-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2014; 3(2): 15-21
doi:10.5923/j.diabetes.20140302.02
Impact of Shift Work on Glycemic Control in Insulin Treated Diabetics Dar El Chefa Hospital, Egypt 2014
Ihab Mohammadi El Tayeb1, Entesar Omar Ahmad El Saghier2, Basma Kamal Ramadan3
1Department of Community, Occupational and Environmental Medicine, Faculty of Medicine, Zagazig University, Egypt
2Department of Endocrinology and Metabolism, Faculty of Medicine for girls, Al-Azhar University, Egypt
3Department of Physiology, Faculty of Medicine for girls, Al-Azhar University, Egypt
Correspondence to: Entesar Omar Ahmad El Saghier, Department of Endocrinology and Metabolism, Faculty of Medicine for girls, Al-Azhar University, Egypt.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Background: Shift work has been associated with adverse health effects as it causes disturbance of circadian rhythms. Shift work is essential and unavoidable, even obligatory regimen in many occupations. Diabetic patients employed in shift work, particularly under insulintherapy may find difficulty in adjusting their glycemic control and the sleep pattern. Objectives: To compare glycemic control and microvascular complications among diabetic patients under insulintherapy, employee in shift work versus daytime work. Methods: In this cross-sectional study a total of 152 diabetic patient under insulin therapy shift work group (76), and daytime work (76) have been randomly selected; from attendant to outpatient clinic of diabetes and endocrinology, Dar El Chefa hospital. Questionnaires of demographicdata, especially employment status (shift work or daytime work), and Pittsburgh Sleep Quality Index (PSQI) have been applied. Assessment of microvascular complications of diabetes for every subject has been employed. A measurement of fasting, postprandial blood glucose, glycated hemoglobin (HbA1c) and albumin creatinine ratio (ACR) was applied. Results: The study revealed that shift work group, in comparison for daytime work group, has higher body mass index (BMI) 32.2(3.2)vs. 28.2(2.4)(P<0.05), poor-sleep-quality54(71.1%)vs. 6(7.9%)(P<0.05) and higher HbA1c9.8(1.2)vs. 8.1(1.3) (P < 0.05). In spite of the higher percentage of diabetic retinopathy, nephropathy, the difference was only significant for diabetic neuropathy. Conclusion: Our findings suggest that shift work adversely affect diabetic control and deteriorate measured HbA1c; and increase the incidence of microvascular complication.
Keywords: Shift work, Diabetes control, Complication
Cite this paper: Ihab Mohammadi El Tayeb, Entesar Omar Ahmad El Saghier, Basma Kamal Ramadan, Impact of Shift Work on Glycemic Control in Insulin Treated Diabetics Dar El Chefa Hospital, Egypt 2014, International Journal of Diabetes Research, Vol. 3 No. 2, 2014, pp. 15-21. doi: 10.5923/j.diabetes.20140302.02.
Article Outline
1. Introduction
- Shift work is an employment practice designed to make workers taking turns to have rest, where factories are required to operate all day. The term "shift work" normally includes both long-term night shifts and work schedules, in which employees change or rotate shifts [1]. There is no precise definition of shift work [2]. Simply, work that is scheduled outside “normal” daylight hours (i.e. 9 AM to 5 PM) is called “Shift work”. Schedules can be varied from one workplace to another. Unfortunately, night work cannot be avoided in some occupations [3]. Shift work, including night work, has been hypothesized to increase the risk of chronic diseases, including cancer [4], cardiovascular disease (CVD) [5] obesity [6], metabolic syndrome and diabetes [2], possibly due to an impairment of biological rhythm [2], lifestyle changes, job strain, stress, and social stress [7]. Recent data increasingly reveal relations between shift work and plasma resisting, ghrelin, leptin and adiponectin [2].The incidence of Type 2 DM (T2DM) has been recently increasing, mainly due to changes in lifestyle; such as over-eating, physical inactivity and sleep deprivation [8].Egypt is a developing and a lower middle-income country [9]. The changed consumption patterns of the Egyptian population due to changes in socio-economic status, feeding habits, urbanization and globalization during the last two decades, led to increased prevalence of obesity with Type 2 diabetes mellitus (T2DM) parallel to it [10, 11].In Egypt 10.4% of the adult population (aged 20 - 79 years) have diabetes. However, since Egypt has a relatively young population this is corrected to 11.4%, when used to compare with other countries [12]. With the rapid progress of industry worldwide, shift work itself become necessary in many occupations and the demands of round-the-clock services are increased in some companies [13]. Recently, shift workers represent more than 20% of the whole working population in industrial countries [14]. Intolerance of shift working due to failure to align the circadian rhythms to a new working time pattern is more likely in rapidly rotating shifts. For those with diabetes, such a work pattern requires necessary changes to meal times and the timing of insulin doses needs to be adjusted without inducing hypoglycemic episodes. This may account for their poorer glycemic control [15]. Moreover, our bodies are verified to have a regulatory mechanism to adjust the circadian rhythm [16]. Previous studies suggested that most shift workers were not able to adjust their circadian rhythms to the atypical timetable when they first started shift work [17]. Some of them then suffer from sleep loss and poor quality of sleep [1]. Diabetic patients under insulintherapy may find difficulty with employment because of restrictions placed upon them. Supposing that, they will face difficulty, especially in adjusting to irregular hours or shifts [18]. Until 1982 avoidance of shift work was supported by the British Diabetic Association, but this point of view has been revised with the development of newer insulin regimens and better methods of monitoring blood glucose [19]. Recently, any person with diabetes, whether insulin [treated] or non–insulin [treated], should be eligible for any employment for which he/she is otherwise qualified [20]. With changing the pattern of lifestyle being westernized, and a 24-hour societies, the current high prevalence and unavoidably of night shift work has potential health effects.Assessments of diabetic patients employed in shift work, especially those under insulin therapy, have been an urgent issue. In the present study, we compare glycemic control (fasting, postprandial blood glucose and HbA1c), microvascular complications and sleep quality between shift work and daytime work diabetic patients under insulin therapy.
2. Subjects and Methods
2.1. Study Design and Setting
- A cross-sectional study was conducted among diabetic patients randomly selected from attendants of diabetes and endocrinology outpatient clinic at Dar El Chefa hospital, Egypt (from March 2013 until February 2014). Our sample size was 182 diabetic patients from attendant of diabetic clinic within 3 month. A pilot study was conducted on 10 diabetic patients, who were excluded later from the study sample. The remaining 172 diabetic patients were eligible to participate. 20 of them refused to participate in the study, so the study was conducted on the remaining 152 patients. Only 152 diabetic patients were interviewed in the clinic. Our inclusion criteria was: diabetic patients with age range (18 – 65) years old , being under insulin therapy, either type 1 or type 2, duration of diabetes more than 10 years and fixed work pattern either shift work or daytime work for at least one year or more. For purpose of the present study non manual workers refer to white collar workers e.g. professional (clerk, nurses, teachers) and manual workers refers to blue collar workers (workers in factory, carpenters, plumbers etc).Exclusion criteria: diabetic patients under oral hypoglycemic medication and those who recently changed their pattern of work.
2.2. Data Collection
- a. The study questionnaires are composed of:(1) Demographic data (including age, gender, smoking, duration of employment in shift work or daytime work (in years), duration of diabetes, frequency of symptoms and suggestive hypoglycemic episode). They were classified according to type of work into shift work group (76 participants), which defined as (any work schedule involving unusual or irregular working hours and night work) and similar number (76 participants) of normal daytime work group (work schedule from 8:00 AM to 17:00 PM) [1]. (2) Pittsburgh Sleep Quality Index(PSQI) which measures the quality and patterns of sleep that differentiates “poor” from “good” sleep by measuring seven areas: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction over the last month. Scoring of answers is based on a 0 to 3 scale, whereby 3 reflect the negative extreme on the Likert Scale [21]. Minimum Score=0 (better); Maximum Score=21 (worse)Interpretation: Total < 5
 good sleep qualityTotal > 5
good sleep qualityTotal > 5  poor sleep qualityb. Physical examination:1. Measurement of height (m), body weight (kg), body mass index (BMI)2. Blood pressure was the average of three measurements made with a sphygmomanometer at two minute intervals. Any patient is considered hypertensive if he /she is already on antihypertensive medication or≥ 140 /90 According to the eighth Joint National Committee (JNC 8) [22].3. Assessment of diabetic neuropathy by using Foot sensitivity test which assessed by using Semmes-Weinstein monofilaments. The (10-g) monofilament was applied to nine sites on each foot. Each site was tested three times in random order, and in case of two or more failures per site to feel the monofilament, this was regarded as an incorrect answer. Impaired foot sensitivity was considered to be present if one or more incorrect answers were given for either foot [23].4. Fundus examination (by ophthalmologist) c. Laboratory test:Measurement of fasting and postprandial blood glucose, glycated hemoglobin and albumin creatinine ratio (ACR)Laboratory investigations were done in the local hospital laboratory as a part of routine laboratory.Determination of fasting and postprandial blood glucose level were measured by using Dialab B.S. 300 kit, Mindery), glycatedHbA1c (B.S 280-Kintic kit, Mindery). Urinary albumin and creatinine ratio (I Tachi 902 kit,<2.0mg/mmol (normoalbuminuria), 2.0-20mg/mmol(micro-albuminuria), >20.0 mg/mmol (macro-albuminuria) [24]
poor sleep qualityb. Physical examination:1. Measurement of height (m), body weight (kg), body mass index (BMI)2. Blood pressure was the average of three measurements made with a sphygmomanometer at two minute intervals. Any patient is considered hypertensive if he /she is already on antihypertensive medication or≥ 140 /90 According to the eighth Joint National Committee (JNC 8) [22].3. Assessment of diabetic neuropathy by using Foot sensitivity test which assessed by using Semmes-Weinstein monofilaments. The (10-g) monofilament was applied to nine sites on each foot. Each site was tested three times in random order, and in case of two or more failures per site to feel the monofilament, this was regarded as an incorrect answer. Impaired foot sensitivity was considered to be present if one or more incorrect answers were given for either foot [23].4. Fundus examination (by ophthalmologist) c. Laboratory test:Measurement of fasting and postprandial blood glucose, glycated hemoglobin and albumin creatinine ratio (ACR)Laboratory investigations were done in the local hospital laboratory as a part of routine laboratory.Determination of fasting and postprandial blood glucose level were measured by using Dialab B.S. 300 kit, Mindery), glycatedHbA1c (B.S 280-Kintic kit, Mindery). Urinary albumin and creatinine ratio (I Tachi 902 kit,<2.0mg/mmol (normoalbuminuria), 2.0-20mg/mmol(micro-albuminuria), >20.0 mg/mmol (macro-albuminuria) [24]2.3. Data Management
- The collected data were presented, summarized, tabulated and analyzed by using computerized software statistical packages SPSS version 19. P-value < 0.05 was considered statistically significant.
2.4. Ethical Issues
- Before interview, diabetic patients were informed of the general aim of the study and their participation in the study was fully on voluntary base. Informed consent has been obtained. Confidentiality of collected data was guaranteed to participants.
3. Results
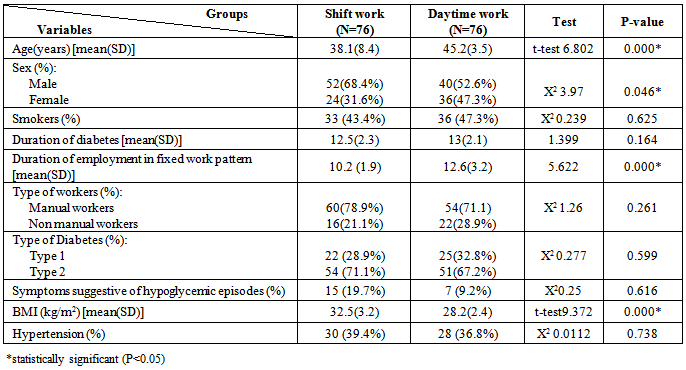
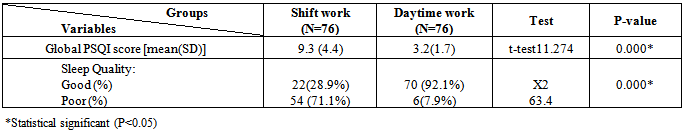
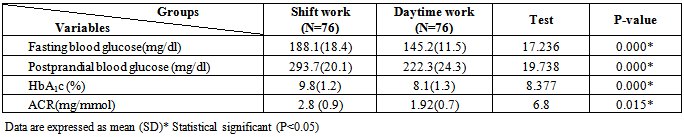
- This table shows that no statistical significant difference as regard sex, smoking, duration of diabetes, duration of employment and the percentage of those having symptoms suggestive of hypoglycemic episodes, and hypertension between the two groups (p>0.05). While age is higher in daytime group than shift work group and the difference in between are statistically significant (P< 0.05). Mean of BMI was higher among shift group than daytime group (P<0.05). Most the patients of the study are type 2 diabetes (71.1%) in shift work group ,(67.2%) in daytime group and manual workers (78.9%) in shift work and (71.1%) in day time work.This table shows higher mean PSQI global score among shift work group than daytime group and the difference in between are statistically significant (P<0.05). The frequency of poor sleep quality are higher (71.1%) among shift work than daytime work (7.9%) and the difference in between are statistically significant (P < 0.05).
|
|
|
|
|
|
|
4. Discussion
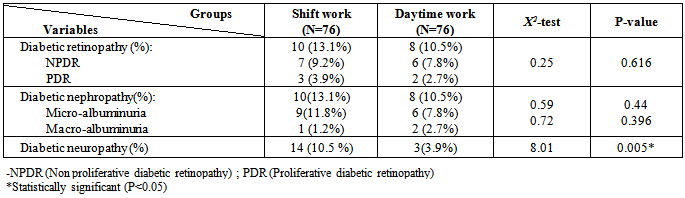
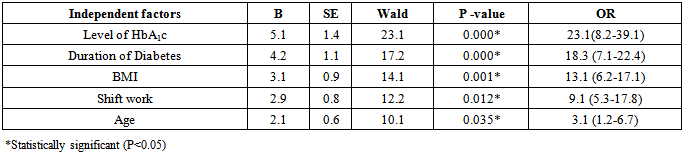
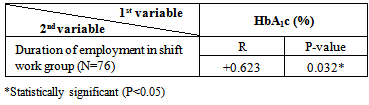
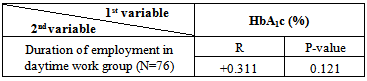
- In the present study, table 1 shows both groups had high BMI, but shift workers had higher BMI than daytime workers and the difference in between was statistically significant. As well as they complained of more frequent symptoms suggestive hypoglycemia, albeit, of no statistical significance. Also Poole et al [19] found similar results, shift and night work leads to differing activity levels and changes to meal times and may involve snacking on high fat foods as these may be all that is available outside normal working hours [25].In agreement with our study, a study by Niedhammar et al. [26] shows that weight gains was more frequent among nurses on night work than daytime work. In terms of obesity or high BMI, majority of cross-sectional studies indicate that shift work increases weight gain and the prevalence of obesity. On the other hand, half of cohort studies show higher frequency of meal intake and/or poor nutrition quality in the shift workers. Generally, it is indicated that shift working negatively impacts on health and nutritional status of workforces [27]. Shift work and long work hours increase the risk for reduced performance on the job, obesity, injuries, and a wide range of chronic diseases. In addition, fatigue-related errors could harm patient [28]. However a number of studies have not been able to confirm weight differences between shift and day work [29].Sleep is increasingly recognized as an important factor in the homeostasis of multiple body functions [30]. Many adverse health effects such as anxiety, endocrine disorders could hit the body following sleep deprivation [31]. Shift work, especially night rotating shift work, could reduce sleep quality directly by disturbing chronobiological rhythms [32], and reducing the secretion of melatonin [33]. The results of the present study confirmed the elevated frequency of poor sleeping quality in shift works versus daytime workers (71.1%)vs. (7.9%) respectively, P<0.05. This is in agreement with Saudi study by Al Metrek et al. [34], that showed shift workers with poor sleep quality represent 67.6% compared to only 20.3% of non- shift group, and the difference is statistically significant. A study in Japan shows also similar results, among Japanese workers, for non-shift workers, poor sleep quality was 33 to 44% and 42 to 45% for men and women, and excessive daytime sleepiness was 7% and 13% for men and women, respectively [35]. During shift work, the workers have to change the bed time frequently [36]. Shift work is associated with chronic misalignment between the endogenous circadian timing system and behavioral cycles, including sleep-wake and fasting-feeding cycles [37]. Experimental studies have shown that sleep deprivation and disturbed sleep tend to decrease glucose tolerance and compromise insulin sensitivity [38]. A study by Monk and Buysse [39] shows that shift work exposed groups reported an increased proportion of self-reported diabetes in comparison to daytime work group, the effect remained significant after adjusting for gender and body mass index.In the present study, both groups had uncontrolled diabetes , but with higher fasting and postprandial blood glucose level and HbA1c among shift work group than daytime group and the difference in between are statistically significant. Also, there is a moderate positive correlation between duration of employment in shift work and HbA1c level, while there is weak positive correlation between duration of employment in daytime work group and HbA1c, so it is clear that night-shift has more impact on deterioration of diabetes control. A study by Young et al. [15] shows poorer control of diabetes was associated with working shifts. Recent research continues to show that sickness absence is higher in people with diabetes (types1 and 2) [40]. So, physicians should be aware of this association and be able to advice on management strategies to improve diabetic control while working shifts. Changes in the circadian rhythms of counter-regulatory hormones may also impact on the ability to control blood glucose, an example being the dawn phenomena where blood glucose elevation occurs in the morning as result of changes of counter regulatory hormones [25].This study revealed a higher prevalence of microvascular complications, diabetic retinopathy and nephropathy among shift work group than daytime group (13.1%vs. 10.5%), (13.1%vs. 10.5%) respectively (P>0.05). While, the difference are more obvious among higher frequency of diabetic neuropathies among shift work group 10.5%vs. 3.9 % (P<0.05).Data from the Diabetes Control and Complications Trial (DCCT; type 1 diabetes) (DDCT, 1995) and the United Kingdom Prospective Diabetes Study (UKPDS; type 2 diabetes) demonstrated a continuous relationship between HbA1c and diabetes complications [41]. Targetglycated hemoglobin of less than 7% has commonly been recommended in hopes of preventing both macrovascular and microvascular complications, however the evidence for similar benefits for macrovascular disease has been less clear. Recent results from the Action to Control Cardiovascular Risk in Diabetes (ACCORD), Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE), and Veterans Affairs Diabetes Trial (VADT) studies have challenged the conventional believe that lower glycated hemoglobin values should be pursued in all diabetic patients [42]. On logistic regression analysis, it was found that the most important predictors of diabetic neuropathy among our study groups were control of HbA1c (OR = 23.1), for duration of diabetes (OR = 17.2), for shiftwork workers (OR = 12.2), for age (OR = 10.1). These results showed that control of HbA1c was the most important predictor of developing diabetic neuropathy and in consequently other micro vascular complication of diabetes. It seems shift work has its impact on developing diabetic neuropathy indirectly through deterioration of HbA1c control, the results were supported by previous studies, which concluded that tight control of diabetes are associated with less incidence of diabetes neuropathy [41,42].
5. Conclusions and Recommendations
- Our findings suggest that shift work adversely affect diabetic control (deteriorate measured glycatedhaemoglobin) and microvascular complications. Diabetologists and Occupational health practitioners should therefore be aware by this notion for diabetic patients treated by insulin and be able to advise workers with the best way to manage diabetes during shift work and when rotating their shift patterns. Future research may address the role of insulin analogue in such shift work with the concept of their flexibility and less adverse effect of hypoglycemia than conventional insulin.
ACKNOWLEDGEMENTS
- The authors wish to thank all staff in the local laboratory of Dar El Chefahospital for their support and cooperation during the study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML