-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Diabetes Research
p-ISSN: 2163-1638 e-ISSN: 2163-1646
2012; 1(3): 36-41
doi: 10.5923/j.diabetes.20120103.02
Determinants of Abnormal Liver Function Tests in Diabetes Patients in Myanmar
Han Ni 1, Htoo Htoo Kyaw Soe 2, Aung Htet 3
1Department of Internal Medicine, Melaka Manipal Medical College, Melaka, 75150, Malaysia
2Department Community Medicine, Melaka Manipal Medical College, Melaka, 75150, Malaysia
3Department of Diagnostic Radiology, Singapore General Hospital, 169608, Singapore
Correspondence to: Han Ni , Department of Internal Medicine, Melaka Manipal Medical College, Melaka, 75150, Malaysia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
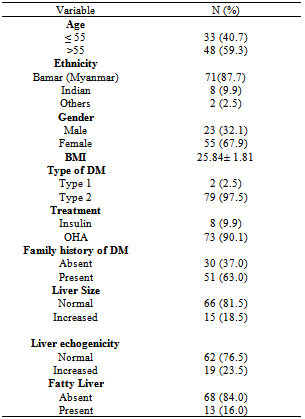
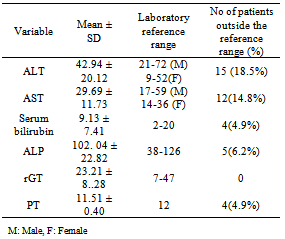
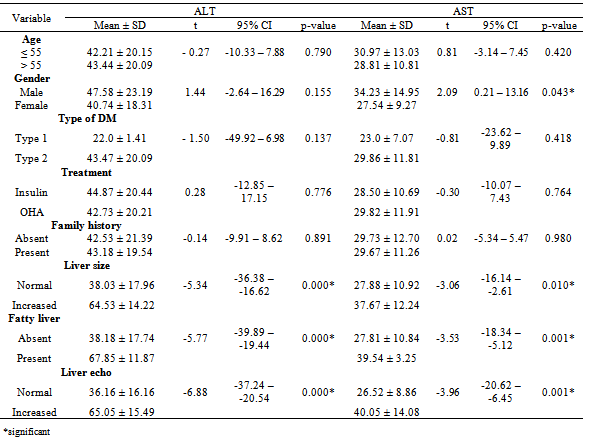
Abnormal liver function tests are not uncommon encounter in diabetes mellitus patients. The aim of this study was to find out the liver function test abnormalities in a group of diabetic patients in Myanmar and to determine the factors associated with these biochemical changes. In this cross sectional study conducted at the diabetic clinic of Yangon General Hospital, Myanmar between March 2006 and February 2007, a total of 81 patients were included. The means of alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), γ glutamyl transferase (γ GT), bilirubin and prothrombin time fall within normal range. Raised ALT and AST were noted in 18.5% and 14.8% respectively. 4.9% had high bilirubin and prolonged prothrombin time each, γGT was normal in all patients. The mean values of ALT and AST had no significant correlation with age, family history of diabetes, mode of therapy or type of diabetes. Although mean ALT had no correlation with gender of the diabetes patients, AST was found to be significantly elevated in men. Values of ALT and AST were also significantly higher with increasing BMI. Hepatomegaly, increased liver echogenicity and presence of fatty liver were the factors significantly correlated with elevated ALT and AST values. In conclusion, abnormal liver function results are more common among diabetes patients. Elevated ALT and AST are the markers for associated non alcoholic fatty liver disease in diabetes patients. Testing for ALT and AST, should be carried out to screen underlying fatty liver, especially in male diabetes patients with high BMI.
Keywords: Liver Function Tests, Diabtes Mellitus, Myanmar, Alanine Aminotransferase, Aspartate Aminotransferase
Article Outline
1. Introduction
- Diabetes mellitus is one of the major non-communicable diseases and the prevalence is rising globally. Type 2 diabetes is the most common form, accounting for 90% of all cases[1]. The prevalence of diabetes worldwide was estimated to be 2.8% in 2000 and 4.4% in 2030. The total number of diabetes is projected to increase from 171 million in 2000 to 366 million in 2030. Diabetes is more prevalent in men than women[2].There exists an association between diabetes and liver injury. Liver plays a major role in the regulation of carbohydrate homeostasis. Hepatocellular glycogen accumulation leads to hepatomegaly and liver enzyme abnormalities in poorly controlled diabetes patients. In hyperglycemic states, there will be intracellular glycogen accumulation in the hepatocytes due to increased glycogen synthesis, causing typical biochemical findings of mild to moderately elevated aminotransferases, normal liver synthetic function, with or without mild elevations of alkaline phosphatase. All these biochemical disturbances and hepatomegaly are found to be reversible with good glycemic control[3]. Secondly, liver can be affected by steatosis or accumulation of fat, a condition known as non-alcoholic fatty liver disease (NAFLD). It is a well-recognized complication of diabetes with frequency of 40–70%[4]. Associated obesity is a confounding variable for fatty liver. Increased transport of fatty acids to the liver, enhanced hepatic fat synthesis as well as decreased oxidation or removal of fat from the liver lead to fat accumulation in the liver. The steatosis is either microvesicular or macrovesicular and is found to progress to fibrosis and cirrhosis. The most common clinical finding is hepatomegaly, with normal or only mildly elevated transaminases and normal bilirubin. These changes are not reversible with sustained glucose control[4].Nonalcoholic fatty liver disease (NAFLD) is the main cause of chronic liver disease associated with diabetes and obesity. It was first reported in 1980’s in obese females with diabetes. Without treatment, compensated steatosis in NAFLD will eventually lead to decompensated steatosis with necroinflammation and fibrosis, i.e stage of non-alcoholic steatohepatitis (NASH). NASH is a leading cause of end-stage liver disease and also a contributor of cardiovascular disease in type 2 diabetes mellitus[5].Definitive diagnosis of NASH requires liver biopsy. However, new imaging methods like transient elastography and plasma biomarkers such as cytokeratin-18 fragments (marker of hepatocyte apoptosis) are emerging as alternative diagnostic techniques. Lifestyle modification is the gold standard in the management of NASH. Thiazolidiendiones have shown some promising results in recent randomized controlled trials[5]. Serum amino transferases such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST) indicate the concentration of hepatic intracellular enzymes that have leaked into the circulation. These are the markers for hepatocellular injury and are used as primary screening of NASH[6]. Chronic mild elevations of ALT and AST are seen in type 2 diabetes patients. In a study done in United States by Erbey et al in 2000, the prevalence of elevated ALT among type 2 diabetes is 7.8% compared to 3.8% in those without diabetes[7]. In another study by Salmela et al, elevated ALT in diabetes patients was associated with increased BMI and poor glycemic control in multivariate analysis[8].Elevated liver enzymes are found to be predictors of future cardiovascular disease in some studies. In the Firenze Bagno a Ripoli (FIBAR) study done in Italy, raised gamma-GT of more than 40 U/L and AST of more than 40 U/L were associated with increased incidence of Cardiovascular Disease (CVD)[9]. However, subsequent reviews conclude that diagnosis of NAFLD is insufficient to consider as high risk for CVD. The presence of NAFLD should prompt for screening of diabetes, but CVD screening should be guided by other established cardiovascular risk factors[10]. In Myanmar, the estimated prevalence of diabetes mellitus was 2.4% in 1995, 2.5% in 2000 and expected to be 3.2 % in 2025 according to World Health Organization (WHO) estimates and projections 1995-2025[11]. There is no doubt that the morbidity of diabetes mellitus is increasing in Myanmar, especially in the urban population.The aim of this current study was to evaluate the liver function among diabetes patients in Myanmar and to find out the factors associated with these abnormalities.
2. Materials and Methods
2.1. Study design and Subjects
- This study was a hospital based cross sectional descriptive study conducted at the diabetic clinic of Yangon General Hospital, Yangon, Myanmar between March 2006 and February 2007. Subjects were recruited according to simple random sampling method meeting the selection criteria.
2.2. Selection Criteria
2.2.1. Inclusion Criteria
- The patients with confirmed diabetes mellitus or newly diagnosed diabetes mellitus by WHO criteria (1999), fasting plasma venous glucose of ≥ 7 mmol/l (126 mg/dl) or random or two hour post prandial plasma venous glucose of ≥ 11.1 mmol/l (200 mg/dl).
2.2.2. Exclusion Criteria
- The diabetic patients with history of alcohol intake, hepatotoxic drugs like amiodarone, antituberculous drugs, history of liver diseases or clinical evidence of acute hepatitis, those who were found to have evidence of hepatitis B and C virus infection (HBsAg positive and HCV antibody positive) were excluded from this study.
2.3. Ethical Considerations
- The Institution’s Ethical Committee approval was obtained prior to the enrolment of subjects. The objectives and the detailed procedures of blood taking and imaging involved in the study were explained to all eligible subjects for this study. Emphasis was given that participation in this study was voluntary. Written consent forms were obtained from all participants who agreed to take part in the study.
2.4. Questionnaire and Biodata Collection
- A questionnaire was specifically designed to obtain information which helps to select individuals according to the selection criteria of the study. The questions also focused on sociodemographic data (age, sex, ethnicity) and background characteristics of diabetes (family history of diabetes, duration and type of diabetes mellitus, mode of anti-diabetic therapy). Weight and height were measured using standard procedures and Body Mass Index (BMI) was then calculated from the formula of weight(kg)/height(m2).
2.5. Blood Sample
- 5 ml of venous blood was drawn from each volunteer in this study using a disposable plastic syringe. The sample was then analysed for serum bilirubin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), γ glutamyl transferase (GGT), prothrombin time (PT) by 550 Expressed Plus Automatic Chemistry Analyzer at the pathology department of Yangon General Hospital.
2.6. Imaging of Liver
- Ultrasonographic examination of abdomen was carried out at the radiology department of Yangon General Hospital to determine the size, echogenicity of liver and the presence of fatty liver.
2.7. Statistical Analysis
- The data collected during the current study were recorded and analyzed statistically to determine the significance of different parameters by using SPSS package for windows version 16.0.
3. Results
|
|
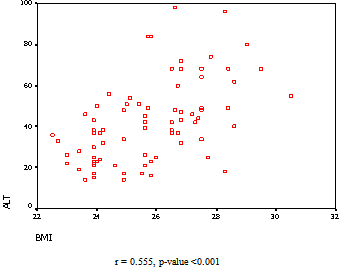 | Figure 1. Correlation between ALT and BMI among diabetes patients (n = 81) |
|
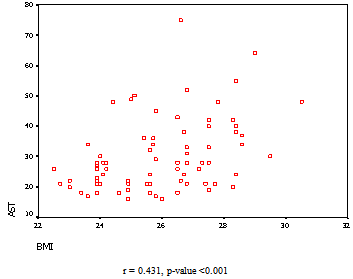 | Figure 2. Correlation between AST and BMI among diabetes patients (n = 81) |
4. Discussions
- Type 2 diabetes patients have been reported to be associated with higher incidence of abnormal liver function tests (LFT) compared to the individuals without diabetes, elevated ALT being the most common abnormality[12]. Salmela et al in 1984 studied the liver function tests of 175 diabetic patients without chronic liver disease, where 57% were found to have at least one abnormal LFT, 27% had at least two abnormal LFTs. However, these increases in liver function values were rarely more than two times of the upper limit of normal[8].A cross sectional study from Iran demonstrated a rise of ALT and AST in 10.4% and 3.3% of type 2 diabetes patients respectively[6].In a UK cohort study of 959 diabetic patients over four year period, 15.7% had raised ALT, 10.4% had elevated alkaline phosphatase whereas only 3.9% hadhyperbilirubinaemia[13]. Another study of 60 well controlled diabetic outpatients showed elevation of alkaline phosphatase and γGT in 11 and 10 patients respectively, but the rise was not more than two times upper limit of normal value[14]. According to a study in Sudan, where 50 diabetes patients and 30 normal control subjects were tested for liver function, the means of ALT, AST, γGT, total protein and albumin were reported to be significantly higher among diabetes compared to the control. However, the mean values were within the normal range[15]. In this study, 22% had at least one abnormal liver function test.Similar finding was also present in a study by Foster et al, in which the means of ALT, AST, ALP, γGT, bilirubin and albumin of 60 study subjects with diabetes were within the reference range[14].Likewise in our study, the means of ALT, AST, ALP, γGT, bilirubin and prothrombin time were within normal range among 81 diabetes patients. Raised ALT and AST were noted in 18.5% and 14.8% respectively. 4.9% had high bilirubin and prolonged prothrombin time. In contrast to the study by Salmela et al, where raised γGT was reported in 19% of diabetes patients[8], none of the diabetes patients in our study had elevated γGT. Abnormal liver function tests in diabetes patients can be attributed to several factors, the most common cause being non alcoholic fatty liver disease (NAFLD) associated with insulin resistance and metabolic syndrome in diabetes. Recently, studies have revealed the association of hepatitis C virus infection in diabetes patients causing deranged LFTs[16]. Though relatively infrequent, statin therapy can also contribute to abnormal liver function results[12].Majority of the studies on liver function in diabetes excluded the hepatotoxic causes of viral hepatits, alcohol and medications. These studies focused on the factors influencing the liver function in diabetes. Elevated ALT was significantly associated with overweight, short duration of diabetes, poor glycemic control and those treated with diet control or oral agents on multivariate analysis according to Salmela et al. In this study, the histologic changes were also studied but no significant correlation was present between liver histology and raised ALT nor γGT[8]. Contrary to the above study, Foster et al reported no significant correlation between measures of glucose control and abnormal liver function tests. However, they found that presence of abnormally bright liver echo on ultrasound imaging was associated with minimally elevated ALT and ALP. This bright liver echo was due to fatty infiltration of liver[14]. Among the Iran diabetes population, although raised ALT was seen with increasing age, fasting blood glucose and triglyceride levels, it was not statistically significant. The risk of higher ALT was significantly lower with longer duration of diabetes. The incidence of high ALT was more common among men[6].Erbey JR et al reported that the prevalence of elevated ALT levels among the U.S. type 2 diabetics was 7.8% and this prevalence was higher among obese (BMI > 25kg/m2) than non-obese diabetics (10.6% vs. 6.6%)[7].In Sudan, high serum alanine aminotransferase level is greater among type 2 diabetes, overweight or obese and men[15]. The elevated ALT levels were significantly related to a BMI of > 25 kg / m2 among the type 2 diabetics (p=0.0103) in a study conducted in India. Positive correlation was also reported between glycaemic control (FBS and PPBS) and duration of diabetes mellitus with the ALT levels in this Indian study[17].According to a study in India, age, duration of diabetes, presence of hypertension, family history of diabetes mellitus, body mass index, waist circumference, treatment with Metformin, and prevalence of metabolic syndrome were similar between diabetes patients with and without Non Alcoholic Steatohepatitis (NASH)[18].Similarly, in our study, no significant correlation was noted between means of ALT and AST with age, family history of diabetes, mode of therapy or type of diabetes. Mean ALT had no correlation with sex of the population. However, AST was found to be significantly correlated with male sex. Values of ALT and AST were also significantly higher with increasing BMI. A large cohort study done in India reported the presence of fatty infiltration of liver in ultrasonography in 62.25% (127 out of 204 diabetes patients)[18]. Our study revealed presence of fatty liver in 16 % of diabetes patients on ultrasound scan.Raised liver enzymes can be a marker of steatohepatitis in diabetes patients. Nevertheless, evidence fails to show significant positive correlation between liver histology and biochemical derangement[8, 18]. Advanced degree of NASH and fibrosis can occur in diabetic patients without significant liver function abnormalities[18].In the present study, means of ALT and AST were significantly correlated with hepatomegaly, increased liver echo and presence of fatty liver on ultrasound imaging. This might be due to the presence of non alcoholic steatohepatits in these patients. However, exact confirmation will require histological examination which is invasive. Larger studies are recommended in future to find out the exact association between the biochemical and histological changes of liver in diabetes patients without chronic liver pathology in Myanmar.
5. Conclusions
- Based on the findings of this study, raised ALT and AST are more common among the diabetes patients with higher BMI. AST elevation was also significant among men. Derangement of liver enzymes correlated statistically significantly with fatty liver on ultrasound. Therefore, abnormal liver function tests among diabetes patients can be indicator of associated non alcoholic fatty liver disease. Thus, checking for liver enzymes, ALT and AST, should be carried out to screen the possibility of underlying fatty liver, which might need further evaluation and early intervention to prevent from progression into cirrhosis and chronic liver disease, especially in male patients with high BMI.
ACKNOWLEDGEMENTS
- We are much grateful to all the patients who had voluntarily participated in this study as well as the staffs from the Pathology and Radiology department of Yangon General Hospital for their utmost contribution in completing this study. Our special thanks go to Professor Nyunt Thein, Professor Myint Han, Professor Tint Swe Latt and Professor Khin Maung Win from Yangon General Hospital for their encouragement, continuous support and guidance in undertaking this work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML