-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Clinical Practice
p-ISSN: 2326-1463 e-ISSN: 2326-1471
2019; 8(1): 1-9
doi:10.5923/j.cp.20190801.01

Administration of Ephedrine versus Norepinephrine for Management of Post-Spinal Hypotension during Lower Limb Orthopedic Surgery
Amira Abo Elnasr Awad
Lecturer of Anesthesia and Intensive Care, Department of Anesthesia and Intensive Care, Faculty of Medicine for Girls, Al-Azhar University, Egypt
Correspondence to: Amira Abo Elnasr Awad, Lecturer of Anesthesia and Intensive Care, Department of Anesthesia and Intensive Care, Faculty of Medicine for Girls, Al-Azhar University, Egypt.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Neuraxial anaesthesia technique induce vasodilation, this may result in hypotension requiring the administration of vasopressors drugs. The present study was conducted to compare the effects of intermittent I.V. boluses of ephedrine (EPH) and norepinephrine (NE) on maintain arterial blood pressure in patients undergoing lower limb orthopedic surgery during spinal. Aim: To compare the efficacy and safety of intermittent boluses administration of ephedrine (EPH) versus norepinephrine (NE) for treatment of hypotension patients during spinal anesthesia for patients undergoing lower limb orthopedic surgery. Patients and methods: A randomized, double-blinded study was carried out on 100 patients ASA I or II undergoing lower limb orthopedic surgery. The patients were divided into two groups of 50 patients, the ephedrine group (EPH group): received 5 mg intravenously bolus (IV) and the norepinephrine group (NE group): received 5μg intravenously bolus (IV) when hypotension occurred (systolic blood pressure decrease by 20% or more from baseline). Systolic blood pressure (SBP), mean arterial blood pressure (MAP) and heart rate (HR) were recorded at baseline (before spinal anasethesia) and after initiation of spinal anaesthesia at 3, 6, 9, 12, 15 minutes then every 5mins were measured for 30 mins then every 15 minutes up to end of surgery. The number of boluses of vasopressors, incidence of bradycardia, tachycardia and hypertension episodes were recorded. Also incidence of side effects during surgery were recorded. Results: There was no significant difference in SBP and MAP between both groups in all times P<0.05 however, the rise in heart rates were significant higher in group EPH than group NA at 6, 9, 12 mins (p <0.001) but bradycardia was not significantly different between the two groups P<0.05. The number of boluses of vasopressors required to maintain systolic blood pressure were lower in NE group 29/ 45 patients (64.4%) than EPH group 24/ 45 patients (53.3%). The incidence of hypertension and bradycardia were not significantly different between the two groups however tachycardia were significantly higher (P < 0.01) in group EPH. There was no significant difference in side effects during surgery between both groups. Conclusions: Norepinephrine is potent drug can be used as an alternative vasopressor for maintainance of blood pressure during post-spinal hypotension.
Keywords: Spinal Anaesthesia, Hypotension, Ephedrine, Norepinephrine, Lower Limb Orthopedic Surgeries
Cite this paper: Amira Abo Elnasr Awad, Administration of Ephedrine versus Norepinephrine for Management of Post-Spinal Hypotension during Lower Limb Orthopedic Surgery, Clinical Practice, Vol. 8 No. 1, 2019, pp. 1-9. doi: 10.5923/j.cp.20190801.01.
Article Outline
1. Introduction
- Spinal anesthesia is one of the oldest and most reliable techniques in anesthesia today. It produces sympathetic block, sensory analgesia and motor block, depending on dose, concentration, or volumes of local anesthetics. Spinal anesthesia is often used for lower limb orthopedic surgery. Because of its rapid onset, negligible failure rates and cost effectiveness. In addition, decreases intra-operative blood loss, decrease the incidence of postoperative thromboembolic and pulmonary aspiration events [1].Regional anesthesia has been shown to have several advantages over general anesthesia but associated with a risk of severe and prolonged hypotension (33%) and bradycardia (13%) [2]. Hypotension during spinal anesthesia results principally from the preganglionic sympathetic blockade. Systemic vascular resistance decreases as a result of a reduction in sympathetic tone of the arterial circulation this leads to peripheral arterial vasodilatation, the extent of which depends on the number of spinal segments involved. Other theories are proposed to explain hypotension during spinal anesthesia, among them: 1) direct depressive circulatory effect of local anesthetics, 2) relative adrenal insufficiency, 3) skeletal muscle paralysis, 4) ascending medullary vasomotor block, and 5) concurrent mechanical respiratory insufficiency [3]. Loss of sympathetic input to the heart, leaving vagal parasympathetic innervations unopposed, and a decrease in cardiac preload are the main reasons for bradycardia during spinal anesthesia [4]. Therefore, systemic hypotension should be prevented or treated by preloading or coloading of IV fluid (electrolyte and/or colloid) which is first used to correct this hypotension, but is frequently not effective. Consequently, vasopressors are often required [5]. Ephedrine is the most commonly used vasopressor during anaesthesia. Ephedrine has direct effects on alpha and beta receptors (α, ß1 and ß2) and indirect effects by releasing endogenous norepinephrine from synaptic storage sites. It causes increase in systolic and diastolic blood pressure and heart rate and it improves preload via an increase in cardiac output and peripheral arteriolar vasoconstriction. However, ephedrine has several adverse effects; it causes tachycardia, arrhythmia, nausea and vomiting [6, 7]. Norepinephrine is a naturally occurring catecholamine. It stimulates the alpha and beta receptors in the sympathetic nervous system. It is direct-acting sympathomimetic producing profound alpha-adrenergic receptor activity and weak βadrenergic activity. Alpha receptors stimulation causes peripheral, renal, splanchnic and pulmonary vasoconstriction. Beta receptors (ß1 and ß2) stimulation increases myocardial contractility, with less tachycardia produced than with adrenaline. ß1 adrenergic effect is prominent in the lower dose range, while alpha adrenergic effects predominate at higher doses [8]. It may be a more suitable option for maintaining blood pressure with less negative effects on heart rate (HR) [9].
2. Patients and Methods
- One hundred patients with American Society of Anesthesiologists (ASA) physical status I or II aged between 18-65 years of both sex undergoing spinal anaesthesia for lower limb orthopedic surgeries in the Anaesthesia Department of Al-Zhraa University Hospital. In this randomized, double-blinded study, patients were randomized by using a computer generated randomization list; the study was approval from ethical committee, an informed consent obtained from all participants in this research. Patients divided into two groups: the ephedrine group (EPH group, n = 50) and the norepinephrine group (NE group, n = 50). The anesthesiologist was blind to vasopressor agent. The assigned drug was given via coded syringes, each of which contained the same volume. Vasopressor solution was freshly prepared before operation by an anesthesiologist who had no role in the study. Exclusion criteria: operation with sever blood loss, patients maintained on cardiovascular medications including calcium-channel blockers, angiotensin convertase inhibitors, β- or α-blocking agents, or α2-adreno-receptor agonists or any drugs that may alter normal response to study drugs, severe congestive heart failure, arrhythmia, contraindications to spinal anesthesia such as pre-existing neurological disease, bleeding disorder, patient on anticoagulant treatment, infection at site of injection and history of allergy to local anesthetics or allergic to any drug used in the study.
2.1. Preoperative Management
- All the patients had the inclusion criteria were assessed before the day of surgery with history, clinical examination, routine laboratory investigation (complete blood count, liver function, renal function and coagulation profile). All patients in the preoperative unit were monitored (non-invasive blood pressure, heart rate and peripheral oxygen saturation) these values were recorded as baseline values. Intravenous access obtained with a peripheral 18-G cannula, patients were preloaded with normal saline (NS) 10 ml/kg 20 minutes before the spinal anesthesia. In operating room, continuous standard monitoring equipment was connected to patients till the end of surgery (pulse oximetry, electrocardiogram and non-invasive blood pressure). Subarachnoid block was done with the patient in sitting position, the patient sit on the edge of the operating table with legs on stool, leaning forward arching his back. Under complete aseptic condition, iliac crest was palpated and thumb extended to meet the midline, feeling the space between the choice of median or lateral access at level of L3/4 or L4/5 was made by the anesthesiologist depended on the anatomy of the patient, the subcutaneous tissues and muscles were infiltrated with 3 ml of lidocaine 2%, with 25 or 22 G spinal needle was placed intrathecal (Quincke needle, Becton Dicknson, Spain), to get a free flow of CSF. 2.5-3 ml of 0.5% hyperbaric bupivacaine (Anawin – Neon labs) plus 25μg fentanyl were injected intrathecally, Thereafter, patients were immediately turned to supine position. The sensory and motor block was evaluated by sense of coldness and the Modified Bromage Scale (0 = no motor block, 1 = inability to raise extended leg, 2 =inability to flex the knee and 3 = inability to flex the ankle and foot), respectively within 5 min of intrathecal injection. The failure of spinal anesthesia was recorded and excluded from the study. In patients who developed hypotension, which defined as a decrease in systolic arterial blood pressure (SBP) by 20% or less from baseline after spinal block. All the patients were randomized into ephedrine group and norepinephrine group. Vasopressor prepared in identical syringes before operation by (anesthesia resident) who had no rule in the study, the intraoperative monitoring was done by the same anesthesiologist who will be administering the drug but unaware of the content of the syringes.Ephedrine group (EPH group): Patients in the ephedrine group received i.v. bolus 5 mg (used ephedrine 25 mg / ml ampoule, ephedrine sulphate MISR CO. Egypt) dilute 1 mL of it with saline 0.9% solution to a 5ml syringe produce a concentration of (5mg/mL)). After spinal anesthesia whenever systolic blood pressure (SBP) dropped by 20% from baseline value, patients were received rescue boluses Norepinephrine group (NE group) Patients in the norepinephrine group received an i.v. bolus 5 μg (used norepinephrine ampoule 8mg/4ml, norepinephrine bitartrate Egypharma Alex. CO. For Egypharma ampoule) can easily prepared by take 1ml of (equal to 2000 μg) diluting or adding it to solution of 500 ml of 5% dextrose solution bag was discarded 100ml; leaving 400 ml of it, obtaining a concentration of 5μg / ml then 5 ml from this glucose bag was taken in a 5ml syringe (5μg/ml). Patients were received rescue boluses whenever hypotension occurred this dose was chosen based on previous studies [10, 11]. Haemodynamic data (SBP, MAP and HR) were recorded before spinal anasethesia (baseline) and at 3,6,9,12,15 minutes after initiation of spinal anaesthesia then every 5 min up on 30 minutes finally every 15 minutes till end of surgery. If patients developed bradycardia, patients was managed by 0.3 mg of atropine. The frequency of hypotension (SBP < 20% or less from baseline), hypertension episodes (SBP > 20% from baseline or more), tachycardia episodes (HR >100 beats/min) and bradycardia episodes (HR < 60 beats/min), the number of boluses of vasopressors and vasopressor consumption used in each group were recorded. The incidence of nausea, vomiting, shivering, restlessness, headache, and pruritus were recorded as well.
2.2. Sample Size
- The sample size was calculated from a known total population of 100 patients by adjusting the power of the test to 80%, the confidence interval to 95% and the margin of error accepted 5%. So the sample size was found to be 90 patients divided into two equal groups.
2.3. Statistical Analysis
- Data were collected, revised, coded and entered to the statistical package for Statistical Package for social science (IBM SPSS) version 22 (V. 22.0, 2013; IBM Corp., New York, USA). The distribution of quantitative data was tested by Kolmogorov-Smirnov test of normality. So, the quantitative data were presented as mean, standard deviations and ranges when parametric. Also qualitative variables were presented as number and percentages. The comparison between groups regarding qualitative data was done by using Chi-square test and/or Fisher exact test when the expected count in any cell found less than 5.The comparison between two independent groups with quantitative data and parametric distribution was done by using Independent t-test. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant at the level of < 0.05.
3. Results
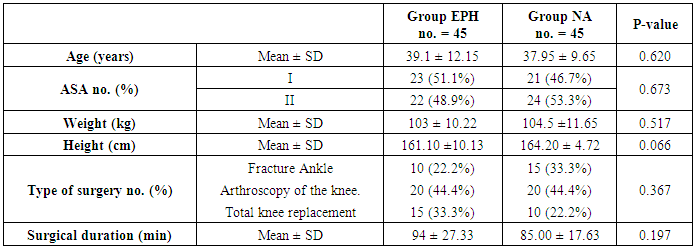
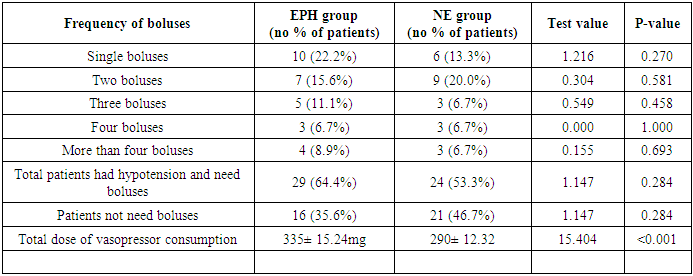
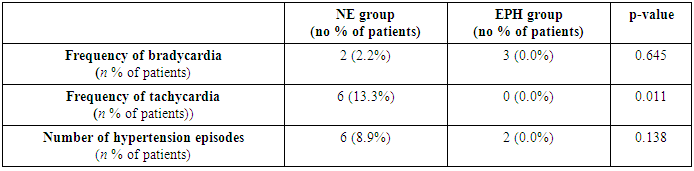
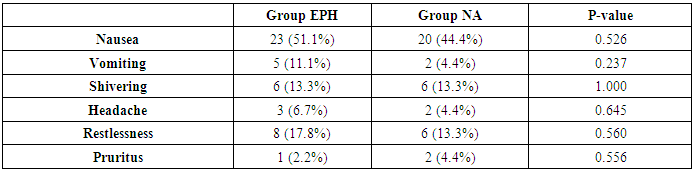
- One hundred patients scheduled for orthopedic lower limb surgeries that fulfilling the inclusion criteria were enrolled in this study. They were divided randomly into two groups of 50 patients in each, EPH group (Ephedrine group) and NE group (norepinephrine group). Ten patients were excluded from the study: four patients needed to change into general anaesthesia, three patients had sever vasovagal during initiation of spinal anaesthesia and were given atropine and or vasopressor, three patients did not receive the drugs because failed spinal anaesthesia. Demographic data (age, weight, height, ASA, duration of surgery and type of surgery) were comparable in both groups and not statistically significant. (table 1). As regarded haemodynamic characteristics, there were significantly higher heart rate (tachycardia HR > 100 beats/min) in EPH group especially recorded at 6, 9, 12 mints (P < 0.001) compared with NE group but at other times intervals the differences observed between two groups were statistically insignificant (figure 1). The incidence of bradycardia (HR< 60 beats/min) were not significantly different between the two groups (three patients were bradycardia in NE group and two patients in the EPH group and were given atropine 0.3 mg for only once and then the patient's heart rate recovered to normal). There were no significant differences between the two groups in SBP and MAP all over the time intervals of the study (figure 2, 3). Hypotension episodes were observed in 29 patients at ephedrine group (64.4%) compared to 24 patients in norepinephrine group (54.3%) without significant difference. The total dose of drugs consumsion in each group was significantly lower in NE group (290 ± 12.32ug) compared with ephedrine group (320 ± 15.24 mg) (table 2). Ephedrine administration caused more incidence of tachycardia (P = 0.011) and hypertension (P =0.138) episodes than norepinephrine and were significantly higher in tachycardia. (Table 3). The incidence of nausea, vomiting, shivering, headache, restlessness and pruritus were comparable and no statistically significant differences were detected between the studied groups P < 0.05 (Table 4).
|
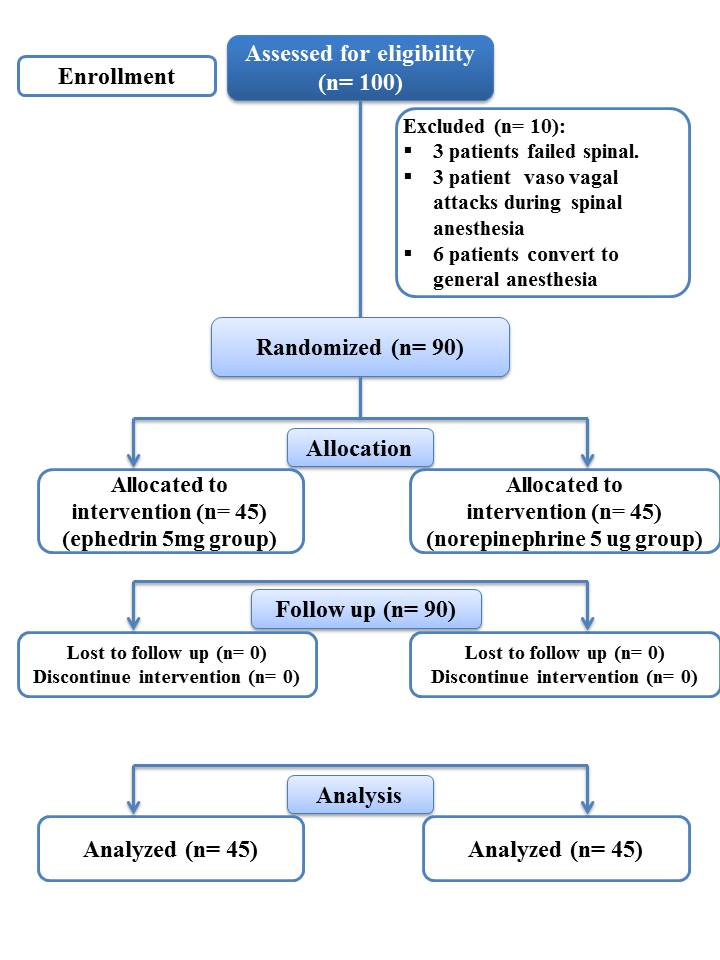 | Figure (1). Flow chart of the patients enrolled in the study |
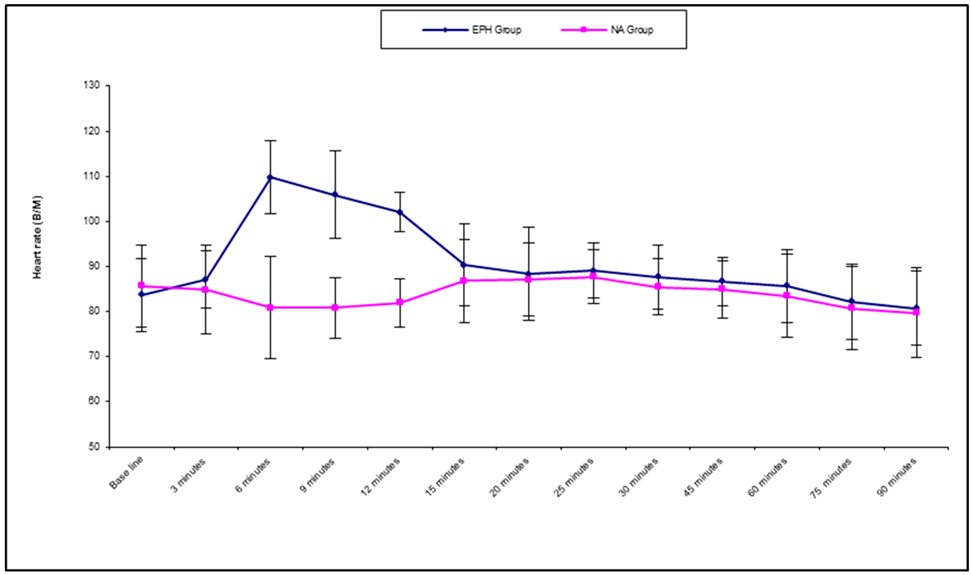 | Figure (2). Heart rate changes between the two groups (beat/min) |
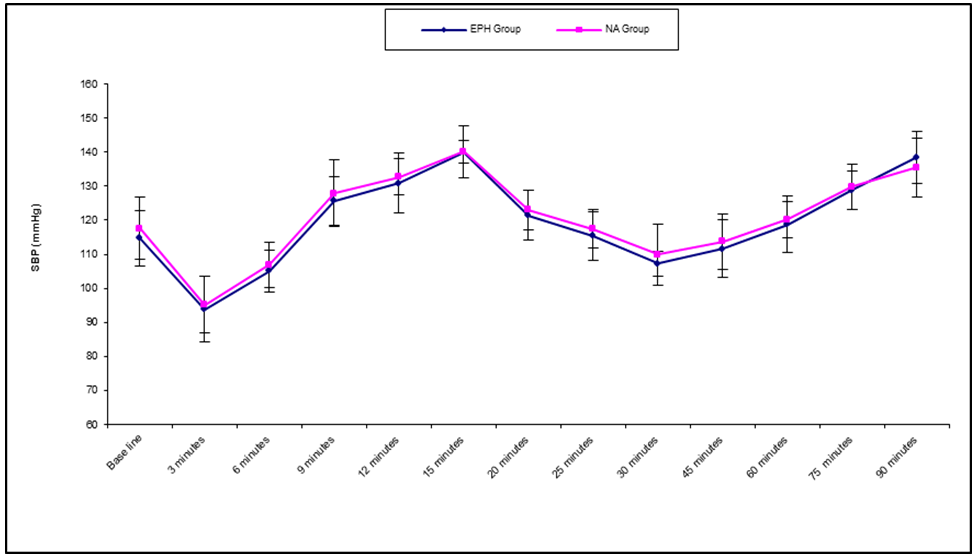 | Figure (3). Systolic blood pressure changes between the two groups |
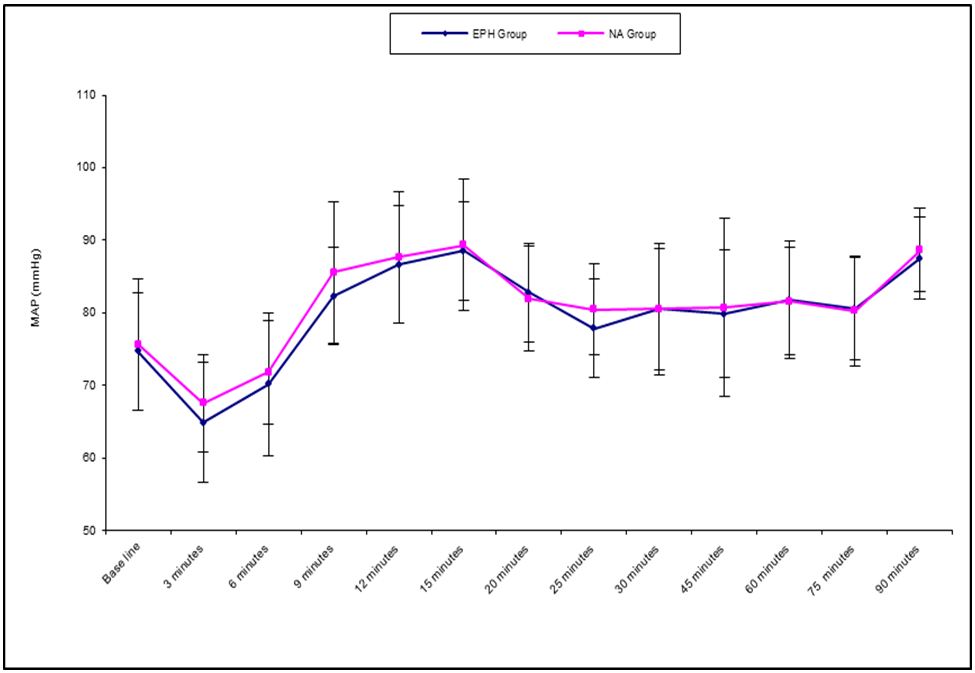 | Figure (4). Mean arterial blood pressure changes between the two groups |
|
|
|
4. Discussion
- Subarachnoid block is a commonly employed anaesthetic technique for performing lower limb orthopedic surgeries. It is a safe, simple, inexpensive, easy-to-administer technique and has rapid onset and is reliable. This technique also offers a high level of post–anaesthesia satisfaction for patients despite the clinical benefits of spinal anaesthesia there is a major threat of hypotension following its administration and requiring vasopressors therapy for maintenance of blood pressure. This study, evaluated the effect of the administration of intermittent i.v. boluses of ephedrine versus norepinephrine to maintain the SBP within 20% of the baseline values during the hypotensive effect of spinal anesthesia in lower limb orthopedic surgery. This administration does not require an infusion pump, so it is easy to perform clinically. Ephedrine has sympathomimetic effect with a direct α and β- receptor agonist and an indirect mechanism of action (release of norepinephrine) causing an increase in myocardial contractility, HR and cardiac output. Norepinephrine, has a strong α-adrenergic effect and only a mild β-adrenergic effect, is often used to treat anesthesia-induced vasodilatation by increasing systemic vascular resistance). The results of current study showed that both drugs had similar efficacy for maintaining blood pressure during spinal anesthesia. SBP and MAP were comparable in both groups but the number of boluses of vasopressors used during spinal anesthesia were higher in ephedrine group. Norepinephrine produced a better hemodynamic stability compared with ephedrine by maintaining stable blood pressure and HR.These results are consistent with the results of El Shafei et al. [12] who compared norepinephrine with ephedrine to prevent spinal induced hypotension in coronary artery disease in patients undergoing knee arthroscopy. Patients were randomly allocated to two groups receive either 5 mg of ephedrine or 5ug of norepinephrine when hypotension occurs. They found that norepinephrine is more effective compared with ephedrine in the maintenance of SBP with significant tachycardia (P < 0.0001) in EPH group. However, they found no significantly difference between the two groups regarding the incidence of hypotension, hypertension, and bradycardia, and not recorded nausea, vomiting, or shivering. They go with study although present study was found significantly lower numbers of hypotension and hypertension episodes and less tachycardia in the patients treated with norepinephrine. The current study in agreement with the some results of Elnabtity and Selim [13] who compared intravenous a prophylactic bolus of norepinephrine 5ug at the time of intrathecal block, plus rescue boluses of 5ug norepinephrine and a prophylactic bolus of ephedrine10 mg i.v. at the time of intrathecal block, plus rescue boluses of 10 mg ephedrine, to treat hypotensive effect of spinal anesthesia during cesarean delivery. The numbers of hypotension and hypertension episodes and the frequency of bradycardia and tachycardia were significantly lower in group N compared with group E (P = 0.02, 0.003 and 0.008, respectively). Furthermore, the number of boluses of vasopressors were also lower in group NA. The frequency of bradycardia was significantly lower in group norepinephrine, this against current study which reported frequency of bradycardia insignificant in EPH group, the incidence of maternal side effects during the operation (nausea, vomiting, shivering, headache, restlessness, and pruritus) were comparable and not significant between both groups.Present study is not consistent with the work of many researchers whom studied on norepinephrine for prevention of hypotension during spinal block for cesarean section and used different doses or different regimen of administration. like Onwochei et al. [14] who studied the effect of different intermittent i.v. boluses of norepinephrine of either 3, 4, 5, 6, 7, or 8 µg when (SBP) fell below 100% of baseline to prevent hypotension during spinal. The results were the norepinephrine maintain SBP at or above 80% of baseline, from induction of spinal anesthesia to delivery of the fetus and were not associated with significant maternal or fetal adverse effects and Ngan Kee et al. [15] who used a manually adjusted norepinephrine infusion that ranged between 1.25 μg/min and 5 μg/ min. They reported a lower incidence of post-spinal hypotension in the norepinephrine group compared with the control group. Daili Chen et al. [16] they used three different infusion norepinephrine dosing regimens for preventing spinal hypotension, the infusion dosage regimens were 5, 10, and 15 g/kg/h, respectively compared with the control group (patients received saline infusion). Norepinephrine infusion groups of 5μg/kg/h and10 g/kg/h were effective to reduce hypotension without significant adverse effects on patients, but highest dose (15μg/kg/h) experienced more hypertension episodes. There were no significant differences among groups in HR, CO (cardic output), systemic vascular resistance (systemic vascular resistance), maternal adverse effects. Hasanin et al. [17] who were randomized the patients into three groups, received norepinephrine with starting infusion rates of 0.025 μg/ kg/ min, 0.050 μg/ kg /min, and 0.075 μg/kg/ min to reduce post-spinal hypotension (SBP below 80% of the baseline), Infusion was stopped when intraoperative hypertension occurred. Both of the 0.050μg/ kg /min and 0.075 μg/kg/ min of infusion rates effectively reduced hypotension compared with the 0.025μg/kg/ min. Many studies not coincide with current study as compared norepinephrine with phenylephrine for maintaining blood pressure during hypotension after subarachnoid block in cesarean sections. Dongl et al. [18] they compared of prophylactic bolus norepinephrine (10 μg) and phenylephrine (50 μg) on hypotension immediately after spinal anesthesia. They reported that norepinephrine is effective as phenylephrine in preventing spinal hypotension but has less adverse effects on heart rate and cardiac output than phenylephrine. Sharkey et al. [19] compared of intermittent intravenous boluses of phenylephrine with norepinephrine to treat spinal-induced hypotension. Patients receive either PE 100 µg or NE 6 µg when SBP was below 80% of baseline. In addition, ephedrine was given intravenously to both groups if SBP was <80% of baseline for 2 consecutive readings. patients requiring rescue boluses of ephedrine was lower in the NE group compared to the PE group, the patients in the PE group had a higher risk of bradycardia episodes compared to the NE group. Also study of Ngan Kee et al. [20] were done on healthy patients having cesarean delivery under spinal anesthesia were randomized patients with a computer-controlled infusion of norepinephrine 5 μg/ml or phenylephrine 100 μg/ml. they showed that norepinephrine produced greater HR and CO with similar efficacy for maintaining SBP compared with phenylephrine. Study of Vallejo et al. [21] they compared phenylephrine (0.1μg/kg/min) with norepinephrine (0.05μg/kg/min) at fixed-rate infusions in preventing hypotension in spinal anesthesia; patients who required rescue vasopressor boluses were similar between groups. Haemodynamic parameters including HR, SBP, CO, SVR, cardiac index and stroke volume, were similar in both group. Poterman et al. [22] were done on patients under balanced propofol/remifentanil anaesthesia, phenylephrine and norepinephrine produced similar clinical effects when used to counteract anaesthesia-induced hypotension. They were found phenylephrine 100 μg/min and norepinephrine 10 μg/min caused an equivalent increase in MAP, stroke volume (SV), combined with a significant equivalent decrease in HR , cardiac index (CI) , cerebral tissue oxygenation (SctO2) and unchanged RPP (rate-pressure product). Many researchers against this study whom compared ephedrine with phenylephrine for treatment of spinal-induced hypotension, like study of Naghibi et al. [23] who compared intravenous ephedrine with phenylephrine, for post-spinal hypotension during elective lower abdominal surgery, following spinal block, patients received a 1 mL bolus of (ephedrine 2.5 mg or phenyephrine 25 mcg or placebo) and another 5 mg bolus of ephedrine if the blood pressure below 10% of baseline and repeated as necessary. there was no significant difference between ephedrine and phenylephrine in prevention of hypotension and was a higher incidence of bradycardia in patients receiving phenylephrine than ephedrine or placebo in the range of doses that have been studied and Gunda et al. [24] who compared the effectiveness and the side effects of ephedrine, versus phenylephrine administered for management of post-spinal hypotension during cesarean section and they found no significant difference.Vakili et al. [25] Comparing intravenous phenylephrine and ephedrine for hypotension during spinal anesthesia for elective cesarean section patients were divided to 4 groups: group I received 5mg ephedrine bolus, group II received 10 mg bolus ephedrine, group III received phenylephrine bolus of 50 mcg, and group IV received 100 mcg phenylephrine bolus in case of hypotension. According to the results of the study in terms of the haemodynamic changes, the low-doses of these drugs could control systolic and diastolic blood pressure close to the patient’s baseline blood pressure. Increased SBP was greater at higher doses of both drugs and diastolic blood pressure had a significant difference among the 4 groups (P < 0.01) Heart rate had a significant difference between the 4 groups (P < 0.0001), HR in the ephedrine group was higher than the phenylephrine group. And study of Dalai et al. [26] conducted to compare the effects of prophylactic phenylephrine 100μg/ml/min and ephedrine infusion 8mg/ml/min on haemodynamics in caesarean section under spinal anaesthesia. The prophylactic phenylephrine infusion would maintain better maternal haemodynamics than ephedrine infusion.
5. Conclusions
- The current study concluded that norepinephrine is more effective than ephedrine in preventing and treatment spinal hypotension and has less adverse effects on HR in patients undergoing lower limb orthopedic surgeries.
Limitations
- This study had some limitations that did not use advanced haemodynamic monitors for cardiac output measurement. So we needs further work using different boluses doses of vasopressors under cardiac output measurement.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML