population at high risk of diabetes (selective screening) and performed during a medical check-up (opportunistic screening) [3]. Testing should be carried out, within a health care setting. Community testing outside a health care setting is not recommended because people with positive tests may not seek or have access to appropriate follow-up testing and care. Community testing may also be poorly targeted, i.e., it may fail to reach the groups most at risk and inappropriately test those at very low risk or even those who have already been diagnosed [6].The screening programme also allows the detection of other disorders of glucose metabolism, such as impaired fasting glucose (IFG) and impaired glucose tolerance (IGT) [7], all of which predict the future development of the disease and therefore require appropriate preventive interventions that are based primarily on lifestyle changes. The effects of lifestyle interventions to prevent or delay progression to diabetes were consistent across a substantive body of literature [8, 9].Primary care is widely considered the prime setting to implement opportunistic screening programmes for early detection of T2DM and prediabetes.Currently, the general practitioners (GPs) use computer systems to allow them to identify people at high risk of diabetes easily and to manage the entire screening programme proactively.Within the context of the SIMG of Palermo, a study (Diabetes Screening Palermo) has been designed to evaluate the effectiveness of a screening strategy, which uses electronic instruments to allow easy identification of people at high risk for diabetes and to provide early diagnosis of T2DM and prediabetes.
2. Methods
- Twenty GPs of SIMG conducted an observational study, between September 2013 and August 2015, in the Italian region of Sicily in the Province of Palermo. The study participants were drawn from the general patient population of these physicians. Included were men and women, aged > 14 years, after the exclusion of individuals previously diagnosed with diabetes.The screening programme was carried out in two phases:1st phase: identification of people at high risk for diabetes through the analysis of databases of the general practitioners.2nd phase: screening for early diagnosis of T2DM and other disorders of glucose metabolism (IFG, IGT).To identify those at high risk for T2DM, the criteria adopted was from the Italian Standard of Medical Care in Diabetes 2014 (3). Adults, of any age, who were obese or overweight (BMI ≥25 kg/m2) and who had one or more additional risk factors for diabetes, were considered as being at high risk for diabetes (Table 1). For all patients, without these risk factors, testing began at age 45.
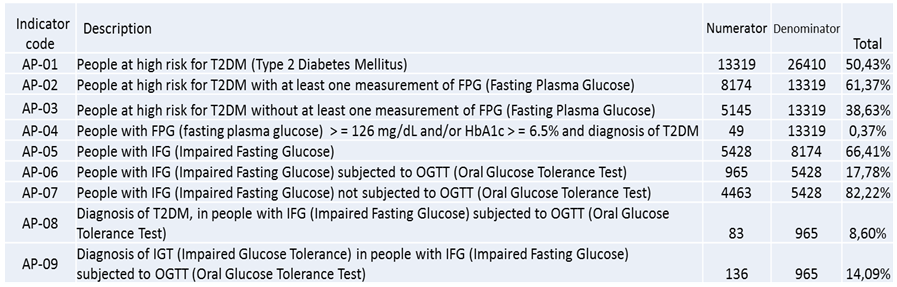 | Table 1. Values of the main indicators, after 24 months of the DSP Study |
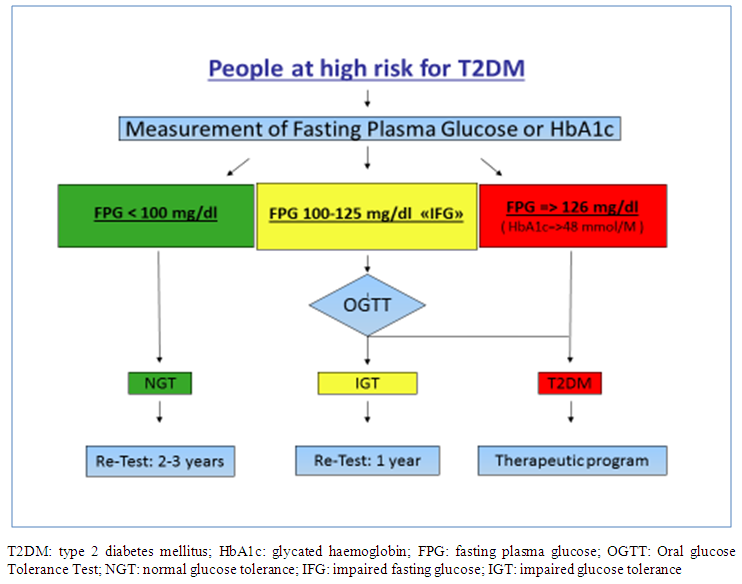 | Figure 1. Screening procedure and the follow up of the subjects at high risk for T2DM |
3. Results
- Table 1 shows the numerical values of the nine core indicators, after 24 months of the study.The study was composed of 26 410 subjects, of which 13 319 (50.43%) were at high risk for T2DM. A total of 8174 subjects, representing the 61,37% of those at high-risk, had at least one measurement of fasting plasma glucose (FPG). A total of 5428 subjects equal to 66,41% of those with at least one measurement of fasting blood glucose and equal to 40.75% of all high-risk subjects, had impaired fasting glucose (IFG) (Fig 2).
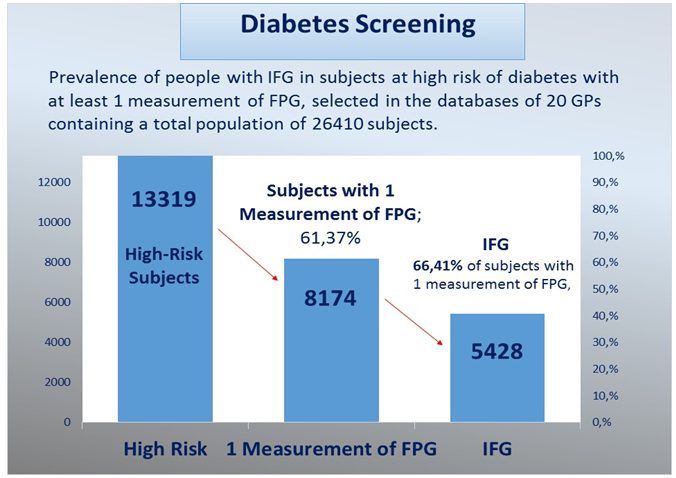 | Figure 2. Prevalence of IFG in the population at high risk for T2DM selected in the database of 20 GPs, containing a total population of 26 410 subjects, in the DSP Study |
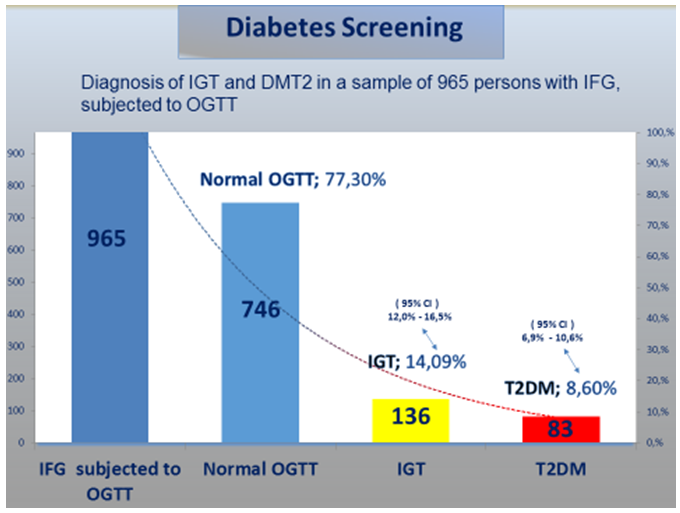 | Figure 3. Diagnosis of IGT and DMT2 in a sample of 965 individuals with IFG, subjected to an OGTT. The percentages of IGT and T2DM were calculated with a confidence interval of 95% |
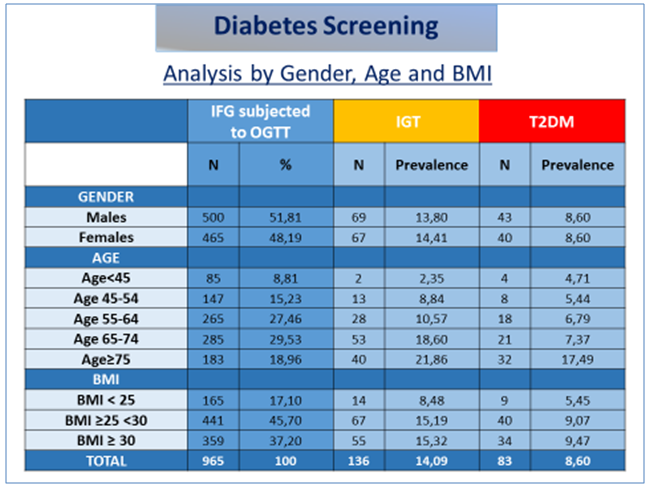 | Table 2. Analysis by gender, age and BMI in subjects with IGT or T2DM diagnosed based on an OGTT in the DSP Study |
4. Discussion
- Facilities for Diabetes diagnosis and management should be available in primary health-care settings, with an established referral and back-referral system.The use of electronic databases to identify subjects at high risk of diabetes has resulted in the development of algorithm/prediction models in several countries. The main goal of these studies is, in general, to define patients' characteristics associated with a higher probability of having diabetes, i.e. patients for whom performing a blood test is justified. The Diabetes Screening Palermo Study, confirmed that, through a process of clinical audit, the computerised systems, used by GPs, facilitated the identification of people at high risk for diabetes and moreover improved the management of the screening programme. These computer systems used a panel of indicators that allowed the monitoring of clinical activity and highlighted any clinical or managerial problems, thereby allowing the physician to make the necessary corrections and to lead the screening programme with a proactive approach.Primary care remains the most favourable setting for an early diagnosis of diabetes. A systematic and proactive approach towards diabetes screening, especially by performing OGTT in subjects with IFG, facilitated, in the Diabetes Screening Palermo Study, the early diagnosis of T2DM. The prevalence of 8.60% of subjects with T2DM diagnosed based on an OGTT could be extended to all subjects with IFG identified in the study, using the OGTT. Similarly, If this screening model was applied through a joint action of the Italian regions or European countries, the result would be a global reduction of undiagnosed diabetes and the identification of a large population of patients with prediabetes (IFG or IGT), requiring preventive interventions based primarily on lifestyle changes [22-24].GPs partecipating in the study: Tindaro Iraci, Salvatore Campo, Girolamo Consiglio, Rosario D’Alessandro, Vittorio Di Carlo, Baldassare Di Silvestre, Serenella Fasulo, Luigi Galvano, Francesco Paolo Lombardo, Francesco magliozzo, Giuseppa Mazzola, Vincenzo Mazzola, Giovanni Merlino, Umberto Pozzecco, Francesco Salamone, Salvatore Sardo, Pasquale Severino, Maria Teresa Simoneti, Rita Zafonte.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML