-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2015; 4(1): 1-6
doi:10.5923/j.diabetes.20150401.01
Risk Factors for the Development of Diabetic Foot Ulcers in Gaza Strip: A Case-Control Study
Hassan Ata Abu Obaid1, Ashraf Eljedi2
1Ministry of Health, Gaza Strip, Palestine
2Faculty of Nursing, Islamic University of Gaza, Gaza Strip, Palestine
Correspondence to: Ashraf Eljedi, Faculty of Nursing, Islamic University of Gaza, Gaza Strip, Palestine.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
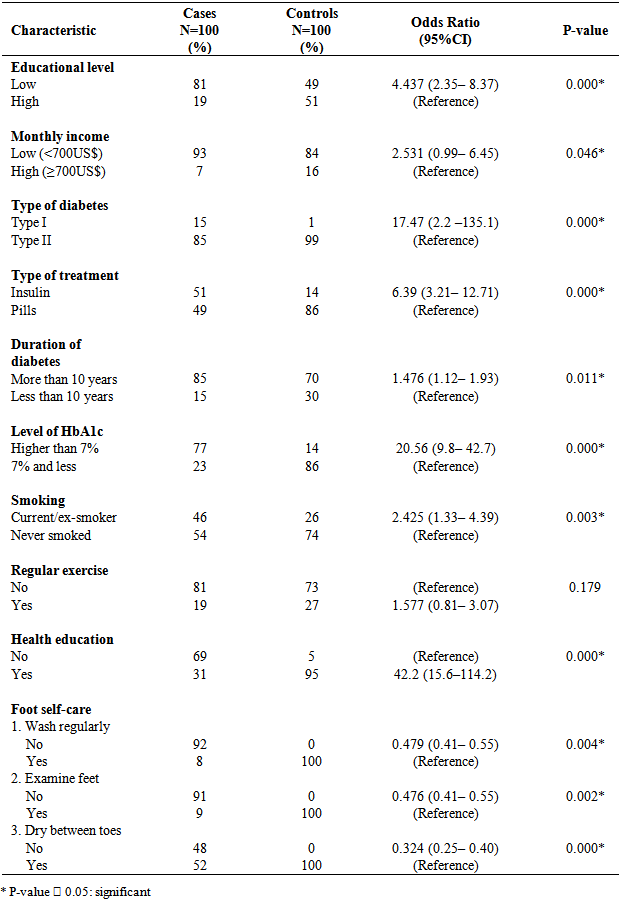
Background: Diabetic foot ulcers are significant health and socioeconomic problems, having negative effects on the quality of life and imposing a heavy economic burden on the patients and the community. Aims and Objectives: This study was conducted to identify the risk factors contributing to diabetic foot ulcers among diabetic patients in Gaza strip (Palestine). Materials and methods: Case-control, retrospective approach was used in this study, where 100 diabetic patients with foot ulcers and 100 controls (diabetic without foot ulcers) were selected from the surgical departments at the largest two governmental hospitals in Gaza. Both groups were matched for age and gender. By using questionnaire, the data were collected concerning main risk factors i.e. socio-demographic, lifestyle, and disease profile variables. Results: This study found several factors associated with higher incidence of diabetic foot ulcers including: low educational level (OR = 4.437; 95% CI: 2.351-8.374), low household income, type I diabetes, being on insulin treatment, longer duration of diabetes (more than 10 years), HbA1c ≥ 7% (OR=20.56; 95% CI: 9.89-42.76), being current smoker or ex-smoker, and lack of health education (OR = 42.29; 95% CI: 15.64–114.28). On the other hand, proper foot care activities [e.g., washing feet every day (OR= 0.479; p=0.004), examining feet regularly (OR = 0.476; p=0.002) and drying well between toes (OR = 0.324; p=0.000)] was a protective factor that decreases the chance of developing foot complications. Conclusions: Most of the identified risk factors were modifiable. Emphasis should be directed toward health education, changes in lifestyle, and following safety measures to decrease the higher incidence of diabetic foot complications in Gaza strip.
Keywords: Diabetes mellitus, Diabetic foot, Risk factor, Palestine
Cite this paper: Hassan Ata Abu Obaid, Ashraf Eljedi, Risk Factors for the Development of Diabetic Foot Ulcers in Gaza Strip: A Case-Control Study, International Journal of Diabetes Research, Vol. 4 No. 1, 2015, pp. 1-6. doi: 10.5923/j.diabetes.20150401.01.
Article Outline
1. Introduction
- Diabetic Foot Ulcers (DFUs) are a significant health and socioeconomic problems, having negative effects on the quality of life and imposing a heavy economic burden on the patient and the community; it can lead to long stay in hospital and the need for rehabilitative and home care services [1]. It is estimated that in 2012 approximately 370 million people have diabetes which accounts for 8.3% of the world’s population. Around 80% of these people live in developing countries. By 2030, the global estimate is expected to rise to over 552 million – 9.9 % of the adult population [2]. Every 20 seconds a lower limb is lost due to diabetes somewhere in the world [3]. Foot complications occur in both forms of diabetes and are related more to the duration of illness rather than to the age at onset of disease [4]. Diabetic patients have suffered from foot ulceration. Despite progress in the prevention treatment, and achieving the healing of established ulcers, Diabetic Foot Ulcer remains a considerable challenge [5]. The development of foot problems is not an expected consequence of having diabetes, indeed, most foot ulcers are preventable. However, a recent study indicated that foot ulcer recurrence is still an unresolved issue. Although several therapies have been described for preventing foot ulcers, the rates of reulcerations are very high [6].In Palestine, few studies indicated that the prevalence of DM in Palestine was 9.6% in females and 10.0% in males [7]. However, no or weak national data is available on the overall incidence and prevalence of DFUs and disabilities resulting from DM. There is neither effective surveillance system nor community–based screening program to detect the potential cases of DFUs among Palestinian people. The current system counts mainly the visits of the diabetic patients to primary health care centers and depends on mortality data to estimate the impacts of this disease. Thus, this study was the first one to fill this gap and to try to identify major risk factors contributing to diabetic foot ulcers among diabetic patients in Gaza strip (Palestine). We hope that the findings of this pioneer study in Gaza strip will contribute to setting priorities and establishing effective national preventive programs to decrease the incidence of DFUs and amputation rate among the diabetic clients in Palestine.
2. Materials and Methods
- We performed a retrospective case control study in surgical, medical and outpatient departments at the largest two governmental hospitals in Gaza strip namely, Al-Shifa Hospital and European Gaza Hospital (EGH) from May 2013 till April 2014. The study sample consisted of 200 participants; 100 diabetic patients with foot ulcers and other 100 controls (diabetic without foot ulcers). According to Epi Info program at 95% confidence interval and power 80%, an assumption risk was 20% among controls and 40% among cases; the sample size was 91 for case group and 91 for control group. The researcher decided to assign 100 patients in each group to avoid low response rate. The inclusion criteria for cases was: all diabetic patients, male or female, with non-traumatic foot ulcer resulted from the disease itself and admitted to either Al-Shifa Hospital or EGH; while for controls was: all diabetic patients, male or female without diabetic foot ulcers or who have foot ulcers resulted from trauma or incident. Both groups were matched for age and gender.
2.1. Data Collection
- The data were collected from both groups by answering the questionnaire of the study in face-to-face interviews. The interviews were held in Al-Shifa Hospital, and EGH. The questionnaire covered the following data: 1. Socio-demographic and economic data included gender, age, marital status, place of residency, educational level, occupation and income. 2. Clinical data included medical history, smoking status, physical activity, access to health care centers, history of foot problems, current foot or leg problems, information about foot care, safety and preventive measures and foot care education.
2.2. Ethical Approval
- The ethical and administrative considerations were taken. We obtained an ethical approval to perform the study from Helsinki Committee in Gaza. Administrative permissions were obtained from ministry of health and the two hospitals. Every participant in the study received a complete explanation about the purpose of the study and assurance about the confidentiality of the information. All subjects have agreed to participate in the study and signed a consent form. Time allocated for each interview was 15-20 minutes.
2.3. Data Analysis
- SPSS version 20 was used to analyze the data. Frequency, percentages and means were calculated for describing the socio-demographic and economic variables. Cross tabulation was conducted to determine the relationships between two variables or more. We used Chi squire, t- test, and ANOVA to test the significant differences in categorical and continuous variables of the socio-demographic characteristics between the cases and the controls. Binomial logistic regression was used to measure the strength of association between the incidence of diabetic foot ulcers and the risk factors (determinants) by calculating odds ratios (OR), with 95% confidence intervals (CI). If the CI did not include 1, the OR was considered significant. For all comparisons, we defined statistical significance as any P value less than 0.05.
3. Results
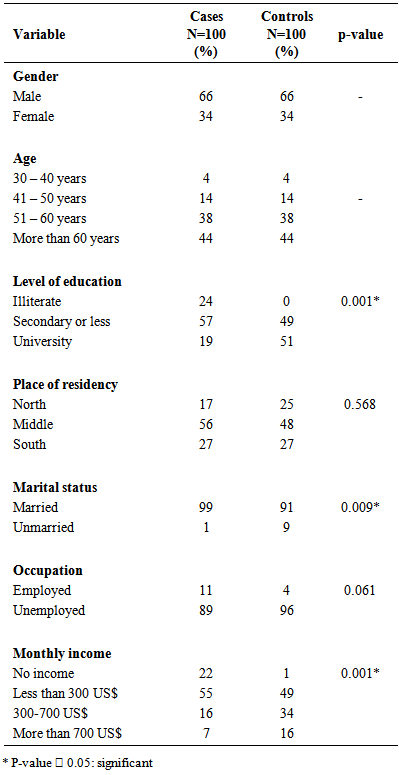
- The study sample consisted of 200 participants; 100 diabetic patients with foot ulcer and other 100 controls (diabetic without foot ulcers). Cases and controls were matched for age and gender. Table (1) shows that about 66% were males and 34% were females. Most of them were older than 50 years old with low educational level. Regarding the place of residency, 56% of the cases and 48% of the controls were from the middle area of Gaza strip which is mainly composed of refugee camps. This indicated that most of our participants were refugees living in poor and crowded refugee camps. This explains why the majority of them were not working and don't have sustainable sources of income. Table (1) also indicated that there were significant differences between cases and controls in regards to level of education, marital status and monthly income; while no significant differences were found in other socio demographic variables (occupation and place of residency).
|
|
4. Discussion
- In this study we examined the risk factors contributing to diabetic foot ulcers and their association with demographic and socio-economic variables in Gaza governorates. We found that higher incidence of diabetic foot was associated with low levels of education, low income, type I diabetes, use of insulin, longer duration of DM, HbA1c higher than 7%, smoking and lack of health education. Meanwhile, proper foot care was found to be a protective factor that decreases the chance of developing foot complications among diabetic patients. Our results are consistent with previous studies which found an association between DFUs and illiteracy [8, 9]. Another study indicated that incidence of DFU was positively influenced by education [10]. It is suggested that individuals with high level of education have better understanding of their disease, and are more aware of suspected complications that may occur. Moreover, recent statistical analysis proved that the educated group was significantly better in terms of foot care [11] and patients with higher education participated in foot self-care programs more than patients with lower levels of education [12]. Indeed, education is usually seen as the key to better health as it enhances individuals to better utilizing health information and treatment, and the less educated patients were also more likely to be seen as non-compliant by health professionals and used less hospital care. Several studies found an association between DFUs and low average monthly income [8,13-15]. Poor socioeconomic status determines the ability to obtain medication and services that improve health [8]. It is suggested that low income may restrict patients' ability to pay for treatment and consultation expenses, and in consequence may aggravate their health problems.We found that Type I diabetic patients on insulin treatment were at a greater risk for the development of foot ulcers as compared to those on diet and oral anti-diabetic medication. This result could be attributed to the fact that Type I DM usually affects people at early stages of life and it is difficult to be treated or controlled compared to Type II diabetes, and as a sequence, possibility of developing foot complications would be higher [16]. However, Type II diabetes if not controlled and managed well, may lead also to lower limb complications [9, 10]. Similar results concerning the longer duration of diabetes and development of DFUs were revealed by other researchers [9, 10, 17, 18] who reported that the long duration of DM (10–15 years) can lead to developing DFUs. Reports from Mayo Clinic [19] showed that the earlier you develop diabetes, and the less controlled your blood sugar, the higher the risk of complications. This study showed that elevated of level HbA1c increases the risk of diabetic foot. These results are supported by other studies [17, 20, 21] which indicated that the main characteristics associated with chronic non-healing DFUs is elevated HbA1c > 7%. In Saudi Arabia, a cross sectional study showed strong association between increase level of Hba1c ≥10 and the risk for development of DFUs [22]. In addition, two case control studies conducted in Sudan and Iran reported that uncontrolled HbA1c was the main risk factor for development of DFUs [9, 23]. Also, it was found that incidence of DFUs was significantly associated with poor glycemic control [24]. From the above results it is clear that uncontrolled blood sugar was associated with development of foot problems, and raised the need to pay attention for checking blood sugar and HbA1c at regular interval bases to monitor the effectiveness of treatment they receive and control consumption of sugar.Our results indicated that diabetic patients who are currently smokers or ex-smokers are at higher risk of developing diabetic foot. Such findings are consistent with other studies which found that smoking was significantly associated with diabetic foot problem [15, 20]. Shailesh, et al. [25] revealed that the presence of DFUs was higher among habitual smokers or who were smokers or tobacco users. Furthermore, diabetic patients who are smokers undergo more amputations compared to those who did not smoke, and that increase the number of smoking years follow an increasing trend of more amputations [26]. These results revealed that proper foot care was a protective factor that decreases the chance of developing foot complications among diabetic patients, and in the other hand, poor foot care would be a risk factor for foot ulcers. Balla, et al. [14] reported that lack of self-care of foot was associated with developing diabetic septic foot. Similar to several studies [11, 27], our results indicated significant association between health education for diabetic patients and reducing the chances of developing DFUs. Even though the association between health education and DFUs was evident from the above results, but still large number of patients do not receive adequate information and instructions about the disease process. A cross sectional study found that 78.4% of patients had poor information about foot care [8]. Another study showed statistically significant associations between level of education and effective diabetic foot practice [28]. Furthermore, a study conducted in Iran found that 7.5% of subjects attended an educational program about self-care to prevent foot ulcers [12].
5. Limitations of the Study
- This study had several limitations, most notably, the small size of the sample in comparison with the large number of Palestinians who have diabetic foot ulcers. Another limitation was the insufficient documented clinical data in the subjects' files. Finally, this study was hospital-based cross sectional, so, there was lack of longitudinal data to follow the changes over time in risk factors for DFUs.
6. Conclusions
- This study found several factors associated with higher incidence of diabetic foot among diabetic patients including: low educational level, low household income, type I diabetes, being on insulin treatment, longer duration of diabetes (more than 10 years), HbA1c ≥ 7%, being current smoker or ex-smoker, poor self-care of foot, and lack of health education. Most of the identified risk factors were modifiable. Emphasis should be directed toward health education, changes in lifestyle, and following safety measures to decrease the higher incidence of diabetic foot complications in Gaza Governorates.
ACKNOWLEDGMENTS
- We would like to express our gratitude to all patients who participated in the study. Many thanks also go to the administrations of Gaza European Hospital, and Al-Shifa hospital for their cooperation during the study period. Their sincere contributions made this research fruitful and possible.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML