-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2013; 2(6): 91-95
doi:10.5923/j.diabetes.20130206.01
Louisiana Diabetes Excellence Initiative: Accomplishing Excellence in Diabetes Self-Management in a Rural Community
Praphul Joshi1, Caren Pourciau2, Alok Bhoi3, Lynn Kinchen4
1School of Community and Population Health, University of New England, Portland, ME 04103, USA
2Chronic Disease Nurse Consultant, Louisiana Department of Health and Hospitals
3Chronic Disease Epidemiologist, Louisiana Department of Health and Hospitals
4Obesity / Diabetes Prevention and Control Program Monitor, Louisiana Department of Health and Hospital
Correspondence to: Praphul Joshi, School of Community and Population Health, University of New England, Portland, ME 04103, USA.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Aims:To evaluate the impact of diabetes self-management interventions implemented as a part of Louisiana Diabetes Excellence Initiative (LaDEI)Methods:Mixed methods were used for impact evaluation. Quantitative measures included clinical measures, self-management activities and participation rates. Qualitative measures included individual interviews with the clinical staff at the intervention site as well as with the clinical staff of a comparison clinical site that did not offer any specific interventions targeting type-II diabetes. Results:Clinical measures including lipid profile, controlled hypertension and obesity (body mass index) improved over the two-year period. Qualitative data indicated a high level of satisfaction among the providers and improved patient compliance. The comparison site indicated a high drop-out rate of their patients with diabetes and demonstrated a need to have community-based interventions targeting diabetes. Conclusions:Results if this initiative indicates a need to implement more interventions involving self-management activities to reduce the burden of diabetes among rural and underserved populations.
Keywords: Diabetes self-management, Health disparities, Qualitative methods
Cite this paper: Praphul Joshi, Caren Pourciau, Alok Bhoi, Lynn Kinchen, Louisiana Diabetes Excellence Initiative: Accomplishing Excellence in Diabetes Self-Management in a Rural Community, International Journal of Diabetes Research, Vol. 2 No. 6, 2013, pp. 91-95. doi: 10.5923/j.diabetes.20130206.01.
Article Outline
1. Introduction
- Type-II Diabetes affects 26 million Americans and results in premature death and serious health conditions[1]. Disparities in outcomes among people with diabetes care are related to differences in self-management. Helping these patients better self-manage their diabetes can avoid diabetes-related complications. However, engaging in self-care activities is especially challenging for the 70% of those having diabetes who suffer from co-morbid conditions such as chronic pain, hypertension and obesity[2]. Patients with diabetes who have comorbid conditions face substantial challenges in disease self-management, interfering with their ability to take medications, exercise, follow an eating plan, self-monitor, and foot care[3]. There are many different approaches to diabetes self-management that have been shown to improve health outcomes (including glycemic control) and reduce emergency room visits. The prevalence of type-II diabetes in the U.S. has been increasing in the last two decades mainly due to higher obesity rates, rise in ageing population and co-existing morbidities such as hypertension and depression.[1] Based on the hemoglobin A1C (HbA1C) measures, about 35% of the US adults ages 20 and above have pre-diabetes and every year about 2 million new cases of diabetes are being reported.[2] Diabetes is a major cause of cardiovascular diseases as well as the leading cause of kidney failure, non-traumatic limb amputations, and new cases of blindness in the U.S.[2,3] Type-II diabetes is the fifth leading cause of death in the US, although many more people with diabetes die due to other complications such as cardiovascular diseases.[1,4] In addition to the above complications, about 60 – 70% of people with diabetes suffer from neurological problems including impaired sensation in hands and feet, carpal tunnel syndrome, erectile dysfunction and other nerve problems.[5] In 2007, the estimated direct and indirect costs related to diabetes in the US were $174 billion of which $116 was attributable for direct medical costs. The substantial indirect costs ($58 billion) include disability, work-loss, and premature mortality.[1,3,4] These costs are estimated to continue to rise. The majority of the costs related to diabetes complications and treatment can be avoided by patient self-management leading to behavioral modifications and stricter adherence to medications.[5,6]Similar to the US, diabetes is a public health concern in Louisiana. In 2011, an estimated11.8% of the adult population of Louisiana was diagnosed with diabetes.[7] Theprevalenceof diabetes has steadily increased from 6.6% in 2000 to 11.6% in 2011, with Louisiana rates consistently exceeding national rates.[7] In addition, another 7.5% of adults were identified as having pre-diabetes in 2011. The prevalence of diabetes was higher among males than females (12.2% vs. 11.4%, respectively). African Americans (15.8%) reported a higher prevalence rate than any other racial/ethnic groups.[7] Individuals of lower socioeconomic status (i.e., education and income) seem to be at greater risk for Type 2 diabetes and pre-diabetes. Diabetes is the fifth leading cause for deaths among Louisiana residents.Louisiana has the 5th highest diabetes mortality rate (26.4/100,000 population) in the nation for 2010.Despite having significant benefits, the percentage of people having diabetes adhering to self-management protocols is very low.[8] Socio-economic status (SES) is a significant determinant of self-management as it directly impacts access to health care, utilization of resources and lack of understanding of the disease (driven by lower education status).[9,10] Besides SES, several co-morbid conditions including chronic pain, hypertension and depression contribute towards decreased adherence to self-management protocols.[5,8] Chronic pain is the most important factor interfering with self-management, more important than any other condition.[2] This project explicitly addresses the personal, social, and clinical factors that complicate diabetes self-management. The long-term goal of this study is to learn if better self-management activities improve patient outcomes.Several interventions have been implemented nationally, based on DSME and other standardized guidelines.[5, 8] The use of evidence-based performance and outcome measures has been adopted by organizations and initiatives such as the Centers for Medicare and Medicaid Services (CMS), the National Committee for Quality Assurance (NCQA), the Diabetes Quality Improvement Project (DQIP), the Health Plan Employer Data and Information Set (HEDIS), and the Veterans Administration Health System.The Louisiana Diabetes Excellence Initiative (LaDEI) is a collaborative program between the Louisiana Department of Health and Hospitals (DHH), Diabetes Prevention and Control Program (DPCP) and designated health care systems. The LaDEI goals were to (1) reduce health disparities related to diagnosis and treatment of diabetes, (2) improve chronic disease health care delivery for patients diagnosed with diabetes, (3) reduce risk factors for diabetes related complications, (4) and to develop systems to capture health care delivery data and information that will be used to define a seamless and well coordinated approach to reducing chronic disease prevalence and health care disparities within the State of Louisiana. The Louisiana DPCP used funds from another funding source (FLEX Medicare grant, Quality improvement) within the Bureau of Primary Care and Rural Health to help a Rural Health Clinic (RHC) purchase an electronic diabetes registry (DiaMed). This interdepartmental collaboration with the Bureau was essential to the success of the LaDEI initiative with the RHC. The RHC adopted the National Committee for Quality Assurance Diabetes Recognition Program (NCQA DRP) and populated the registry with the NCQA-DRP measures. Staff was educated on tracking and reporting clinical measures on all patients of the two LaDEI providers. The American Association of Diabetes Educators recognized program for patient self –management education at RHC and continue to share the registry with the rural health clinic to successfully achieve the goals of LaDEI. Educational information and webinars were shared through the diabetes list-serv and available for clinic providers and staff, billing and coding staff and LaDEI staff. Tobacco cessation was monitored and referred to a community network for tobacco cessation help.
2. Subjects
- Participants for this initiative included patients attending the RHC who had a diagnosis of type-II diabetes. Initial assessments of patients were conducted and entered in the database from September 2011 through February 2012. The patients were followed up until June 2013. Initial goal of the initiative was to follow-up 100 patients from baseline till completion. However, the number of participants of LaDEI exceeded the initial goals and 196 were registered during the first six months. The final assessment had a sample of 149, which was significant considering the drop-out rates in other initiatives. All the intervention activities including foot exam, nephrological exams, eye care, smoking cessation, and nutrition / physical activity sessions were offered to all the participants at no cost. Participation in all the activities were entered in the registry and every effort was made to protect the confidentiality of the patients.
3. Materials and Methods
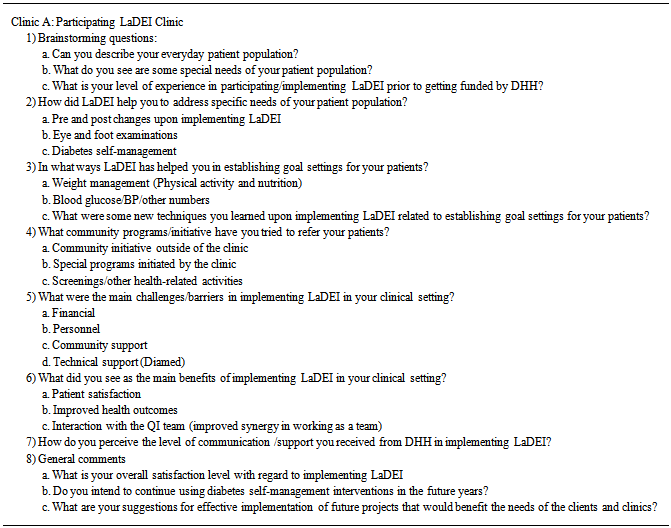
- A mixed methods approach was used for evaluating the impact of LaDEI. Quantitative measures included clinical assessments including HbA1C, blood pressure (systolic and diastolic) and lipid profile (LDL). Obesity status was measured through body mass index (BMI) and smoking status was assessed during routine clinical visits. Referrals to foot exam, eye exam and counseling for smoking cessation were tracked on the DiaMed registry as well. Constant staff training and validation by co-workers accomplished quality control in data management. Qualitative measures included data from in-person key informant interviews at the clinical site as well as a comparison site that did not have any specific diabetes self-management interventions. Individual interviews were conducted with two lead physicians, two diabetes educators (nurses) and a data coordinator (also a nurse). Table 1 represents the list of questions that were asked during the in-person interviews. The set of questions were slightly modified for the interviews at the comparison clinic. The comparison clinic had very similar geographic and demographic characteristics but no specific intervention related to diabetes. All the interviews were conducted in a secure room to assure privacy and maintain confidentiality. The interviews were audio-recorded and decoded into a text format to enable interpretation and coding. An interpretative coding technique was used to analyze qualitative data.
|
4. Results
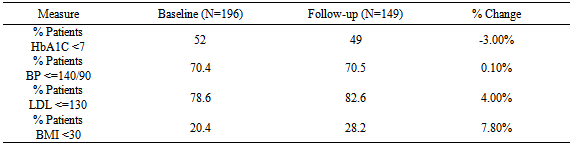
- Summary results of LaDEI are reported in Table 2 during the two-year funding period. The project exceeded in meeting the number of patients (compared to original goal of 100 patients) served in rural areas for promoting diabetes self-management. The project had an initial patient pool of 196 and the sample for the final measures was 149. Although the primary outcome measure (HbA1C under control) did not show any improvements, the secondary outcome measures (LDL under control, BP under control) improved. In addition to the outcome measures, percentage of patients with BMI less than 30 increased by 7.8%.
|
5. Discussion
- According to the National Diabetes Self-management Education (DSME), self-management of diabetes includes compliance to the medication protocols (taking insulin as well as oral medications regularly), obtaining annual eye and foot examinations, exercising regularly, maintaining a healthy diet as well as adhering to medical protocols for pre-existing conditions, particularly hypertension.[1,6] Adherence to self-management protocols leads to significant reductions in diabetic complications.[5] There are many documented factors that contribute to successful blood glucose control, but the ability of patients to manage their diabetes is critical because adherence with therapeutic regimens can prevent or delay the onset of complications and improve health outcomes.[9,10] The key to successful diabetes management is heavily dependent upon the education, knowledge and diabetes self-management skills of each individual.[11] This project has addressed critical barriers to self-management of diabetes by focusing on comorbid conditions as well as increasing the knowledge and skills related to diabetes control.Implementing self-management intervention like LaDEI in a rural health center provided number of benefits both to the clinic as well as for the community. The intervention provided patients with free access to eye exams, foot care, smoking cessation and behavior modifications to reduce the complications of diabetes and improve their clinical outcomes. It should be noted that HbA1C changes represent intermediate outcomes of the project and sustained interventions are needed to see further improvements in numbers. Given the rural nature of the population as well as the socio-economic challenges in the community served, the project provided positive results to indicate a need for self-management initiatives to control chronic diseases elsewhere in the state. Qualitative measures indicated a need for patient education and motivation due to very low education status / reading levels of the target population.
ACKNOWLEDGEMENTS
- This publication was supported by the Cooperative Agreement Number 5U58DP001970-06 REVISED, from The Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of The Centers for Disease Control and Prevention.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML