-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Database Theory and Application
2012; 1(2): 8-12
doi: 10.5923/j.database.20120102.01
Building a Spatial Information System for Cancer Patients' Registry in Egypt
Sayed M. E. Abdel-Wahab , Christina Albert Rayed
Computer and Information System dept, Sadat Academy for Management Science,Cairo, Egypt
Correspondence to: Sayed M. E. Abdel-Wahab , Computer and Information System dept, Sadat Academy for Management Science,Cairo, Egypt.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
A cancer registry is an important program component for the evaluation of cancer care. Accurate and timely collection of cancer patient data with appropriate follow-up is required by the Commission on Cancer. electronic medical information system (EMIS) and medical database (MDB) as basises for health service planning and resource allocation are vital importance in settings with limitted resources. Whether the data is collected on paper or electronically does not matter at the end important is the involvment of the staff responsible for its collection and the tangible benefits for the health professionals. This paper present Spatial Information System (SIS) for cancer patients' registry in Egypt which will be very important from the reference and legal point of views for the consultant and administration and also will play vital role in treatment, follow up, medical researches and statistical reports in hospitals.
Keywords: Electronic Medical Information System (EMIS), Electronic Medical Record (EMR)And Medical Database (MDB), Spatial Information System (SIS)
Cite this paper: Sayed M. E. Abdel-Wahab , Christina Albert Rayed , "Building a Spatial Information System for Cancer Patients' Registry in Egypt", American Journal of Database Theory and Application, Vol. 1 No. 2, 2012, pp. 8-12. doi: 10.5923/j.database.20120102.01.
Article Outline
1. Introduction
- Electronic information systems now permeate the world of healthcare. In the early days of their implementation considerable care was taken in checking the accuracy of the information they provided. As time has moved on all information systems have become more trusted and those operating in eHealth are no different. However, in this regard, and with the increasing amount of critical and sensitive information that they hold they are as important to patient safety as an item of medical equipment. Integrating the Healthcare Enterprise (IHE) is an initiative designed to stimulate the integration of the information systems that support modern healthcare institutions. IHE initiative recommends the use of existing standards[1] .A cancer registry is an important program component for the evaluation of cancer care. Accurate and timely collection of cancer patient data with appropriate follow-up is required by the Cancer centers. The cancer registry contributes to administrative and programmatic planning, patient treatment planning, research, staging, and continuity of care through data retrieval and monitoring of outcomes through annual analysis, and long-term follow-up [2].In all registries, a permanent record needs to be kept for each individual. This is because information regarding the diagnosis of a patient is usually drawn from diverse sources for example, hospital records, pathology, X-ray and death notifications. As registries usually need to count incident cases, information from these sources needs to be compiled so that each new case is not counted more than once. Information communication technology (ICT) has had a dramatic impact on our daily lives in recent years, benefiting many areas of the public health including health care delivery, surveillance, research and education. ICT provides more convenient ways to accomplish daily tasks and diminishes the impact of long distances in both personal and business interactions [3].Interaction between patients and physicians through the use of electronic tools for health-related purposes has been broadly defined as “e-Health” [4].E-Health activities are becoming quite common in our society and using the latest ICT have the potential to transform the health care delivery systems both in advanced and emerging nations by meeting the needs of citizens, patients, healthcare professionals, providers, and policy makers [5].There are many types of Registries; Diagnosis specific based registries (e.g. laboratory based disease registries) record all new cases of disease diagnosed via a specific diagnostic technique. Such registries are limited by the accuracy of the tests used, and provide minimal incidence rates. While the diagnosis of the condition may be ‘accurate’, many patients (rural, poor) may not have access to these diagnostic tests, and thus incidence patterns can be distorted. Hospital based registries record all cases admitted in a particular hospital irrespective of method of diagnosis. The advantage of these registries is that they provide a complete record of conditions diagnosed and listings of patients for further research into treatment effectiveness as well as facility planning. The main disadvantage of hospital based registries is that incidence rates cannot be calculated since the background population size from which the cases were drawn is not known. Consequently, the real needs of a community cannot be inferred and moreover, this type of registry may be biased by specialist interest in a particular condition or, specialist interest in favor of stages of particular conditions. Population based registries record all cases, irrespective of method of diagnosis from a population residing in a defined well-enumerated area. Data from these can be used to calculate disease incidence (i.e. the true burden of disease) without bias, and hence measure geographical variation, survival, unmet need and cost effectiveness of interventions.
2. Objectives of Cancer Patients' Registry
- Cancer patients registry are essential for assessing the extent of cancer burden in a specified geographic area. The primary objective of the cancer patients registry is to provide a large database to study cancer patterns and trends to monitor differences in cancer risks among different populations. Information about cancer incidence and survival is generated by the cancer patients registry. The information is used for descriptive and analytic epidemiological studies to: identify risk factors for the cancer; plan, monitor and evaluate a broad range of cancer control programs (e.g., screening); and, conduct research in health services and economics. Cancer patients registry is to produce standardized and comparable cancer incidence data for each newly diagnosed primary site of cancer. The cancer patients registry is a patient-based system, in which are recorded the kind and number (incidence) of primary cancers diagnosed for each person over a number of years until death. New primary cancers occurring for previous cancer patients are identified. The patient data is regularly linked to mortality data so that the date and cause of death of every cancer patient is eventually known [6].Cancer Patient Registry also plays an important role in research to identify the causes of cancer. Researchers often use the data collected by the cancer registry to identify cancer patients who could be interviewed about possible exposures they had before they were diagnosed with cancer. These can be compared to interviews among people without cancer to determine if cancer patients had different exposures. Researchers can also use registry data to determine if groups of people with specific exposures, such as those who work in a particular occupation or with a particular substance, are more likely to develop cancer than people who do not have these exposures. In addition to the data in the cancer patients registry may be used in a variety of research projects. Such uses might include survival statistics, epidemiological studies, planning of services, or controlling the disease and assessing the effects of intervention.A Global Observatory for e-Health dedicated to understanding the e-Health domain, its growth, evolution, and impact on health systems in all countries has been developed by the World Health organization [7]. Moreover, the European Community considers as a priority action “initiative on telemedicine (TM) for chronic disease management as home health monitoring” and the future “vision for Europe 2020” is based on development of “integrated Telemedicine Services” [8]. Cancer Program may decrease the morbidity and mortality of patients with cancer and improve the quality of care. The Cancer Program may provide educational needs for public and healthcare professionals about specific malignancies. The Cancer Program may maintain a supportive care system for all cancer patients, and ensures availability of consultation and rehabilitation. Reports on incidence and mortality from cancer may publish regularly. Occasional reports may include analyses of trends, variation according to country of birth or geographical area and reviews of specific cancers [9].The Cancer Registry is composed of certified personnel who operate a computerized registry, and fulfil the requirements including annual follow-up on all appropriate cases. The Cancer Registry’s statistical reports are available upon request by all staff physicians and allied health professionals as needed for research or education purposes. Cancer Registry staff are responsible for creating and publishing the annual report for statistical analysis of the Cancer Program as required [10].Information on the register is used to:• to determine the incidence of cancer with respect to geographic, demographic, and social characteristics • to monitor trends and patterns of cancer incidence over time • to identify high risk populations • monitor the number of new cases and deaths from cancer population • compare local and national trends in cancer • assist in planning services for the control of cancer and the care of cancer patients • monitor and evaluate the quality of cancer treatment, the outcomes of cancer care and the performance of cancer control programs • to provide a database and serve as a resource in conducting epidemiologic studies • to provide data to assist public health officials, hospital administrators, and physicians to effectively plan services, prioritize health resource allocations and develop and measure prevention and intervention strategies • develop education programs for schools and outside workers • provide background data for research assist with studies to determine the causes of cancer and to improve the quality of cancer services • contribute to national monitoring of cancer cases and cancer deaths.
3. Cancer Patients' Registry System in Egypt
- In Egypt, attempts to have a cancer registry date to the late sixties of the past century with the recognition of oncology as a separate discipline. There are two types of cancer registries: Hospital-based and Population based. Hospital-based registries collect information on cancers reported in a given hospital, regardless of where that person with cancer resides. They help in assessing cancer patient care in a given hospital and aid in hospital administration including cancer control programs. Population-based cancer registries collect information on all new cancer cases reported from the population residing in a defined geographic area. The period of residence in the geographic area is usually for a minimum of one year at the time of diagnosis of cancer. Population-based cancer registries are concerned with providing information on cancer incidence trends over time and constitute a base for carrying out research studies on cancer etiology through epidemiological studies. They provide reliable data on the magnitude of the cancer problem and about the pattern of cancer and its types and changes that might occur over time.National Cancer Institute, Cairo that started its activities in 1970. The first initiative was the establishment of the Alexandria Cancer Registry that was followed by the registry of the National Cancer Institute in Cairo. This pioneer registry was initiated in the High Institute of Medical Research, Alexandria University. The far sight of establishing the registry as a recognized activity of the institute and covered by its budget, and not as a research project. The registry is still ongoing as a regional hospital-based cancer registry for Alexandria. The institute started a project for registration of cancer in hospitals of the Metropolitan Cairo Area that had an off-spring in the Governorate of Fayoum. In addition to these registries, there are medical records rooms in different institutions dealing with cancer cases with variable degrees of sophistication. All these attempts to register cancer are hospital-based. The only existing population-based cancer registry is that in Gharbiah, established in 1998[11].With the spread of oncology facilities all over the country, a large number of medical records rooms became available with variable degrees of perfection and sophistication. The largest of these hospital-based registries is that of Nasser Institute. It is a multi-institutional registry that collects data of the 8 cancer centers of the Ministry of Health and Population using standardized formats compatible with that of MECC. It is hoped that this registry will eventually develop into a set of population-based cancer registries using Gharbiah experience as a model.Many patient record systems that exist today contain mostly unstructured text – the text valuable in different circumstances of patient care. To extract information from the record relevant for decisions that appear consumes time and because physicians work under severe time constraints, they have little time left to search for this information. Although, clinicians benefit from efficiency gains of the computerized patient record system, efficiency gains are not enough. A record system should also support physicians in getting overview of and access to information in the record.Below, we look at some limitations of an existing electronic patient record system in order to come up with some requirements for improving a future electronic medical record system:1. The text can be characterized as rich and extensive in words. Usually, the record contains several pages of text. Many implementations of patient systems have time orientation - recording events in order of appearance. Information is, more or less, only accessible to the author, or information owner, who knows where to search.2. The patient record is built around a principal free-text area to document patients' complaints, symptoms, signs, clinical findings, diagnoses, prescriptions of medication, laboratory tests, and other information pertinent to the specific medical problem at hand. The free-text area contains a lot of information, but with very limited possibilities to extract parts of it. Typically, physicians themselves enter information into the patient record system during patient care. Therefore, we consider physicians as both information owner and information user, thus, simplifying issues related to security and privacy of information. 3. The record system offers separate windows to document patients' family and social history but to record this information requires extra effort in moving away from the main record. Physicians tend to integrate family and social history into the free-text area relevant for the medical problem being treated at the time of writing. The record system structure appears as rigid and seems to force physicians to work in non-optimal ways.4. Interleaving medical problems impede overview and, thereby, also continuity of care. A chronological record mixes descriptions of different medical problems. The process of getting an overview of previous history of a medical problem or to view simultaneously documents related to a specific problem either consumes time or does not exist. Due to lack of overview and continuity of care, the record contains both redundant and confusing information, complicating work with the patient record unnecessarily5. There are some redundancy data like giving code for sex and also entering sex in text.6. Some cancer registry did not make a code for some patients data.7. Data in text form there are some errors in typing like in patients areas or streets names. 8. Some errors like reversing patient street name and area name or putting home number beside street name.We relate requirements for a problem-oriented electronic medical record to some of the limitations listed in previous section:1. Patient record system should present levels of relevant information.2. Patient record system should also provide physicians flexibility when working with record information for add, update and delete. 3. Patient record system should not force physicians to work in formal ways.4. System should present statistical data in a report form for different sides.
4. Case Study: Spatial Information System for Medical Records for Cancer Patients' Registry in Egypt
- Cancer patient medical record system will design to become more complete, rigorous, and systematic in documenting clinical information. These case sheets and files are very important from the reference and legal point of views for the consultant and administration and also play vital role in treatment, follow up, medical researches and statistical reports in hospitals. The objectives of electronic medical record system:1. Offer new methods of storing, manipulating and communicating medical information of all kinds, which are more powerful and flexible than paper based systems.2. Analyze the impact of computer-based medical record systems on medical practice, quality of care, and user and patient satisfaction.3. Find out the pattern for admission at National Cancer Institute (NCI) and some public hospitals.4. Provide The availability of using electronic medical record system in different places in hospitals like outpatients clinics, inpatient, X-rays, diagnostic aids, emergency and so on.5. Identify the possible reasons for non-availability of case sheets.6. Develop a patient medical record system to make availability of all the case sheets.7. Observe the effect statistical reports which will create from electronic medical record system.Potential users of electronic medical record system include:• Patients• Doctors• Nurses• Managers• Pharmacists• Doctors’ support staff such as secretaries or receptionists happy• Dispensing assistants• National health organizations• Insurance companies or other reimbursement agencies• Researchers• Drug companiesThe proposed Spatial Information System for Medical records for cancer patients' registry divided into five classes as following personal class, demographic class, spatial class, pathologic class, and Clinical class. In each class there are some data core “C”, required “R”, and optional “O”.
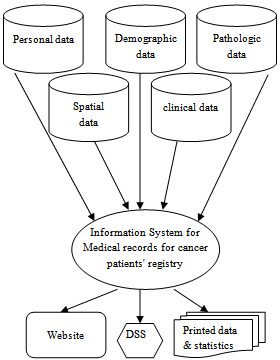 | Figure 1. proposed Spatial Information System for cancer patients' registry |
5. Conclusions
- It is becoming clear that developments in the electronic medical record systems are set to increase significantly in the near future. From the Previous studies in cancer registry international or national as discussed. This paper suggests a proposed Electronic medical record (EMR) for cancer patients' registry in Egypt. This Electronic medical record (EMR) is a data collection system that tracks cancer cases that have been diagnosed or treated in a specific institution or geographic area. Cancer registries typically collect information from medical records provided by hospitals, and other care facilities.We look at some limitations of an existing electronic medical record (EMR)in order to come up with some requirements for improving a future Spatial Information System for cancer patients' registry in Egypt. So that the objectives of proposed Spatial Information System for Medical records are Offering new methods of storing, manipulating and communicating medical information of all kinds, which are more powerful and flexible than paper based systems, analyzing the impact of computer-based patient record systems on medical practice, quality of care, and user and patient satisfaction, finding out the pattern for admission at National Cancer Institute (NCI) and some public hospitals, Providing availability of using Spatial Information System for Medical records in different places in hospitals like outpatients clinics, inpatient, X-rays, diagnostic aids, emergency, and observing the effect statistical reports .
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML