-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2015; 4(2): 38-42
doi:10.5923/j.diabetes.20150402.03
Lipohypertrophy - The Neglected Area of Concern in the much Talked about Diabetes
Salahuddin Farooq Mohammed1, Muktar Sano Kedir2, Tarekegn Tesfaye Maru3
1Associate Professor of Pharmacology, Department of Pharmacy, College of Health Sciences, Mizan Tepi University, Mizan Teferi, Ethiopia
2Lecturer of Clinical Pharmacy, Department of Pharmacy, College of Health Sciences, Mizan Tepi University, Mizan Teferi, Ethiopia
3Lecturerof Pharmacology, Department of Pharmacy, College of Health Sciences, Mizan Tepi University, Mizan Teferi, Ethiopia
Correspondence to: Salahuddin Farooq Mohammed, Associate Professor of Pharmacology, Department of Pharmacy, College of Health Sciences, Mizan Tepi University, Mizan Teferi, Ethiopia.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Insulin injectable therapy is an easy process and so the side effect of injecting insulin in the same area of the body again and again leads to development of a thicker subcutaneous adipose tissue which is not a pleasant outcome. This thickening of the subcutaneous adipose tissue at the injection sites is defined as lipohypertrophy. This effect is evident enough to catch the eye of healthcare workers, doctors and patients themselves yet it remains to be the most neglected area of concern. Dedicated health professionals leave no stone unturned in creating awareness about diabetes and its complication yet the most commonly used insulin therapy by injections and its adherence have somehow been deserted due to ”assumed fact that this type of injectable therapy is being used correctly and efficiently”. Healthcare practitioners and providers need to re-educated and patients need to be educated on the safe techniques of insulin injection to allow a uniform absorption of insulin and thus this article is aimed at emphasizing the need of awareness towards the areas to be used for insulin injections, correct injection techniques and proper health care.
Keywords: Lipohypertrophy, Diabetes Mellitus, Site rotation, Insulin
Cite this paper: Salahuddin Farooq Mohammed, Muktar Sano Kedir, Tarekegn Tesfaye Maru, Lipohypertrophy - The Neglected Area of Concern in the much Talked about Diabetes, International Journal of Diabetes Research, Vol. 4 No. 2, 2015, pp. 38-42. doi: 10.5923/j.diabetes.20150402.03.
Article Outline
- The objective of this paper is to instruct diabetics on the injection technique:1) Educating diabetic patients with the correct injection technique including the right injection, the correct area to be injected and caring of these injected areas. 2) Educating diabetic patients as to how insulin acts, overcoming anxiety towards injections and employing the correct practice.
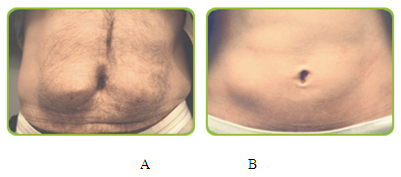 | Figure 1. A: Abdominal picture of Lipohypertrophic patient; B: Abdominal picture of normal patient. myclickfine.com image c 2015 |
1. Treatment of Diabetes Mellitus
- Having diabetes means making permanent lifestyle changes which include treatments either with insulin or oral hypoglycaemic agents, exercise and a healthy diet. Diabetic patients are personally responsible for maintaining good metabolism and they continuously have to monitor and adjust the elements of their treatment. In everyday life, multiple (3 to 5 injection daily) insulin injections may seem to be a flexible treatment option but self-care and blood glucose measurements are still a concern. With the advent of new and superior insulin devices, new skills needed to handle these devices and both the diabetic patient and healthcare professional need to be updated. Hence aside from diet, exercise and the medical treatments, awareness on the right type of technique involved in insulin injections and the ease of reducing diabetic complications by implying site rotations would help reduce the aftermaths of diabetes.
2. Insulin Treatment
- In diabetic patients, the role of insulin treatments is to prevent hyperglycaemia and also to prevent the risk of developing late diabetic complication. Earlier, insulin was extracted from bovine and porcine pancreatic tissue but today, modified yeast and bacteria are used to produce human insulin using DNA recombination technology. This new technique develops variations on biosynthetic insulin analogues thus allowing a more physiological approach to insulin management. Analogues of biosynthetic insulin have an increased half-life thus providing a long lasting effect with effective profiles and they are made up of monomer or dimer molecules of insulin resulting in rapid uptake from injection sites [1].Types of insulins available in the market: • Extra-rapid acting insulin injectable (NovoRapid, Apidra, Humalog) is taken immediately before a meal and the effects starts approximately after 15 minutes reaching its maximum after 1 to 3 hours. After 3 to 5 hours the effect ceases. This injectable has a shorter duration of action than the soluble human rapid acting insulin analogue. • Soluble insulin/Rapid-acting insulin analogue (Insuman Rapid, Actrapid) is injected about 30 minutes before a meal and it reaches maximum effect within 1 to 3 hours with action duration lasting 6 to 8 hours. • Intermediate-acting insulin analogue (Insulatard, Humulin NPH, Insuman Basal) has action duration that lasts for 24 hours with the maximum effects after 4 to 12 hours. This intermediate-acting insulin analogue is a pen with a glass sphere. The solution in the pen is mixed by moving the glass sphere back and forth at least 10 times until a uniform milky-white colour solution is formed [2].• Premixed insulin analogues consist of extra-rapid acting insulin or rapid-acting insulin which is produced in different concentrations (NovoMix 30, Humalog Mix 25, Mixtard 30, InsumanKomb 25). Premixed insulin should be mixed at least 10 times forward and back until a uniform solution of milky white has been formed [2]. When used for the first time NovoMix 30 must be rolled in a horizontal position. • Slow-acting insulin analogues (Lantus, Levemir) have longer action duration with straight profiles. This injectable reaches maximum effects in 60 minutes and lasts for 24 hours. No agitation is required before use.
3. Sites of Injection
- Injection site is an important issue in dealing with diabetes. Subcutaneous adipose tissue is said to most optimum for injecting insulin. Intramuscular injection of insulin makes it challenging to maintain a good glycaemic control thus it should be avoided. An international workshop held in 1998 on insulin injection technique concluded the same [3]. The preferred systemic blood uptake of insulin is through subcutaneous insulin injection and not by the portal blood system where naturally produced insulin is in use. Careful planning of insulin in accordance with food, exercise and insulin type should be done as insulin absorption rate is prolonged by the subcutaneous adipose tissue.
4. Factors Affecting Absorption of Insulin from Subcutaneous Adipose Tissue
- Varying blood glucose concentrations throughout the day is partly due to the fact that absorption of intermediate-acting insulin in individual patients is an average of 25% in the day to day variation [4]. In individual patients, difference in absorption up to 35% has been established [5]. Insulin uptake is affected by the volume and concentration of insulin. Higher the concentration and volume of insulin, the more delayed the absorption. Bovine and porcine insulin is taken up slower than human insulin [6]. The rate of insulin uptake is not affected if the insulin is injected either at the top or bottom layer of subcutaneous adipose tissue [7, 8]. According to a Danish study conducted in 1998, insulin dose should be divided in case of doses over 40 IU. A risk of hypoglycaemia develops when the muscle close to insulin depot is exercised as the rate of insulin absorption in that area increases. Muscle exercises can increase blood flow up to 237 times compared to resting stage and this has an intense effect on insulin uptake [9]. Absorption rates are also increased by high body temperature and by massaging the injection site. Smoking causes insulin to be absorbed slowly [6, 10]. For a more uniform insulin uptake the insulin should be injected in the subcutaneous adipose tissue and this can be achieved by choosing the accurate needle length. Chiefalterations in uptake of insulin can occur if the insulin is injected in the muscle tissue [6, 10]. Anatomical area in the subcutaneous adipose tissue is also of importance with regards to insulin uptake. Insulin absorption is slowest from thigh and hip and fastest from abdomen and upper arm. Patients are not encouraged to change site of injection day to day due to the variations in insulin uptake [6]. Apart from anatomical area, the thickness of the tissue also varies from person to person and injection site to injection site. In the same person, the thickness of the subcutaneous adipose tissue in the thigh varies from area to area [6, 8]. Intermediate-acting insulin analogues have higher insulin uptake than extra-rapid-acting insulin analogues [1].
5. Threats Linked with Intramuscular Insulin Injection
- In recent years, radiological methods have confirmed the risks involved in injecting insulin intramuscularly. Frid and Lindén measured the thickness of subcutaneous adipose tissue injection sites in 91 normal weight diabetic patients using computer topography and results showed that intramuscular insulin injections in the upper arm is not recommended due to the high risk involved. The subcutaneous adipose tissue was 15.1 and 12.2 mm respectively in women and men indicating that finding skin fold in the upper arm is difficult and therefore a 12.5 mm needle is not recommended [8]. Thow and colleagues confirmed the same in their study [11].
6. Adherence
- Following the doctor’s instruction and understanding the treatments recommended is key to adherence and addressing the disease. Patients show more compliance towards following medication or treatments recommended after having a satisfied consultation cum communication with the doctor. In a study conducted in 1984, 53% patients adhered to the treatments following a good communication/ consultation with the doctor [11]. Studies conducted in recent years have revealed that following lifestyle changes recommended seem to be a problem but it’s important that patients need to maintain a good glycaemic control in order to delay the incidence of diabetic complication which may appear in later in life. For diabetic patients no education is less to emphasize the need of being in control and to do the needful. Support from the groups and families become an integral part of their system and helps diabetic patients to adhere to the treatments. Before the actual treatment of diabetes begins, the patient is traumatized by the fact that he/she has acquired the chronic disease. The phobia of needles and the constant need to remember the doses of drugs settles in later. But for some, the fact they have diabetes does not matter much than the use of needles for treatment. Diglas and colleagues conducted a study, in 1999, to investigate the reaction of patients towards diabetes and insulin treatment and results reported that 45.8% patients had needle phobia [13]. With this fact in hand it’s not hard to imagine that patients who have to inject themselves on a daily basis will have trouble maintaining good glycaemic levels. Anxiety pertaining to needles in adults and children is linked with poor metabolism [14].
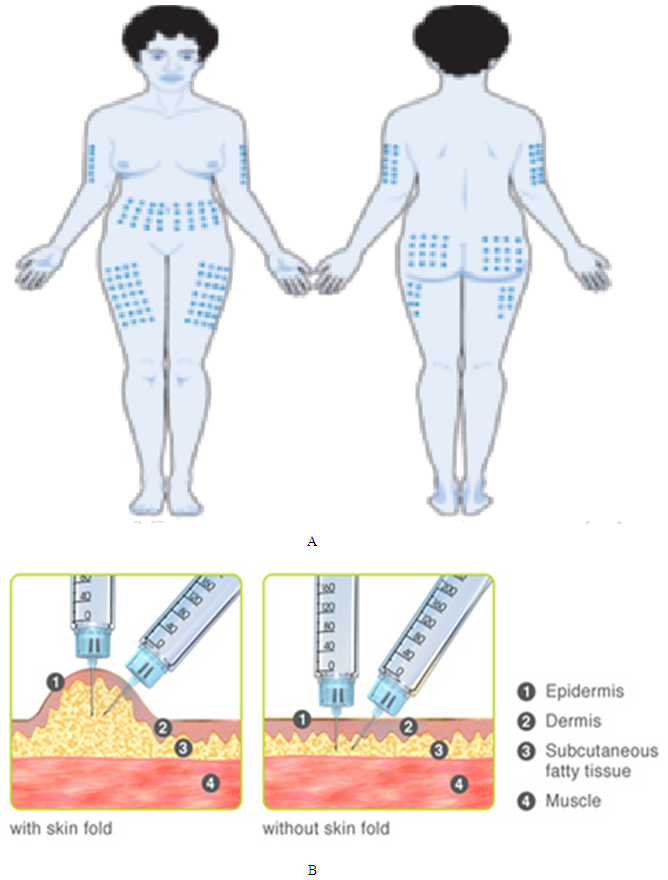
7. Human Body Parts which can be Used for Insulin Injection
- Different blood flow, number of capillaries and permeability of blood capillaries are presumed to be the reasons that affect absorption rates across the same area in the body. Studies have shown that abdomen absorbs rapid-acting insulin 30% and 86% faster from the arm and the femur, respectively. The upper arm absorbs insulin approximately 40% faster than the thigh [15]. The above mentioned study also highlights and emphasizes the aim of this review, that injection sites should be changed with in the same anatomical area and not shifted across different body parts. This point was confirmed in 1984 by Binder and colleagues [5].
8. Uptake of Insulin from Different Parts of the Body
- From the subcutaneous adipose tissue of the femur, rapid-acting insulin is absorbed very slowly with only approximately 50% being absorbed after 5 hours [16, 17]. Compared to the abdomen on a day to day disparity, intermediate-acting insulin is taken up slowly from the thigh. To create a more safe and stable insulin profile at night, it’s crucial that intermediate-acting insulin be injected at bedtime (10:00- 11:00 PM). Hence, insulin injections in the thigh at bedtime ensure a uniform absorption thus decreasing the risk of hypoglycaemia at night and hyperglycaemia before breakfast [18]. The hip can be the best alternate subcutaneous injection site for intermediate- and slow-acting insulin as its insulin absorption rate is equal to the thigh [5]. Relatively, the hip is safer for intramuscular insulin injection than the thigh, but in common practise, the thigh is most often used for insulin injection. This is due to the fact that many patients find it difficult to inject themselves in the hip. In the upper arm, the minimal distance of the skin from the muscle makes it unsafe for insulin injections [8, 11]. But in case the upper arm is to be used anyway, injecting insulin into a lifted skin fold is the recommended way.
9. Rotation of Insulin Injection Sites in the Same Anatomical Area to Prevent Lipohypertrophy
- Among each injection site, a 3cm distance is recommended when injecting insulin in the same anatomical area [19]. Results from a study conducted by Saez-de Ibarra & Gallego, showed that women with higher BMI had the highest incidence of lipohypertrophy as the injections were not correctly distributed with in the same area [20]. Many practitioners recommend using the abdominal area because absorption from this site is least affected by exercise and is the most convenient. However, repetitive use of the same injection site might result in lipohypertrophy, and it does harden the skin, making needle penetration tricky. Furthermore, insulin absorption from lipohypertrophic sites can be slow.
10. Lifted Skin-Fold Injection Method
- The risk of an intramuscular injection can be overcome by creating a skin-fold i.e; to pinch the skin and form a ridge or fold between two fingers, preferable the thumb and index finger, which raises the subcutaneous adipose tissue layer [21]. The skin-fold should be raised through out the delivery of the injection and remain in position for another 5 to 10 second after the injection and before the needle is withdrawn [3]. However, if the length of the needle is greater than the distance of skin to muscle, the skin-fold insulin injection method need not be followed [8]. In 1992, Thow and colleagues showed through ultrasound scanning that except for lean adults (BMI <24.6) everyone else can inject insulin in the upper lateral quadrant of the hip without a skin-fold [11]. In a study conducted in 2000, by Solvig and colleagues, the results showed that overweight diabetic patients injected insulin subcutaneously while the normal weight patients injected insulin into the muscle. Both set of patients had used a 6mm needle and injected insulin without the skin-fold. This study showed that the safe and best way to inject insulin with a 6 mm needle is to create a skin-fold at a 90 degree angle. For a 12 mm needle, lifting the skin-fold upto an angle of 40-60 degree was preferable [22].
11. Conclusions
- Lipohypertrophy is difficult to recognize in the initial stages and only when hyperglycaemia has occurred, we reason that insulin is not getting absorbed by the body and begin to address the situation. This should not be the case anymore. Now that we have understood the importance of site rotations and emphasized the importance of subcutaneous insulin injections, patients suffering from need to be educated on the correct way of injecting insulin and correct method of site rotation. Doctors and healthcare workers associated with diabetes patients need to spread more awareness with regards to lipohypertrophy. Patients dependent on insulin injections need to be educated on the correct insulin injection techniquesas it is crucial to maintaining a good diabetes profile.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML