-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2014; 3(4): 66-70
doi:10.5923/j.diabetes.20140304.03
Effect of Hypertension on the Carotid Artery Intima Media Thickness (IMT) in Patients with Type 2 Diabetes Mellitus – Across Sectional Study
Tawfeeq F. R. AL-Auqbi, Ahmed Abduljabar Al-Sabbagh, Isam Noori Al-Karawi, Maan A. J. Bahrani
National Diabetes Center (NDC), AL-Mustansiriyah University, Baghdad, Iraq
Correspondence to: Tawfeeq F. R. AL-Auqbi, National Diabetes Center (NDC), AL-Mustansiriyah University, Baghdad, Iraq.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
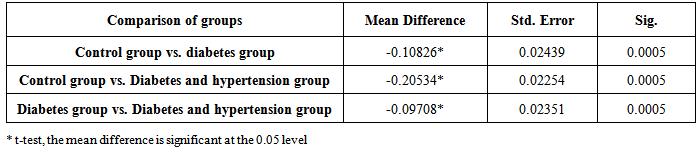
OBJECTIVES: To measure the additional effect of hypertension on the carotid artery (IMT) in type 2 diabetics. PATIENTSANDMETHOD: Cross sectional study, from 1st July 2012 to 30th December 2013, was conducted on 152 participants, 43 diabetes group 59 diabetes plus hypertension group and 50 healthy control persons, who were visiting the National Diabetes Center (NDC) / Al-Mustansiriya University, for periodic follow up and their healthy relatives. RESULTS:The differences between mean of the three groups for age, waist circumference, systolic blood pressure, fasting plasma glucose, HbA1c, total cholesterol, triglycerides, HDL-C and LDL-C were statistically significant. The mean differences in carotid artery (IMT) of mean of left and right common carotid artery between the three groups were statistically significant. The mean carotid artery (IMT) observed in diabetes group and diabetes plus hypertension group showed apparent increased by 24.81% and 31.69% respectively which were more than that of healthy control group. The net percentage of increase attributable to hypertension on mean carotid artery IMT was 6.88%. Effect size analysis showed an increased effect of diabetes and diabetes plus hypertension on mean carotid artery IMT, Cohen’s (d) 1.200 and 1.741 respectively. CONCLUSIONS:Diabetes and hypertension increase the carotid artery IMT independently. Coexistent hypertension with diabetes has an additive effect on the carotid artery IMT.
Keywords: Carotid intima media thickness, Hypertension, Type 2 diabetes mellitus
Cite this paper: Tawfeeq F. R. AL-Auqbi, Ahmed Abduljabar Al-Sabbagh, Isam Noori Al-Karawi, Maan A. J. Bahrani, Effect of Hypertension on the Carotid Artery Intima Media Thickness (IMT) in Patients with Type 2 Diabetes Mellitus – Across Sectional Study, International Journal of Diabetes Research, Vol. 3 No. 4, 2014, pp. 66-70. doi: 10.5923/j.diabetes.20140304.03.
Article Outline
1. Introduction
- Cardiovascular disease and its underlying atherosclerotic pathology, is the most common cause of death and disability in diabetic patients [1, 2]. The international atherosclerosis project suggested that atherosclerotic process occurs at the same time in carotid, cerebral and coronary arteries which leads to ischemic heart disease (IHD), cerebrovascular accidents and peripheral vascular diseases [3, 4]. Many researchers believe that assessment of carotid atherosclerosis can be done by measuring the thickness of intema media of common carotid artery (IMT) using ultrasonography. Hence, IMT can be a surrogate measure of the atherosclerosis process progression and/or regression [5, 6]. The carotid artery intima media thickness (IMT) also has proved to be a good marker for both early presence and extent of arteriosclerosis in an individual [7-10]. Prospective studies have shown a positive correlation between increased carotid artery IMT and the risk of myocardial infarction, stroke, and cardiovascular mortality [11]. Although, diabetes was a risk factor for atherosclerotic cardiovascular disease but an excess of cardiovascular risk and events in diabetic individuals was attributable to coexistent hypertension, link between hypertension and carotid atherosclerosis in diabetics was studied to explore the possible direct and indirect role of hypertension on IMT [6, 12, 13]. Therefore, we tried to measure the magnitude of additional effect of hypertension on the carotid IMT in type 2 diabetics.
2. Patients and Methods
2.1. Ethical Approval
- This study was performed according to the Helsinki II Declaration and approved by the ethical committee and the scientific research committee at the National Diabetes Center. All patients were informed about the aim and the suspected benefit of the study before obtaining their agreements for participation; although a written informed consent should be obtained from all enrolled participants but our participants preferred a verbal consent for privacy reasons.
2.2. Setting
- Cohort study, from 1st July 2012 to 30th December 2013, was conducted on 152 participants, who were visiting the National Diabetes Center (NDC)/ Al-Mustansiriya University.
2.3. Study Participants
- Participants were allocated to three groups, 43 diabetes group, diabetes plus hypertension group and control group. They were thoroughly interviewed, examined and investigated by a team of consultant physician, clinical nutritionist and consultant of ultra-sonography according to the approved standard medical and laboratory work up of the NDC. Participants were examined physically and their height, weight, body mass index (BMI), waist circumference (WC) and blood pressure were measured and recorded. Fasting blood samples were taken from all participants during their visits for laboratory analysis. Colored Doppler ultra-sonography measurements of carotid artery intima media thickness (IMT) of right and left common carotid arteries were done for all participants.
2.4. Inclusion Criteria
- Uncomplicated type 2 diabetes with/without hypertension and healthy participants, from both genders aged 30-75 years, were categorized to three groups, diabetes group, diabetes plus hypertension group and healthy control group (chosen from the healthy relatives and companions of the participants). Diabetes participants were selected according to the American Diabetes Association (ADA), Diagnosis and classification of diabetes mellitus (FPG ≥ 126 mg/dl). Diabetes with hypertension participants selected according to 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults, the Eighth Joint National Committee (JNC 8) (>140/90 mmHG) [14-16].
2.5. Exclusion Criteria
- Participants with diabetic complications (retinopathy, neuropathy and nephropathy), cardiovascular disease and on anti-lipid prophylactic therapy were excluded from the study.
2.6. Colored Doppler-Ultra-Sonography
- The duplex ultra-sonographic measurements were performed by FUKUDA DENSHI / UF- 750 XT. Ultrasound device with a 6-9 MHz linear probe (FUT-L D386-9A) was used to measure and calculate IMT of left and right sides, common carotid artery, and expressed in mm.
2.7. Laboratory Analysis
- Fasting blood sampels were taken from all participants during their visits for testing of fasting plasma glucose (FPG), HbA1c, serum cholesterol, serum triglyceride, HDL-C and LDL-C.
2.8. Statistical Analysis
- Statistical analysis and reporting of obtained data were carried out by using the SPSS Statistics version 19.0, the College of Saint Benedict and Saint John’s University (CSB.SJU) Minnesota, statistics to use website [17] and effect size calculator of the University of Colorado, Colorado Spring Website (UCCS) [18] Kolmogorov-Smirnov Test was used to examine the normal distribution of obtained data and Leven’s test was used to examine the homogeneity of variances. Data were reported and presented as mean ± SD and/or (95% confidence interval) for the normally distributed variables. Analysis of variance (ANOVA) and Post-Hoc (Tukey’s HSD test) were used to compare continuous variables between three groups. Statistical tests were approved by assuming a null hypothesis of no difference, a P values ≤ 0.05 was considered statistically significant. Sample size calculator by Raosoft Inc. was used to determine the sample size; also Cohen’s (d) was used to study the effect size of studied variables [18, 19].
3. Results
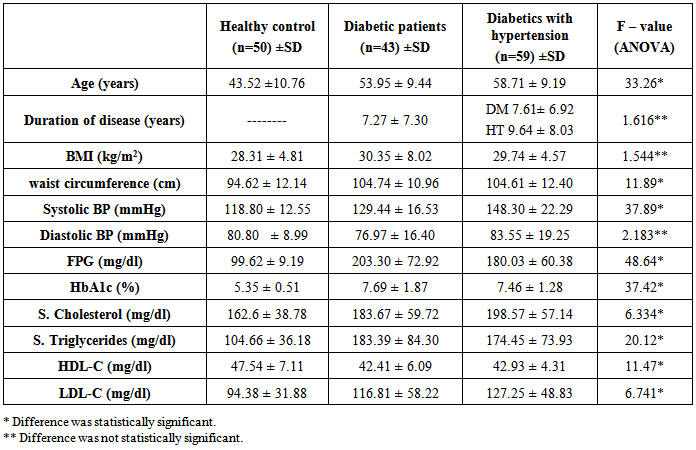
- A hundred and fifty two Participants were studied in three groups, diabetes group 43 subjects (22 men and 21 women), diabetes plus hypertension group 59 subjects (27 men and 32 women) and control group 50 healthy participants (25 men and 25 women) as control group.Anthropometric and metabolic characteristics (Table 1).
|
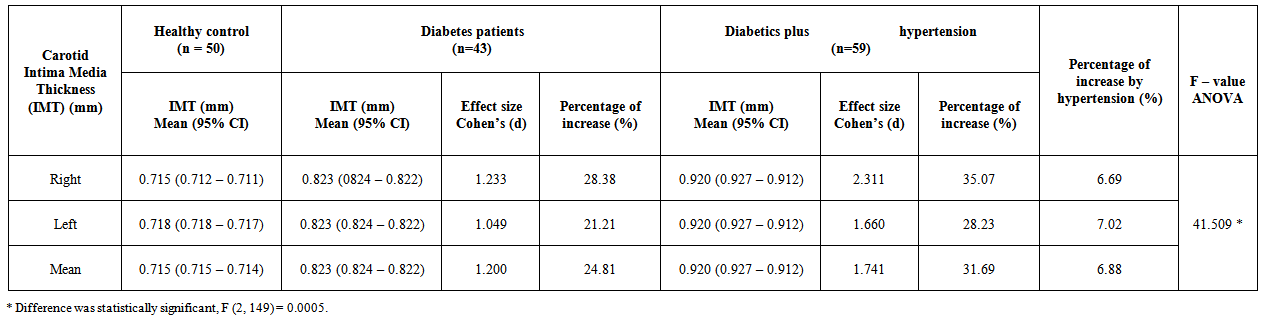 | Table 2. Carotid arteries Intima Media Thickness (IMT) of study population |
|
4. Discussion
- Anthropometric and metabolic parameters mean of our study (age, waist circumference, systolic blood pressure, FPG, HbA1c, S. cholesterol, S. triglycerides, HDL-C, and LDL-C) showed an increase in diabetes group than the control group; and more apparent increase of diabetes plus hypertension group than the other two groups, difference were statistically significant (ANOVA). The forwarded anthropometric and metabolic parameters could easily surrogated by measuring of carotid artery IMT and could be considered a good marker for the presence and progression of atherosclerosis, evidenced of existing cardiovascular diseases and prediction of future cardiovascular related diseases (MI, stroke, hypertension and death); also, carotid artery IMT may be used in clinical trials to evaluate the efficacy of interventions [20-23]. Many epidemiological studies focus on carotid artery IMT as a marker of generalized atherosclerosis and its correlation with established cardiovascular diseases and Framingham score [24-26]; we tried, in our study, to measure the impact and quantify the magnitude of effects on the carotid artery created by diabetes alone and diabetes plus hypertension in comparison to healthy persons. Carotid artery IMT can be used as a risk marker, to assess the risk of diabetes and hypertension quantitatively.Data records showed an increase of carotid IMT of diabetics group and diabetes plus hypertension group more than the healthy group by 24.81% and 31.69% respectively with net percentage of increase attributable to hypertension 6.88%. Our data finding prove that diabetes and hypertension are strong independent predictors of advanced carotid atherosclerosis and increase of carotid artery IMT [27]. Globally, there is an increasing interest, in most of the atherosclerosis and cardiovascular diseases guidelines, on further assessment and stratifying of patients according to their level of risk to design the plan of management according to their risk score [27-29]. The quantitative impact of risk factors on cardiovascular diseases were elucidated by Framingham Heart Study and other studies; the major risk factors are additive in predictive power [30].Analysis of effect size [18] of diabetes and diabetes plus hypertension on the carotid artery IMT, Cohen’s (d) =1.200 and 1.741 respectively, prove quantitatively the impact of diabetes alone and diabetes plus hypertension on the carotid artery IMT support our hypothesis of using carotid artery IMT to assess the magnitude of risk due to diabetes alone and the effect of hypertension coexisting with diabetes mellitus [31, 32]. We found the measurements of carotid artery IMT in our sample were like that found by Lundby et. al. [33] was 0.800±0.131 mm in diabetes patients and 0.679±0.105 mm in persons without diabetes; also, another study [34] showed 0.78 and 0.73 mm in diabetes and no diabetes subjects. Framingham study of risk score (FSRS) and Framingham cardiovascular risk score (FCRS) were 0.830±0.142 and 0.788±0.153 mm for cases and 0.773±0.142 and 0.726±0.149 for controls of both groups respectively [35]. We depend on measurements of carotid artery IMT done by the consultant of ultra-sonography using ultrasound device with a 6-9 MHz linear probe (FUT-L D386-9A) so we couldn’t avoid the observer and technical errors which might be raised; this limitation could be overcome in future work, so, we suggest depending on more than one observer, different measurement techniques and multicentre data collection.
5. Conclusions
- Diabetes and hypertension increase the carotid artery IMT independently. Coexistent hypertension with diabetes has an additive effect on the carotid artery IMT.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML